Myotubular/Centronuclear Myopathy and Central Core Disease
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Periodic Paralysis: a Case Report of Normokalemic Presentation in a Young Girl
Case Report ISSN: 2574 -1241 DOI: 10.26717/BJSTR.2021.35.005673 Periodic Paralysis: A Case Report of Normokalemic Presentation in a Young Girl Lucio Ceglie, Roberta Patacchiola, Daniela Iannucci, Miriana Guarino, Lorenzo Sansone, Maria Chiara Sgarrella, Francesco Chiarelli* and Annalisa Blasetti Department of Pediatrics, University of Chieti, Italy *Corresponding author: Francesco Chiarelli, Department of Pediatrics, University of Chieti, Italy ARTICLE INFO ABSTRACT Received: April 10, 2021 The skeletal muscle channelopathies represent a rare group of neuromuscular disorders which are caused by genetic mutations regarding voltage-gated ion Published: April 21, 2021 channels, which play an important role in muscle membrane depolarization. Muscle channelopathies are broadly divided into 2 main categories: nondystrophic myotonias (NDM) and periodic paralysis (PP). Periodic paralysis (PP) are rare autosomal dominant Citation: Lucio C, Roberta P, Daniela I, neuromuscular disorders, characterized clinically by periodic attacks of muscle weakness Miriana G, Francesco C, et al., Periodic in concomitance with serum potassium level alterations. It is possible to distinguish Paralysis: A Case Report of Normokalemic normokalemic, hyperkalemic and hypokalemic paralysis. PP is caused by genetic Presentation in a Young Girl. Biomed mutations in voltage-gate ion channels like sodium, potassium, and calcium channels, J Sci & Tech Res 35(2)-2021. BJSTR. which are determinant for muscle membrane depolarization. The most common genes MS.ID.005672. involved in pathogenesis are CACN1S, SCN4A and KCNJ2, encoding calcium, sodium, and potassium channels (Table 1). Moreover, paralysis related to serum potassium values Keywords: Hypokalemia; Periodic Paral- may also occur in thyreotoxicosis [1], Liddle syndrome, Gitelman syndrome, primary ysis; Transient Paralysis; Muscular Weak- hyperaldosteronism, and acid-base balance disorders. -

Centronuclear Myopathies Under Attack: a Plethora of Therapeutic Targets Hichem Tasfaout, Belinda Cowling, Jocelyn Laporte
CORE Metadata, citation and similar papers at core.ac.uk Provided by Archive Ouverte en Sciences de l'Information et de la Communication Centronuclear myopathies under attack: A plethora of therapeutic targets Hichem Tasfaout, Belinda Cowling, Jocelyn Laporte To cite this version: Hichem Tasfaout, Belinda Cowling, Jocelyn Laporte. Centronuclear myopathies under attack: A plethora of therapeutic targets. Journal of Neuromuscular Diseases, IOS Press, 2018, 5, pp.387 - 406. 10.3233/JND-180309. hal-02438924 HAL Id: hal-02438924 https://hal.archives-ouvertes.fr/hal-02438924 Submitted on 14 Jan 2020 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Journal of Neuromuscular Diseases 5 (2018) 387–406 387 DOI 10.3233/JND-180309 IOS Press Review Centronuclear myopathies under attack: A plethora of therapeutic targets Hichem Tasfaouta,b,c,d, Belinda S. Cowlinga,b,c,d,1 and Jocelyn Laportea,b,c,d,1,∗ aDepartment of Translational Medicine and Neurogenetics, Institut de G´en´etique et de Biologie Mol´eculaire et Cellulaire (IGBMC), Illkirch, France bInstitut National de la Sant´eetdelaRechercheM´edicale (INSERM), U1258, Illkirch, France cCentre National de la Recherche Scientifique (CNRS), UMR7104, Illkirch, France dUniversit´e de Strasbourg, Illkirch, France Abstract. -

A Schematic Approach to Hypotonia in Infancy
Leyenaar.qxd 8/26/2005 4:03 PM Page 397 NEUROLOGY SUBSPECIALTY ARTICLE A schematic approach to hypotonia in infancy JoAnna Leyenaar MD MPH, Peter Camfield MD FRCPC, Carol Camfield MD FRCPC J Leyenaar, P Camfield, C Camfield. A schematic approach Une démarche schématique envers l’hypotonie to hypotonia in infancy. Paediatr Child Health 2005; pendant la première enfance 10(7):397-400. L’hypotonie peut être le signe révélateur de nombreuses maladies Hypotonia may be the presenting sign for many systemic diseases and systémiques ou du système nerveux. Le présent article traite d’une diseases of the nervous system. The present paper discusses a rational, démarche diagnostique rationnelle, simple et précise envers l’hypotonie simple and accurate diagnostic approach to hypotonia in infancy, pendant la première enfance, illustrée par le cas d’une fillette de cinq mois illustrated by the case of a five-month-old infant girl recently referred récemment aiguillée vers le IWK Health Centre de Halifax, en Nouvelle- to the IWK Health Centre in Halifax, Nova Scotia. Key points in the Écosse. Les principaux points de l’anamnèse et de l’examen physique sont history and physical examination are outlined to allow a tailored exposés afin de permettre une exploration personnalisée de la patiente et investigation both for the patient and for other hypotonic infants. A des autres nourrissons hypotoniques. Un exposé sur une importante discussion of an important neuromuscular disease, diagnosed in the maladie neuromusculaire, diagnostiquée chez la patiente, conclut l’article. present patient, concludes the paper. Key Words: Hypotonia; Infant; Spinal muscular atrophy nfants with hypotonia pose challenges for clinicians respiratory syncytial virus-positive bronchiolitis. -

The Role of Z-Disc Proteins in Myopathy and Cardiomyopathy
International Journal of Molecular Sciences Review The Role of Z-disc Proteins in Myopathy and Cardiomyopathy Kirsty Wadmore 1,†, Amar J. Azad 1,† and Katja Gehmlich 1,2,* 1 Institute of Cardiovascular Sciences, College of Medical and Dental Sciences, University of Birmingham, Birmingham B15 2TT, UK; [email protected] (K.W.); [email protected] (A.J.A.) 2 Division of Cardiovascular Medicine, Radcliffe Department of Medicine and British Heart Foundation Centre of Research Excellence Oxford, University of Oxford, Oxford OX3 9DU, UK * Correspondence: [email protected]; Tel.: +44-121-414-8259 † These authors contributed equally. Abstract: The Z-disc acts as a protein-rich structure to tether thin filament in the contractile units, the sarcomeres, of striated muscle cells. Proteins found in the Z-disc are integral for maintaining the architecture of the sarcomere. They also enable it to function as a (bio-mechanical) signalling hub. Numerous proteins interact in the Z-disc to facilitate force transduction and intracellular signalling in both cardiac and skeletal muscle. This review will focus on six key Z-disc proteins: α-actinin 2, filamin C, myopalladin, myotilin, telethonin and Z-disc alternatively spliced PDZ-motif (ZASP), which have all been linked to myopathies and cardiomyopathies. We will summarise pathogenic variants identified in the six genes coding for these proteins and look at their involvement in myopathy and cardiomyopathy. Listing the Minor Allele Frequency (MAF) of these variants in the Genome Aggregation Database (GnomAD) version 3.1 will help to critically re-evaluate pathogenicity based on variant frequency in normal population cohorts. -

Affected Female Carriers of MTM1 Mutations Display a Wide Spectrum
Acta Neuropathol DOI 10.1007/s00401-017-1748-0 ORIGINAL PAPER Afected female carriers of MTM1 mutations display a wide spectrum of clinical and pathological involvement: delineating diagnostic clues Valérie Biancalana1,2,3,4,5 · Sophie Scheidecker1 · Marguerite Miguet1 · Annie Laquerrière6 · Norma B. Romero7,8 · Tanya Stojkovic8 · Osorio Abath Neto9 · Sandra Mercier10,11,12 · Nicol Voermans13 · Laura Tanner14 · Curtis Rogers15 · Elisabeth Ollagnon‑Roman16 · Helen Roper17 · Célia Boutte18 · Shay Ben‑Shachar19 · Xavière Lornage2,3,4,5 · Nasim Vasli2,3,4,5 · Elise Schaefer20 · Pascal Laforet21 · Jean Pouget22 · Alexandre Moerman23 · Laurent Pasquier24 · Pascale Marcorelle25,26 · Armelle Magot12 · Benno Küsters27 · Nathalie Streichenberger28 · Christine Tranchant29 · Nicolas Dondaine1 · Raphael Schneider2,3,4,5,30 · Claire Gasnier1 · Nadège Calmels1 · Valérie Kremer31 · Karine Nguyen32 · Julie Perrier12 · Erik Jan Kamsteeg33 · Pierre Carlier34 · Robert‑Yves Carlier35 · Julie Thompson30 · Anne Boland36 · Jean‑François Deleuze36 · Michel Fardeau7,8 · Edmar Zanoteli9 · Bruno Eymard21 · Jocelyn Laporte2,3,4,5 Received: 9 May 2017 / Revised: 24 June 2017 / Accepted: 2 July 2017 © Springer-Verlag GmbH Germany 2017 Abstract X-linked myotubular myopathy (XLMTM), a females and to delineate diagnostic clues, we character- severe congenital myopathy, is caused by mutations in the ized 17 new unrelated afected females and performed a MTM1 gene located on the X chromosome. A majority of detailed comparison with previously reported cases at the afected males die in the early postnatal period, whereas clinical, muscle imaging, histological, ultrastructural and female carriers are believed to be usually asymptomatic. molecular levels. Taken together, the analysis of this large Nevertheless, several afected females have been reported. cohort of 43 cases highlights a wide spectrum of clini- To assess the phenotypic and pathological spectra of carrier cal severity ranging from severe neonatal and generalized weakness, similar to XLMTM male, to milder adult forms. -
THE NON-DYSTROPHIC MYOPATHIES JOHN PEARCE, M.B., M.R.C.P., Department of Neurology, the General Infirmary, Leeds
Postgrad Med J: first published as 10.1136/pgmj.41.476.347 on 1 June 1965. Downloaded from POSTGRAD. MED. J. (1965), 41, 347 THE NON-DYSTROPHIC MYOPATHIES JOHN PEARCE, M.B., M.R.C.P., Department of Neurology, The General Infirmary, Leeds. THE TERM 'myopathy' is applied to any disorder Polymyositis may affect people of any age, of the muscle fibre, the muscle fibre membrane, but the age of onset is from 30 to 60 in 60% the myoneural junction, or the muscle connect- of cases. The chief symptom is weakness of ive tissue. 'Non-dystrophic myopathy' includes proximal muscles of the arms and/or legs all diseases of muscle excluding those genetically in every case. Distal muscles are affected in determined primary degenerative myopathies, one third, and the neck muscles in two thirds collectively known as Muscular Dystrophy. of patients. Fever, muscular pain and tenderness TABLE 1 are seen most often in the more acute forms, CLASSIFICATION OF NON-DYSTROPHIC MYOPATHIES and their absence should not lead to neglecting 1. Inflammatory Polymyositis as a Myopathy Connective tissue disorders polymyositis possible diagnosis. Other inflammatory mvopathies Acute polymyositis is not common, but may 2. Metabolic Familial periodic paralysis progress rapidly and involve the respiratory Myopathy Muscle glycogenoses muscles, sometimes with a fatal termination Myoglobinuric myopathies within a few weeks or months. Myopathies associated with Subacute and electrolyte imbalance chronic forms are more frequent, and present Unclassified myopathies with a progressive weakness and moderate of shoulder 3. Endocrine Thyrotoxicosis wasting and pelvic girdle muscles. Myopathy Cushing's Syndrome There is sometimes no systemic disturbance, Steroid myopathy and pain and tenderness are lacking. -

Identification of Gene Mutations in Patients with Primary Periodic
Luo et al. BMC Neurology (2019) 19:92 https://doi.org/10.1186/s12883-019-1322-6 RESEARCH ARTICLE Open Access Identification of gene mutations in patients with primary periodic paralysis using targeted next-generation sequencing Sushan Luo1†, Minjie Xu2†, Jian Sun1, Kai Qiao3, Jie Song1, Shuang Cai1, Wenhua Zhu1, Lei Zhou1, Jianying Xi1, Jiahong Lu1, Xiaohua Ni2, Tonghai Dou4 and Chongbo Zhao1,5* Abstract Background: Primary periodic paralysis is characterized by recurrent quadriplegia typically associated with abnormal serum potassium levels. The molecular diagnosis of primary PP previously based on Sanger sequencing of hot spots or exon-by-exon screening of the reported genes. Methods: We developed a gene panel that includes 10 ion channel-related genes and 245 muscular dystrophy- and myopathy-related genes and used this panel to diagnose 60 patients with primary periodic paralysis and identify the disease-causing or risk-associated gene mutations. Results: Mutations of 5 genes were discovered in 39 patients (65.0%). SCN4A, KCNJ2 and CACNA1S variants accounted for 92.5% of the patients with a genetic diagnosis. Conclusions: Targeted next-generation sequencing offers a cost-effective approach to expand the genotypes of primary periodic paralysis. A clearer genetic profile enables the prevention of paralysis attacks, avoidance of triggers and the monitoring of complications. Keywords: Primary periodic paralysis, Targeted next-generation sequencing, Gene panel, Gene mutation distribution, Calcium homeostasis. Background (SCN4A) and potassium voltage-gated channel subfamily Periodic paralysis (PP) is characterized by episodes of J member 2 (KCNJ2), that encode voltage-gated chan- muscle weakness that occur at irregular intervals due to nels in muscle membranes that generate or sustain skeletal muscle ion channelopathies. -

Distal Myopathies a Review: Highlights on Distal Myopathies with Rimmed Vacuoles
Review Article Distal myopathies a review: Highlights on distal myopathies with rimmed vacuoles May Christine V. Malicdan, Ikuya Nonaka Department of Neuromuscular Research, National Institutes of Neurosciences, National Center of Neurology and Psychiatry, Tokyo, Japan Distal myopathies are a group of heterogeneous disorders Since the discovery of the gene loci for a number classiÞ ed into one broad category due to the presentation of distal myopathies, several diseases previously of weakness involving the distal skeletal muscles. The categorized as different disorders have now proven to recent years have witnessed increasing efforts to identify be the same or allelic disorders (e.g. distal myopathy the causative genes for distal myopathies. The identiÞ cation with rimmed vacuoles and hereditary inclusion body of few causative genes made the broad classiÞ cation of myopathy, Miyoshi myopathy and limb-girdle muscular these diseases under “distal myopathies” disputable and dystrophy type 2B (LGMD 2B). added some enigma to why distal muscles are preferentially This review will focus on the most commonly affected. Nevertheless, with the clariÞ cation of the molecular known and distinct distal myopathies, using a simple basis of speciÞ c conditions, additional clues have been classification: distal myopathies with known molecular uncovered to understand the mechanism of each condition. defects [Table 1] and distal myopathies with unknown This review will give a synopsis of the common distal causative genes [Table 2]. The identification of the myopathies, presenting salient facts regarding the clinical, genes involved in distal myopathies has broadened pathological, and molecular aspects of each disease. Distal this classification into sub-categories as to the location myopathy with rimmed vacuoles, or Nonaka myopathy, will of encoded proteins: sarcomere (titin, myosin); plasma be discussed in more detail. -

Myasthenia and Related Disorders of the Neuromuscular Junction Jennifer Spillane, David J Beeson, Dimitri M Kullmann
Myasthenia and related disorders of the neuromuscular junction Jennifer Spillane, David J Beeson, Dimitri M Kullmann To cite this version: Jennifer Spillane, David J Beeson, Dimitri M Kullmann. Myasthenia and related disorders of the neuromuscular junction. Journal of Neurology, Neurosurgery and Psychiatry, BMJ Publishing Group, 2010, 81 (8), pp.850. 10.1136/jnnp.2008.169367. hal-00557404 HAL Id: hal-00557404 https://hal.archives-ouvertes.fr/hal-00557404 Submitted on 19 Jan 2011 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Myasthenia and related disorders of the neuromuscular junction Jennifer Spillane1, David J Beeson2 and Dimitri M Kullmann1 1UCL Institute of Neurology 2Weatherall Institute for Molecular Medicine, Oxford University Abtract Our understanding of transmission at the neuromuscular junction has increased greatly in recent years. We now recognise a wide variety of autoimmune and genetic diseases that affect this specialised synapse, causing muscle weakness and fatigue. These disorders greatly affect quality of life and rarely can be fatal. Myasthenia Gravis is the most common disorder and is most commonly caused by auto‐antibodies targeting postsynaptic acetylcholine receptors (AChRs). Antibodies to muscle‐specific kinase (MuSK) are detected in a variable proportion of the remainder. -

Disease Mutations in the Ryanodine Receptor N-Terminal Region Couple to a Mobile Intersubunit Interface
ARTICLE Received 1 Oct 2012 | Accepted 15 Jan 2013 | Published 19 Feb 2013 DOI: 10.1038/ncomms2501 OPEN Disease mutations in the ryanodine receptor N-terminal region couple to a mobile intersubunit interface Lynn Kimlicka1, Kelvin Lau1, Ching-Chieh Tung1 & Filip Van Petegem1 Ryanodine receptors are large channels that release Ca2 þ from the endoplasmic and sar- coplasmic reticulum. Hundreds of RyR mutations can cause cardiac and skeletal muscle disorders, yet detailed mechanisms explaining their effects have been lacking. Here we compare pseudo-atomic models and propose that channel opening coincides with widen- ing of a cytoplasmic vestibule formed by the N-terminal region, thus altering an interface targeted by 20 disease mutations. We solve crystal structures of several disease mutants that affect intrasubunit domain–domain interfaces. Mutations affecting intrasubunit ionic pairs alter relative domain orientations, and thus couple to surrounding interfaces. Buried disease mutations cause structural changes that also connect to the intersubunit contact area. These results suggest that the intersubunit contact region between N-terminal domains is a prime target for disease mutations, direct or indirect, and we present a model whereby ryanodine receptors and inositol-1,4,5-trisphosphate receptors are activated by altering domain arrangements in the N-terminal region. 1 Department of Biochemistry and Molecular Biology, Life Sciences Institute, University of British Columbia, Vancouver, British Columbia, Canada V6T 1Z3. Correspondence and requests for materials should be addressed to F.V.P. (email: fi[email protected]). NATURE COMMUNICATIONS | 4:1506 | DOI: 10.1038/ncomms2501 | www.nature.com/naturecommunications 1 & 2013 Macmillan Publishers Limited. All rights reserved. -
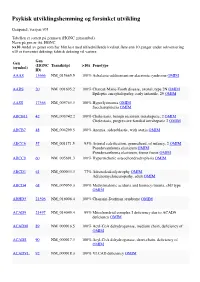
Psykisk Utviklingshemming Og Forsinket Utvikling
Psykisk utviklingshemming og forsinket utvikling Genpanel, versjon v03 Tabellen er sortert på gennavn (HGNC gensymbol) Navn på gen er iht. HGNC >x10 Andel av genet som har blitt lest med tilfredstillende kvalitet flere enn 10 ganger under sekvensering x10 er forventet dekning; faktisk dekning vil variere. Gen Gen (HGNC Transkript >10x Fenotype (symbol) ID) AAAS 13666 NM_015665.5 100% Achalasia-addisonianism-alacrimia syndrome OMIM AARS 20 NM_001605.2 100% Charcot-Marie-Tooth disease, axonal, type 2N OMIM Epileptic encephalopathy, early infantile, 29 OMIM AASS 17366 NM_005763.3 100% Hyperlysinemia OMIM Saccharopinuria OMIM ABCB11 42 NM_003742.2 100% Cholestasis, benign recurrent intrahepatic, 2 OMIM Cholestasis, progressive familial intrahepatic 2 OMIM ABCB7 48 NM_004299.5 100% Anemia, sideroblastic, with ataxia OMIM ABCC6 57 NM_001171.5 93% Arterial calcification, generalized, of infancy, 2 OMIM Pseudoxanthoma elasticum OMIM Pseudoxanthoma elasticum, forme fruste OMIM ABCC9 60 NM_005691.3 100% Hypertrichotic osteochondrodysplasia OMIM ABCD1 61 NM_000033.3 77% Adrenoleukodystrophy OMIM Adrenomyeloneuropathy, adult OMIM ABCD4 68 NM_005050.3 100% Methylmalonic aciduria and homocystinuria, cblJ type OMIM ABHD5 21396 NM_016006.4 100% Chanarin-Dorfman syndrome OMIM ACAD9 21497 NM_014049.4 99% Mitochondrial complex I deficiency due to ACAD9 deficiency OMIM ACADM 89 NM_000016.5 100% Acyl-CoA dehydrogenase, medium chain, deficiency of OMIM ACADS 90 NM_000017.3 100% Acyl-CoA dehydrogenase, short-chain, deficiency of OMIM ACADVL 92 NM_000018.3 100% VLCAD -

Combined Web 759..782
Movement Disorders Vol. 24, No. 5, 2009, pp. 759–782 Ó 2009 Movement Disorder Society Brief Reports Clinical Characteristics of Psychogenic movement disorders (PMDs) are not uncommon in movement disorder clinics.1 PMDs may 49 Patients with Psychogenic phenomenologically mimic almost all movement disor- Movement Disorders in a Tertiary ders. The most common movement disorder is tremor, followed by dystonia and others.2–5 Clinic in Turkey Diagnostic criteria for PMDs was first identified by Fahn and Williams, based on atypical and common Sibel Ertan, MD,1 Derya Uluduz, MD,1 clinical clues.6 Later, other authors described additional 1* 1 Sibel O¨ zekmekc¸i, MD, Gu¨nes Kiziltan, MD, features to distinguish PMD patients from those with 2 1 1 Turan Ertan, MD, Cengiz Yalc¸inkaya, MD, , and neurogenic movement disorders.7–9 ¨ 1 and C¸ igdem Ozkara, MD Because there is no study written in English on any 1Department of Neurology, Cerrahpasa Faculty of Medicine, hospital-based data of PMDs in Turkey, we aimed to Istanbul University, Istanbul, Turkey; 2Department of identify the frequency and phenomenological features Psychiatry, Cerrahpasa Faculty of Medicine, Istanbul of PMDs in our patient population with movement dis- University, Istanbul, Turkey orders. Abstract: Patients admitted to movement disorders outpa- tient unit at a university hospital between January 2002 and June 2007 were screened for psychogenic movement PATIENTS AND METHODS disorders (PMDs). Out of 1,743 patients, 49 patients Patients admitted to our Movement Disorders Unit (2.8%), including four children, were diagnosed to have between January 2002 and June 2007, were screened PMDs. Women to men ratio was 34/15.