Ischial Tuberosity Avulsion General PT Protocol
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Gluteal Region-II
Gluteal Region-II Dr Garima Sehgal Associate Professor King George’s Medical University UP, Lucknow Structures in the Gluteal region • Bones & joints • Ligaments Thickest muscle • Muscles • Vessels • Nerves Thickest nerve • Bursae Learning Objectives By the end of this teaching session Gluteal region –II all the MBBS 1st year students must be able to: • Enumerate the nerves of gluteal region • Write a short note on nerves of gluteal region • Describe the location & relations of sciatic nerve in gluteal region • Enumerate the arteries of gluteal region • Write a short note on arteries of gluteal region • Enumerate the arteries taking part in trochanteric and cruciate anastomosis • Write a short note on trochanteric and cruciate anastomosis • Enumerate the structures passing through greater sciatic foramen • Enumerate the structures passing through lesser sciatic foramen • Enumerate the bursae in relation to gluteus maximus • Enumerate the structures deep to gluteus maximus • Discuss applied anatomy Nerves of Gluteal region (all nerves in gluteal region are branches of sacral plexus) Superior gluteal nerve (L4,L5, S1) Inferior gluteal nerve (L5, S1, S2) FROM DORSAL DIVISIONS Perforating cutaneous nerve (S2,S3) Nerve to quadratus femoris (L4,L5, S1) Nerve to obturator internus (L5, S1, S2) FROM VENTRAL DIVISIONS Pudendal nerve (S2,S3,S4) Sciatic nerve (L4,L5,S1,S2,S3) Posterior cutaneous nerve of thigh FROM BOTH DORSAL &VENTRAL (S1,S2) & (S2,S3) DIVISIONS 1. Superior Gluteal nerve (L4,L5,S1- dorsal division) 1 • Enters through the greater 3 sciatic foramen • Above piriformis 2 • Runs forwards between gluteus medius & gluteus minimus • SUPPLIES: 1. Gluteus medius 2. Gluteus minimus 3. Tensor fasciae latae 2. -

Approach to the Anterior Pelvis (Enneking Type III Resection) Bruno Fuchs, MD Phd & Franklin H.Sim, MD Indication 1
Approach to the Anterior Pelvis (Enneking Type III Resection) Bruno Fuchs, MD PhD & Franklin H.Sim, MD Indication 1. Tumors of the pubis 2. part of internal and external hemipelvectomy 3. pelvic fractures Technique 1. Positioning: Type III resections involve the excision of a portion of the symphysis or the whole pubis from the pubic symphysis to the lateral margin of the obturator foramen. The best position for these patients is the lithotomy or supine position. The patient is widely prepared and draped in the lithotomy position with the affected leg free to allow manipulation during the procedure. This allows the hip to be flexed, adducted, and externally rotated to facilitate exposure. 2. Landmarks: One should palpate the ASIS, the symphysis with the pubic tubercles, and the ischial tuberosity. 3. Incision: The incision may be Pfannenstiel like with vertical limbs set laterally along the horizontal incision depending on whether the pubic bones on both sides are resected or not. Alternatively, if only one side is resected, a curved incision following the root of the thigh may be used. This incision begins below the inguinal ligament along the medial border of the femoral triangle and extends across the medial thigh a centimeter distal to the inguinal crease and perineum, to curve distally below the ischium several centimeters (Fig.1). 4. Full thickness flaps are raised so that the anterior inferior pubic ramus is shown in its entire length, from the pubic tubercle to the ischial spine. Laterally, the adductor muscles are visualized, cranially the pectineus muscle and the pubic tubercle with the insertion of the inguinal ligament (Fig.2). -

Surgical Approaches to Fractures of the Acetabulum and Pelvis Joel M
Surgical Approaches to Fractures of the Acetabulum and Pelvis Joel M. Matta, M.D. Sponsored by Mizuho OSI APPROACHES TO THE The table will also stably position the ACETABULUM limb in a number of different positions. No one surgical approach is applicable for all acetabulum fractures. KOCHER-LANGENBECK After examination of the plain films as well as the CT scan the surgeon should APPROACH be knowledgeable of the precise anatomy of the fracture he or she is The Kocher-Langenbeck approach is dealing with. A surgical approach will primarily an approach to the posterior be selected with the expectation that column of the Acetabulum. There is the entire reduction and fixation can excellent exposure of the be performed through the surgical retroacetabular surface from the approach. A precise knowledge of the ischial tuberosity to the inferior portion capabilities of each surgical approach of the iliac wing. The quadrilateral is also necessary. In order to maximize surface is accessible by palpation the capabilities of each surgical through the greater or lesser sciatic approach it is advantageous to operate notch. A less effective though often the patient on the PROfx® Pelvic very useful approach to the anterior Reconstruction Orthopedic Fracture column is available by manipulation Table which can apply traction in a through the greater sciatic notch or by distal and/or lateral direction during intra-articular manipulation through the operation. the Acetabulum (Figure 1). Figure 2. Fractures operated through the Kocher-Langenbeck approach. Figure 3. Positioning of the patient on the PROfx® surgical table for operations through the Kocher-Lagenbeck approach. -
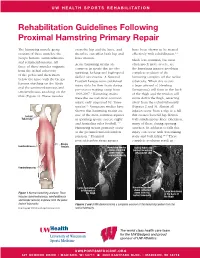
Rehabilitation Guidelines Following Proximal Hamstring Primary Repair
UW HEALTH SPORTS REHABILITATION Rehabilitation Guidelines Following Proximal Hamstring Primary Repair The hamstring muscle group cross the hip and the knee, and have been shown to be treated consists of three muscles: the therefore can affect both hip and effectively with rehabilitation.1, 8 biceps femoris, semitendinosus knee motion. Much less common, but most and semimembranosus. All Acute hamstring strains are often much more severe, are three of these muscles originate common in sports that involve the hamstring injuries involving from the ischial tuberosity sprinting, kicking and high-speed complete avulsion of the of the pelvis and then insert skilled movements. A National hamstring complex off the ischial below the knee with the biceps Football League team published tuberosity. When this occurs femoris attaching on the fibula injury data for their team during a large amount of bleeding and the semimembranosus and pre-season training camp from (hematoma) will form in the back semitendinosus attaching on the 1998-2007.1 Hamstring strains of the thigh and the tendon will tibia (Figure 1). These muscles were the second most common move down the thigh, retracting injury, only surpassed by “knee away from the ischial tuberosity sprains”.1 Numerous studies have (Figures 2 and 3). Almost all shown that hamstring strains are injuries occur from a slip or a fall Ischial one of the most common injuries that creates forceful hip flexion Tuberosity in sprinting sports, soccer, rugby with simultaneous knee extension, and Australian rules football.1-12 -

Determination of Sex Using Os Coxae in Relation to Ischial Tuberosity – a Morphometric Study M
Research Article Determination of sex using os coxae in relation to ischial tuberosity – A morphometric study M. Shruthi, Karthik Ganesh Mohanraj* ABSTRACT Introduction: Sex determination of an unidentified individual is one of the main objectives when human skeletal remains are found, both in forensic investigation and archaeological studies. The distinctive morphology of the human hip bone and its clear sexual dimorphism build it of interest from anatomical, social science, and rhetorical points of analysis. Determination of biological sex is one of the most important determinations to be made from undocumented human remains which this study is aimed for. Materials and Methods: In the present study, a total of 30 dry human pelvic bones of unknown sex and without any gross abnormality will be collected from the Department of Anatomy, Saveetha Dental College, Chennai, for evaluation. With the help of Vernier caliper and ruler, the measurements such as minimum iliac breadth (MIB), maximum auricular length (MAL), and maximum ischiopubic length (MIPL) are measured. The results obtained were analyzed, tabulated, and represented graphically. Results: The average of MIB in male was found to be 57.61 ± 2.11 mm and in female was found to be 53.45 ± 3.14 mm. The MAL in male was 53.71 ± 1.67 mm and 49.16 ± 2.82 mm in females. The MIPL in male and female was 113.23 ± 4.89 mm and 107.2 ± 7.63 mm, respectively. Conclusion: The chances of attaining high levels of accuracy and reliability regarding sex identification are related to the skeletal components analyzed and the ability of techniques utilized to analyze shape and size differences among the sexes. -

An Up-To-Date Overview of Evaluation and Management
Translational Research in Anatomy 11 (2018) 5–9 Contents lists available at ScienceDirect Translational Research in Anatomy journal homepage: www.elsevier.com/locate/tria Ureterosciatic hernia: An up-to-date overview of evaluation and T management ∗ Jason Gandhia,b,c, Min Yea Leea, Gunjan Joshid, Noel L. Smithe, Sardar Ali Khana,f, a Department of Physiology and Biophysics, Stony Brook University School of Medicine, Stony Brook, NY, USA b Medical Student Research Institute, St. George's University School of Medicine, West Indies, Grenada c Department of Anatomical Sciences, St. George's University School of Medicine, West Indies, Grenada d Department of Internal Medicine, Stony Brook Southampton Hospital, Southampton, NY, USA e Foley Plaza Medical, New York, NY, USA f Department of Urology, Stony Brook University School of Medicine, Stony Brook, NY, USA ARTICLE INFO ABSTRACT Keywords: Ureterosciatic hernia, defined as a suprapiriform or infrapiriform herniation of the pelvic ureter, is the sliding of Ureter the ureters into the pelvic fossa, fovea, or greater or lesser sciatic foramen. This type of hernia is the rarest form Sciatic hernia of pelvic sciatic hernias. It may cause a wide range of cryptic clinical symptoms of pain, obstructive uropathy, Ureteral obstruction sepsis, or renal failure. This condition has been described in terms of involvement in inguinal, femoral, sciatic, Sepsis obturator, and thoracic regions. A high index of clinical suspicion is essential for diagnosis because the hernia Hydronephrosis develops in the pelvic cavity and becomes overlayed by the large gluteal muscle. Since ureterosciatic hernias Renal failure have not been adequately reviewed in the literature due to the limited number of case reports, we aim to aid the clinician's knowledge by discussing the relevant anatomy, classification, clinical symptoms, optional radiology, optional diagnostic instrumentation, and management. -

The Diagnosis of Acute Osteomyelitis of the Pelvis Alan Morgan, Alan K
POSTGRAD. MDI). J., (1966), 42, 74 Postgrad Med J: first published as 10.1136/pgmj.42.484.74 on 1 February 1966. Downloaded from THE DIAGNOSIS OF ACUTE OSTEOMYELITIS OF THE PELVIS ALAN MORGAN, ALAN K. YATES, M.B., Ch.B. (Brist.), F.R.C.S. Eng.* M.B., Ch.B. (Sheff.), F.R.C.S. Eng.** The Royal Infirmary and Children's Hospital, Sheffield. OSTEOMYELITIS of the pelvis has a sparse biblio- bone involved and does not include other graphy, probably because of its relative bones of ithe pelvis involved by subsequent infrequency in general orthopaedics. spread of the disease. Froener (1889) istated that less than 10%/ of In agreement with other authors we find cases occured in the pelvis in a series of 545 that the ilium is most commonly affected. The cases of acute osteomyelitis; Butler (1940) ilium forms the largest portion of the bony gives an incidence of 8% in 500 cases of acute pelvis. lits blade has an abundant blood supply osteomyelitis seen at the London Hospital. with a large nutrient artery entering its inner Von Bergmann (1906) found 63 cases of surface, and in the adult it is the only bone of osteomyelitis of the ilium in 71 cases of osteo- the pelvis containing haemopoetic marrow. myelitis of the pelvis. Krasnobajiv (1925), The ischium was more commonly involved Simmons (1915), Bearse (1923), Flickinger than in other series, but i,n no patient was the (1927) and Buosanti (1924) each give an in- pubis primarily infected, although it was in- cidence of osteomyelitis of the ilium of bet- volved by extension in several cases. -

Gluteal Region and Back of the Thigh Musculoskeletal Block - Lecture 14
Gluteal region and back of the thigh Musculoskeletal Block - Lecture 14 Objective: ✓ Contents of the gluteal region: 3 Glutei muscles: Gluteus maximus, medius and minimus. Other 5 Small muscles: Piriformis, Obturator internus, Superior gemellus, Inferior gemellus and Quadratus femoris. ✓ Nerves & vessels. ✓ Foramina: 1-GreaterSciaticForamen. 2-Lesser Sciatic Foramen. ✓ Back of the thigh: Hamstring muscles. Color index: Important In male’s slides only In female’s slides only Extra information, explanation Editing file Contact us: [email protected] Contents Of Gluteal Region: Glutei: 1. Gluteus maximus 2. Gluteus medius 3. Gluteus minimus Muscles Small Muscles (Lateral Rotators): 1. Piriformis 2. Superior gemellus 3. Obturator internus 4. Inferior gemellus 5. Quadratus femoris (All from Sacral plexus): 1. Sciatic nerve 2. Superior gluteal nerve 3. Inferior gluteal nerve 4. Posterior cutaneous nerve of thigh Nerves 5. Nerve to obturator internus 6. Nerve to quadratus femoris 7. Pudendal nerve (all from internal iliac vessels) 1. Superior Gluteal vessel 2. Inferior Gluteal vessel Vessels 3. Internal pudendal vessels Greater Sciatic Foramen: Pictures Greater Sciatic notch of hip bone is transformed into foramen by: sacrotuberous(between the sacrum to ischial tuberosity) & sacrospinous (between the sacrum to ischial spine) ligaments. Structures passing through Greater sciatic foramen: Piriformis muscle - (Above piriformis muscle) Superior gluteal nerves and vessels - (Below Piriformis muscle) Inferior Gluteal nerves and vessels Sciatic nerve Posterior cutaneous nerve of thigh (superficialis) Nerve to quadratus femoris Nerve to obturator internus Pudendal Nerve* Internal Pudendal vessels* *go to Lesser Sciatic foramen too Lesser Sciatic foramen: Lesser Sciatic notch of hip is transformed into foramen by Sacrotuberous & Sacrospinous ligaments. -

7-Pelvis Nd Sacrum.Pdf
Color Code Important PELVIS & SACRUM Doctors Notes Notes/Extra explanation EDITING FILE Objectives: Describe the bony structures of the pelvis. Describe in detail the hip bone, the sacrum, and the coccyx. Describe the boundaries of the pelvic inlet and outlet. Identify the articulations of the bony pelvis. List the major differences between the male and female pelvis. List the different types of female pelvis. Overview: • check this video to have a good picture about the lecture: https://www.youtube.com/watch?v=PJOT1cQHFqA https://www.youtube.com/watch?v=3v5AsAESg1Q&feature=youtu.be • BONY PELVIS = 2 Hip Bones (lateral) + Sacrum (Posterior) + Coccyx (Posterior). • Hip bone is composed of 3 parts = Superior part (Ilium) + Lower anterior part (Pubis) + Lower posterior part (Ischium) only on the boys slides’ BONY PELVIS Location SHAPE Structure: Pelvis can be regarded as a basin with holes in its walls. The structure of the basin is composed of: Pelvis is the region of the Bowl shaped 4 bones 4 joints trunk that lies below the abdomen. 1-sacrum A. Two hip bones: These form the lateral and 2-ilium anterior walls of the bony pelvis. 3-ischium B. Sacrum: It forms most of the posterior wall. 4-pubic C. Coccyx: It forms most of the posterior wall. 5-pubic symphysis 6-Acetabulum Function # Primary: The skeleton of the pelvis is a basin-shaped ring of bones with holes in its wall connecting the vertebral column to both femora. Its primary functions are: bear the weight of the upper body when sitting and standing; transfer that weight from the axial skeleton to the lower appendicular skeleton when standing and walking; provide attachments for and withstand the forces of the powerful muscles of locomotion and posture. -

Differential Diagnosis for the Lower Extremity
Differential diagnosis for the Lower extremity Greg Bellisari MD Introduction • Hip • Knee • Leg • Ankle • Foot • Hope you had tons of coffee, only 128 more slides to go!! Sports and hip injuries • Hip and pelvis subjected to substantial forces. – Up to 8 x body weight • Adult: 5 - 6% of athletic injuries. • Pediatric: 10 - 24% of athletic injuries. • High risk sports: Ballet, Running, Soccer, Contact sports. Introduction Hip & Groin Pain • One of the most difficult problems to diagnose and treat in sports. • Symptoms are often indistinct, poorly localized. • Early and accurate diagnosis is essential: – Rehab times prolonged – May result in chronic, disabling pain “Hip” Pain • Patients may present with chief complaint of “hip” pain, but it may not actually be coming from their hip – Intrarticular hip – Extrarticular hip – Lumbar spin – Sacroiliac joint – Other - Intra-abdominal, hernia, GI, GU History • Knee pain – Can be the initial complaint of hip pathology – Not uncommon for a patient with hip arthritis to present with knee pain – Differentiate with exam, X-rays, injections Initial evaluation • Hip pain – History • Where, how long, trauma, always aware, mechanical, radicular, what aggravates – Joint vs not joint • Joint: FAI, dysplasia, OA, AVN • Not Joint: Gluteal, back, hernia, hamstring, butt History • Absence of groin pain does not preclude an intraarticular hip injury • Testicular pain does not come from the hip Differential Diagnosis Hip & Groin Pain ADULT PEDIATRIC • Stress fractures • Avulsion fracture • Osteitis pubis • ASIS -
Pelvis I: Bones and Muscles
PELVISPELVIS I:I: BONESBONES ANDAND MUSCLESMUSCLES IntroductionIntroduction----whywhy isis pelvispelvis soso hard?hard? BonyBony structuresstructures ofof thethe pelvispelvis MusclesMuscles ofof thethe pelvispelvis---- attachingattaching thethe leleggss forfor uuppririgghtht livinlivingg WhyWhy isis thethe pelvispelvis hardhard----#1#1 uprightupright PelvicPelvic tilttilt oror howhow wewe gotgot toto bebe uprightupright ––CompareCompare withwith quadrupedquadruped (cat(cat forfor instance)instance) BowlBowl conceptconcept ––pelvispelvis spillsspills forwardforward ––HerniaHernia ––““beerbeer bellybelly”” ––InIn humanhuman minorminor pelvispelvis isis behindbehind (posterior)(posterior) toto gutsguts andand abdominalabdominal cavitycavity HumanHuman pelvispelvis stillstill hashas quadrupedquadruped orientationorientation WhyWhy isis thethe pelvispelvis hardhard #2#2 (fig(fig leafs)leafs) “Private parts” don’t uncover except in most intimate setting (or medical setting!) Not comfortable seeing or talking about (except jokes) Now serious-many medical issues Realize and confront, not dehumanize-- develop professional manner and language--starts with anatomy BonyBony structurestructure ofof thethe pelvispelvis MAIN STRUCTURES HOLES Hip bone (innominate, False and true pelvis os coxae)--fusion of (major, minor pelvis) – Ilium (“hips”) Pelvic inlet, pelvic – Ischium (“rear”) outlet – Pubis (anterior midline) Sacrotuberous Sacrum and coccyx ligament Acetabulum Sacrospinous ligament Femur--head, neck, Greater, lesser sciatic greater -

A Variant of the Sciatic Nerve and Its Clinical Implications
Open Access Case Report DOI: 10.7759/cureus.2874 A Variant of the Sciatic Nerve and its Clinical Implications Graham Dupont 1 , Florence Unno 2 , Joe Iwanaga 3 , Rod J. Oskouian 4 , R. Shane Tubbs 5 1. Neuroscience Institute, Seattle Science Foundation, Seattle , USA 2. Hansjörg Wyss Hip and Pelvis Center, Swedish Medical Center, Seattle, USA 3. Seattle Science Foundation, Seattle, USA 4. Neurosurgery, Swedish Neuroscience Institute, Seattle, USA 5. Neurosurgery, Seattle Science Foundation, Seattle, USA Corresponding author: Graham Dupont, [email protected] Abstract Variants of gluteal neural anatomy are important to consider, especially during surgical approaches to the hip. During the routine dissection of the gluteal region, a variant of the sciatic nerve was found where the nerve left the pelvis fully split into its tibial and common fibular components. Intrapelvically and extrapelvically, there was no splitting of the two components by the piriformis muscle. Distally, the two parts of the nerve were draped over the medial and lateral edges of the ischial tuberosity. To avoid iatrogenic injury to the sciatic nerve during invasive or surgical approaches to this region, all possible anatomical variations, such as the one presented herein, should be appreciated by the clinician. Categories: Medical Education, Neurology, Neurosurgery Keywords: nerve injury, iatrogenic, surgery, anatomy, posterior thigh, gluteal region Introduction The sciatic nerve is not a singular nerve itself, rather it is a bundle of two nerves—the common fibular and tibial nerves—bound together by a common epineural sheath that approximates them as they course inferiorly down the posterior gluteal region and posterior thigh. The sciatic nerve, usually arising from the L4-S3 segments of the sacral plexus, leaves the pelvis to enter the gluteal region via the greater sciatic foramen and usually courses inferior to the piriformis.