NOTES from GUTMAN LECTURE 10/26 Use This Outline to Study From
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Minimally Invasive Surgical Treatment Using 'Iliac Pillar' Screw for Isolated
European Journal of Trauma and Emergency Surgery (2019) 45:213–219 https://doi.org/10.1007/s00068-018-1046-0 ORIGINAL ARTICLE Minimally invasive surgical treatment using ‘iliac pillar’ screw for isolated iliac wing fractures in geriatric patients: a new challenge Weon‑Yoo Kim1,2 · Se‑Won Lee1,3 · Ki‑Won Kim1,3 · Soon‑Yong Kwon1,4 · Yeon‑Ho Choi5 Received: 1 May 2018 / Accepted: 29 October 2018 / Published online: 1 November 2018 © Springer-Verlag GmbH Germany, part of Springer Nature 2018 Abstract Purpose There have been no prior case series of isolated iliac wing fracture (IIWF) due to low-energy trauma in geriatric patients in the literature. The aim of this study was to describe the characteristics of IIWF in geriatric patients, and to pre- sent a case series of IIWF in geriatric patients who underwent our minimally invasive screw fixation technique named ‘iliac pillar screw fixation’. Materials and methods We retrospectively reviewed six geriatric patients over 65 years old who had isolated iliac wing fracture treated with minimally invasive screw fixation technique between January 2006 and April 2016. Results Six geriatric patients received iliac pillar screw fixation for acute IIWFs. The incidence of IIWFs was approximately 3.5% of geriatric patients with any pelvic bone fractures. The main fracture line exists in common; it extends from a point between the anterosuperior iliac spine and the anteroinferior iliac spine to a point located at the dorsal 1/3 of the iliac crest whether fracture was comminuted or not. Regarding the Koval walking ability, patients who underwent iliac pillar screw fixation technique tended to regain their pre-injury walking including one patient in a previously bedridden state. -
The Subperitoneal Space and Peritoneal Cavity: Basic Concepts Harpreet K
ª The Author(s) 2015. This article is published with Abdom Imaging (2015) 40:2710–2722 Abdominal open access at Springerlink.com DOI: 10.1007/s00261-015-0429-5 Published online: 26 May 2015 Imaging The subperitoneal space and peritoneal cavity: basic concepts Harpreet K. Pannu,1 Michael Oliphant2 1Department of Radiology, Memorial Sloan Kettering Cancer Center, 1275 York Avenue, New York, NY 10065, USA 2Department of Radiology, Wake Forest University School of Medicine, Winston-Salem, NC, USA Abstract The peritoneum is analogous to the pleura which has a visceral layer covering lung and a parietal layer lining the The subperitoneal space and peritoneal cavity are two thoracic cavity. Similar to the pleural cavity, the peri- mutually exclusive spaces that are separated by the toneal cavity is visualized on imaging if it is abnormally peritoneum. Each is a single continuous space with in- distended by fluid, gas, or masses. terconnected regions. Disease can spread either within the subperitoneal space or within the peritoneal cavity to Location of the abdominal and pelvic organs distant sites in the abdomen and pelvis via these inter- connecting pathways. Disease can also cross the peri- There are two spaces in the abdomen and pelvis, the toneum to spread from the subperitoneal space to the peritoneal cavity (a potential space) and the subperi- peritoneal cavity or vice versa. toneal space, and these are separated by the peritoneum (Fig. 1). Regardless of the complexity of development in Key words: Subperitoneal space—Peritoneal the embryo, the subperitoneal space and the peritoneal cavity—Anatomy cavity remain separated from each other, and each re- mains a single continuous space (Figs. -

A Simplified Fascial Model of Pelvic Anatomical Surgery: Going Beyond
Anatomical Science International https://doi.org/10.1007/s12565-020-00553-z ORIGINAL ARTICLE A simplifed fascial model of pelvic anatomical surgery: going beyond parametrium‑centered surgical anatomy Stefano Cosma1 · Domenico Ferraioli2 · Marco Mitidieri3 · Marcello Ceccaroni4 · Paolo Zola5 · Leonardo Micheletti1 · Chiara Benedetto1 Received: 13 March 2020 / Accepted: 5 June 2020 © The Author(s) 2020 Abstract The classical surgical anatomy of the female pelvis is limited by its gynecological oncological focus on the parametrium and burdened by its modeling based on personal techniques of diferent surgeons. However, surgical treatment of pelvic diseases, spreading beyond the anatomical area of origin, requires extra-regional procedures and a thorough pelvic anatomical knowl- edge. This study evaluated the feasibility of a comprehensive and simplifed model of pelvic retroperitoneal compartmen- talization, based on anatomical rather than surgical anatomical structures. Such a model aims at providing an easier, holistic approach useful for clinical, surgical and educational purposes. Six fresh-frozen female pelves were macroscopically and systematically dissected. Three superfcial structures, i.e., the obliterated umbilical artery, the ureter and the sacrouterine ligament, were identifed as the landmarks of 3 deeper fascial-ligamentous structures, i.e., the umbilicovesical fascia, the urogenital-hypogastric fascia and the sacropubic ligament. The retroperitoneal areolar tissue was then gently teased away, exposing the compartments delimited by these deep fascial structures. Four compartments were identifed as a result of the intrapelvic development of the umbilicovesical fascia along the obliterated umbilical artery, the urogenital-hypogastric fascia along the mesoureter and the sacropubic ligaments. The retroperitoneal compartments were named: parietal, laterally to the umbilicovesical fascia; vascular, between the two fasciae; neural, medially to the urogenital-hypogastric fascia and visceral between the sacropubic ligaments. -

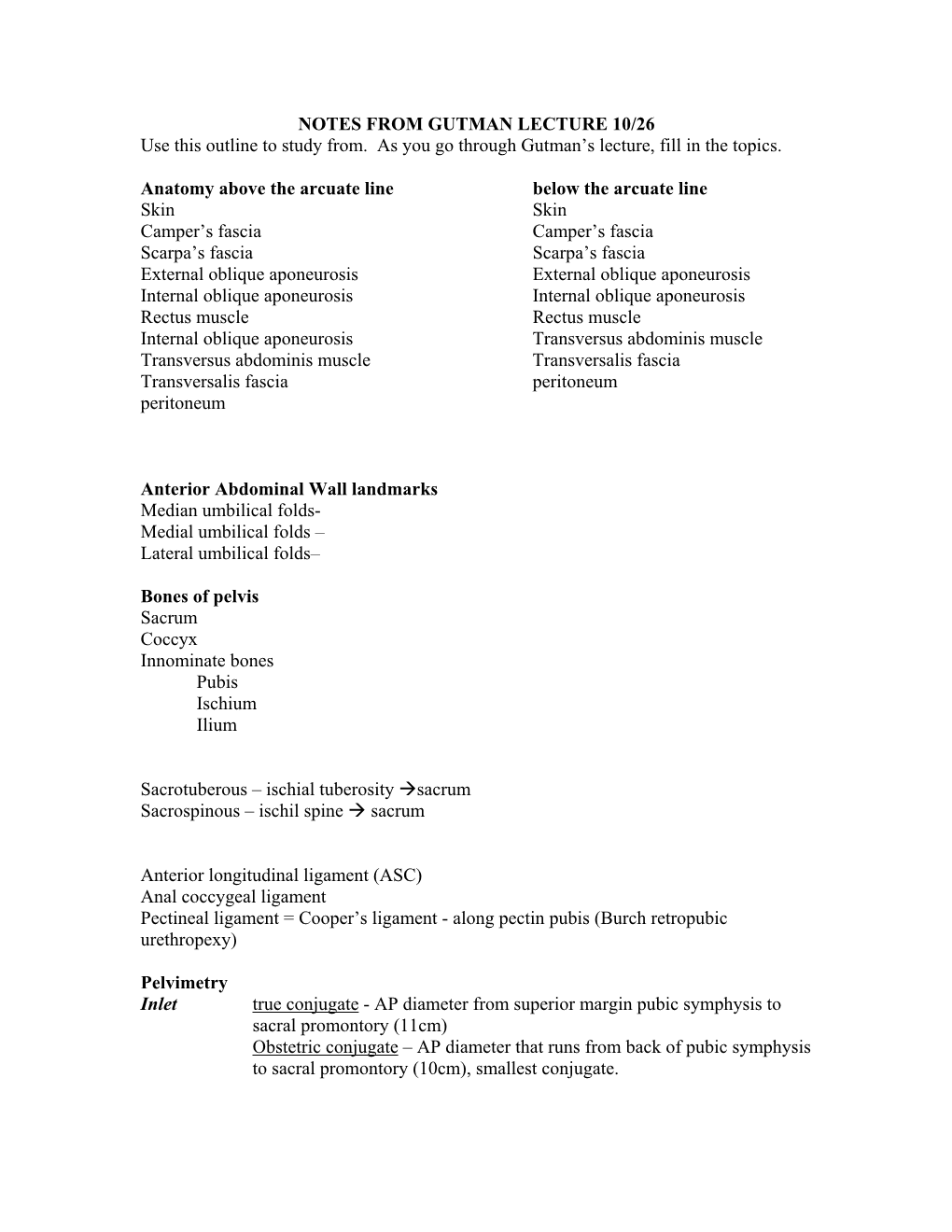
Pelvic Anatomyanatomy
PelvicPelvic AnatomyAnatomy RobertRobert E.E. Gutman,Gutman, MDMD ObjectivesObjectives UnderstandUnderstand pelvicpelvic anatomyanatomy Organs and structures of the female pelvis Vascular Supply Neurologic supply Pelvic and retroperitoneal contents and spaces Bony structures Connective tissue (fascia, ligaments) Pelvic floor and abdominal musculature DescribeDescribe functionalfunctional anatomyanatomy andand relevantrelevant pathophysiologypathophysiology Pelvic support Urinary continence Fecal continence AbdominalAbdominal WallWall RectusRectus FasciaFascia LayersLayers WhatWhat areare thethe layerslayers ofof thethe rectusrectus fasciafascia AboveAbove thethe arcuatearcuate line?line? BelowBelow thethe arcuatearcuate line?line? MedianMedial umbilicalumbilical fold Lateralligaments umbilical & folds folds BonyBony AnatomyAnatomy andand LigamentsLigaments BonyBony PelvisPelvis TheThe bonybony pelvispelvis isis comprisedcomprised ofof 22 innominateinnominate bones,bones, thethe sacrum,sacrum, andand thethe coccyx.coccyx. WhatWhat 33 piecespieces fusefuse toto makemake thethe InnominateInnominate bone?bone? PubisPubis IschiumIschium IliumIlium ClinicalClinical PelvimetryPelvimetry WhichWhich measurementsmeasurements thatthat cancan bebe mademade onon exam?exam? InletInlet DiagonalDiagonal ConjugateConjugate MidplaneMidplane InterspinousInterspinous diameterdiameter OutletOutlet TransverseTransverse diameterdiameter ((intertuberousintertuberous)) andand APAP diameterdiameter ((symphysissymphysis toto coccyx)coccyx) -

Gluteal Region-II
Gluteal Region-II Dr Garima Sehgal Associate Professor King George’s Medical University UP, Lucknow Structures in the Gluteal region • Bones & joints • Ligaments Thickest muscle • Muscles • Vessels • Nerves Thickest nerve • Bursae Learning Objectives By the end of this teaching session Gluteal region –II all the MBBS 1st year students must be able to: • Enumerate the nerves of gluteal region • Write a short note on nerves of gluteal region • Describe the location & relations of sciatic nerve in gluteal region • Enumerate the arteries of gluteal region • Write a short note on arteries of gluteal region • Enumerate the arteries taking part in trochanteric and cruciate anastomosis • Write a short note on trochanteric and cruciate anastomosis • Enumerate the structures passing through greater sciatic foramen • Enumerate the structures passing through lesser sciatic foramen • Enumerate the bursae in relation to gluteus maximus • Enumerate the structures deep to gluteus maximus • Discuss applied anatomy Nerves of Gluteal region (all nerves in gluteal region are branches of sacral plexus) Superior gluteal nerve (L4,L5, S1) Inferior gluteal nerve (L5, S1, S2) FROM DORSAL DIVISIONS Perforating cutaneous nerve (S2,S3) Nerve to quadratus femoris (L4,L5, S1) Nerve to obturator internus (L5, S1, S2) FROM VENTRAL DIVISIONS Pudendal nerve (S2,S3,S4) Sciatic nerve (L4,L5,S1,S2,S3) Posterior cutaneous nerve of thigh FROM BOTH DORSAL &VENTRAL (S1,S2) & (S2,S3) DIVISIONS 1. Superior Gluteal nerve (L4,L5,S1- dorsal division) 1 • Enters through the greater 3 sciatic foramen • Above piriformis 2 • Runs forwards between gluteus medius & gluteus minimus • SUPPLIES: 1. Gluteus medius 2. Gluteus minimus 3. Tensor fasciae latae 2. -

Applied Anatomy of the Hip RICARDO A
Applied Anatomy of the Hip RICARDO A. FERNANDEZ, MHS, PT, OCS, CSCS • Northwestern University The hip joint is more than just a ball-and- bones fuse in adults to form the easily recog- socket joint. It supports the weight of the nized “hip” bone. The pelvis, meaning bowl head, arms, and trunk, and it is the primary in Latin, is composed of three structures: the joint that distributes the forces between the innominates, the sacrum, and the coccyx pelvis and lower extremities.1 This joint is (Figure 1). formed from the articu- The ilium has a large flare, or iliac crest, Key PointsPoints lation of the proximal superiorly, with the easily palpable anterior femur with the innomi- superior iliac spine (ASIS) anterior with the The hip joint is structurally composed of nate at the acetabulum. anterior inferior iliac spine (AIIS) just inferior strong ligamentous and capsular compo- The joint is considered to it. Posteriorly, the crest of the ilium ends nents. important because it to form the posterior superior iliac spine can affect the spine and (PSIS). With respect to surface anatomy, Postural alignment of the bones and joints pelvis proximally and the PSIS is often marked as a dimple in the of the hip plays a role in determining the femur and patella skin. Clinicians attempting to identify pelvic functional gait patterns and forces associ- distally. The biomechan- or hip subluxations, leg-length discrepancies, ated with various supporting structures. ics of this joint are often or postural faults during examinations use There is a relationship between the hip misunderstood, and the these landmarks. -

Role of Greater Sciatic Notch in Sexing Human Hip Bones
International Journal of Recent Trends in Science And Technology, ISSN 2277-2812 E-ISSN 2249-8109, Volume 7, Issue 3, 2013 pp 119-123 Role of Greater Sciatic Notch in Sexing Human Hip Bones Rajashree Sheelawant Raut 1*, Prakash B. Hosmani 2, P. R. Kulkarni 3 1Assistant Professor, Department of Anatomy, B. J. Government Medical College, Pune, Maharashtra, INDIA. 2Associate Professor, Department of Anatomy, Dr. V. M. Government Medical College, Solapur, Maharashtra, INDIA. 3 Professor and Head, Department of Anatomy, Government Medical College, Latur, Maharashtra, INDIA. *Corresponding Address: [email protected] Research Article Abstract: Identification of the deceased person from bones is the in archaeological collections that they cannot be used for most critical problem faced by anatomist, forensic science experts sex determination. When pubic material is not preserved, & anthropologists. Skeletal remains have been used for sexing the sex determinations must be made using other less individual as bones of the body are last to perish after death. Hip bone, especially t he greater sciatic notch is valuable in deformed diagnostic features. The greater sciatic notch is especially bones because it is highly sexually dimorphic, is resistant to valuable in such situations because it is highly sexually damage, and thus can often be scored in poorly preserved dimorphic, is resistant to damage, and thus can often be skeletons. In present study one hundred and eighty three adult hip scored in poorly preserved skeletons[3]. Many attempts bones of known sex (125 male and 58 female) are studied for have been made to describe sex differences in the sciatic various parameters of greater sciatic notch. -

Tension Free Femoral Hernia Repair with Plug Milivoje Vuković1, Nebojša Moljević1, Siniša Crnogorac2
Journal of Acute Disease (2013)40-43 40 Contents lists available at ScienceDirect Journal of Acute Disease journal homepage: www.jadweb.org Document heading doi: 10.1016/S2221-6189(13)60093-1 Tension free femoral hernia repair with plug Milivoje Vuković1, Nebojša Moljević1, Siniša Crnogorac2 1Clinical Center of Vojvodina, Clinic for Abdominal, Endocrine and Transplantation Surgery, Novi Sad, Serbia 2Clinical Center of Vojvodina, Emergency Center, Novi Sad, Serbia ARTICLE INFO ABSTRACT Article history: Objective: To investigate the conventional technique involves treatment of femoral hernia an Received 10 January 2012 approximation inguinal ligament to pectinealMethod: ligament. In technique which uses mesh closure for Received in revised form 15 March 2012 femoral canal without tissue tension. A prospective study from January 01. 2007-May Accepted 15 May 2012 30. 2009. We analyzed 1 042 patients with inguinal hernia, of which there were 83 patients with 86 Available online 20 November 2012 Result: femoral hernia. Femoral hernias were present in 7.96% of cases. Males were 13 (15.66%) and 70 women (84.34%). The gender distribution of men: women is 1:5.38. Urgent underwent 69 Keywords: (83%), and the 14 election (17%) patients. Average age was 63 years, the youngest patient was a Femoral hernia 24 and the oldest 86 years. Ratio of right: left hernias was 3.4:1. With bilateral femoral hernias % ( %) Mesh+plug Conclusions:was 3.61 of cases. In 7 patients 8.43 underwent femoral hernia repair with 9 Prolene plug. Hernioplasty The technique of closing the femoral canal with plug a simple. The plug is made from monofilament material and is easily formed. -

Surgical Management of Pelvic Ewing's Sarcoma in Children and Adolescents
ONCOLOGY LETTERS 14: 3917-3926, 2017 Surgical management of pelvic Ewing's sarcoma in children and adolescents HONGBIN FAN, ZHENG GUO, JUN FU, XIANGDONG LI, JING LI and ZHEN WANG Department of Orthopedic Surgery, Xi-Jing Hospital, The Fourth Military Medical University, Xi'an, Shaanxi 710032, P.R. China Received June 16, 2016; Accepted March 9, 2017 DOI: 10.3892/ol.2017.6677 Abstract. The present study describes a novel surgical strategy of life, with the median age at diagnosis ranging from 13 to used to treat immature pelvic Ewing's sarcoma (ES), one made 19 years (3). Pelvic ES accounted for 19.9% of cases in the possible owing to the intrinsic structure of the skeletally imma- Mayo Clinic series (4) and 21% in the chapter written by ture pelvis. A total of 12 children and adolescents with open Ginsberg et al (5), who discussed the principles and practice triradiate cartilage received limb-salvage surgeries following of ES. The numerous advances made in diagnostic imaging a diagnosis of pelvic ES. In total, 3 patients with iliac lesions and multimodality therapy over the past few decades mean (2 lesions with extension into the sacrum) received surgical that the overall 5-year survival rate of ES has increased from tumor excisions and allograft reconstructions. Another 10% in the 1970s (6) to 55-75% at the turn of the century (7). 8 patients with periacetabular lesions received trans-acetabular Studies have demonstrated that 5-year survival is improved osteotomies and allograft reconstructions. No reconstruction in patients treated with surgical resection and chemotherapy was performed on 1 patient following excision of a pubic lesion. -

Lab #23 Anal Triangle
THE BONY PELVIS AND ANAL TRIANGLE (Grant's Dissector [16th Ed.] pp. 141-145) TODAY’S GOALS: 1. Identify relevant bony features/landmarks on skeletal materials or pelvic models. 2. Identify the sacrotuberous and sacrospinous ligaments. 3. Describe the organization and divisions of the perineum into two triangles: anal triangle and urogenital triangle 4. Dissect the ischiorectal (ischioanal) fossa and define its boundaries. 5. Identify the inferior rectal nerve and artery, the pudendal (Alcock’s) canal and the external anal sphincter. DISSECTION NOTES: The perineum is the diamond-shaped area between the upper thighs and below the inferior pelvic aperture and pelvic diaphragm. It is divided anatomically into 2 triangles: the anal triangle and the urogenital (UG) triangle (Dissector p. 142, Fig. 5.2). The anal triangle is bounded by the tip of the coccyx, sacrotuberous ligaments, and a line connecting the right and left ischial tuberosities. It contains the anal canal, which pierced the levator ani muscle portion of the pelvic diaphragm. The urogenital triangle is bounded by the ischiopubic rami to the inferior surface of the pubic symphysis and a line connecting the right and left ischial tuberosities. This triangular space contains the urogenital (UG) diaphragm that transmits the urethra (in male) and urethra and vagina (in female). A. Anal Triangle Turn the cadaver into the prone position. Make skin incisions as on page 144, Fig. 5.4 of the Dissector. Reflect skin and superficial fascia of the gluteal region in one flap to expose the large gluteus maximus muscle. This muscle has proximal attachments to the posteromedial surface of the ilium, posterior surfaces of the sacrum and coccyx, and the sacrotuberous ligament. -

Approach to the Anterior Pelvis (Enneking Type III Resection) Bruno Fuchs, MD Phd & Franklin H.Sim, MD Indication 1
Approach to the Anterior Pelvis (Enneking Type III Resection) Bruno Fuchs, MD PhD & Franklin H.Sim, MD Indication 1. Tumors of the pubis 2. part of internal and external hemipelvectomy 3. pelvic fractures Technique 1. Positioning: Type III resections involve the excision of a portion of the symphysis or the whole pubis from the pubic symphysis to the lateral margin of the obturator foramen. The best position for these patients is the lithotomy or supine position. The patient is widely prepared and draped in the lithotomy position with the affected leg free to allow manipulation during the procedure. This allows the hip to be flexed, adducted, and externally rotated to facilitate exposure. 2. Landmarks: One should palpate the ASIS, the symphysis with the pubic tubercles, and the ischial tuberosity. 3. Incision: The incision may be Pfannenstiel like with vertical limbs set laterally along the horizontal incision depending on whether the pubic bones on both sides are resected or not. Alternatively, if only one side is resected, a curved incision following the root of the thigh may be used. This incision begins below the inguinal ligament along the medial border of the femoral triangle and extends across the medial thigh a centimeter distal to the inguinal crease and perineum, to curve distally below the ischium several centimeters (Fig.1). 4. Full thickness flaps are raised so that the anterior inferior pubic ramus is shown in its entire length, from the pubic tubercle to the ischial spine. Laterally, the adductor muscles are visualized, cranially the pectineus muscle and the pubic tubercle with the insertion of the inguinal ligament (Fig.2). -

Surgical Approaches to Fractures of the Acetabulum and Pelvis Joel M
Surgical Approaches to Fractures of the Acetabulum and Pelvis Joel M. Matta, M.D. Sponsored by Mizuho OSI APPROACHES TO THE The table will also stably position the ACETABULUM limb in a number of different positions. No one surgical approach is applicable for all acetabulum fractures. KOCHER-LANGENBECK After examination of the plain films as well as the CT scan the surgeon should APPROACH be knowledgeable of the precise anatomy of the fracture he or she is The Kocher-Langenbeck approach is dealing with. A surgical approach will primarily an approach to the posterior be selected with the expectation that column of the Acetabulum. There is the entire reduction and fixation can excellent exposure of the be performed through the surgical retroacetabular surface from the approach. A precise knowledge of the ischial tuberosity to the inferior portion capabilities of each surgical approach of the iliac wing. The quadrilateral is also necessary. In order to maximize surface is accessible by palpation the capabilities of each surgical through the greater or lesser sciatic approach it is advantageous to operate notch. A less effective though often the patient on the PROfx® Pelvic very useful approach to the anterior Reconstruction Orthopedic Fracture column is available by manipulation Table which can apply traction in a through the greater sciatic notch or by distal and/or lateral direction during intra-articular manipulation through the operation. the Acetabulum (Figure 1). Figure 2. Fractures operated through the Kocher-Langenbeck approach. Figure 3. Positioning of the patient on the PROfx® surgical table for operations through the Kocher-Lagenbeck approach.