Year Review of Patients on DOTS in Delta State, Nigeria
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

PRESS RELEASE June 25, 2021 for Immediate Release U.S. Embassy
United States Diplomatic Mission to Nigeria, Public Affairs Section Plot 1075, Diplomatic Drive, Central Business District, Abuja Telephone: 09-461-4000. Website at http://nigeria.usembassy.gov PRESS RELEASE June 25, 2021 For Immediate Release U.S. Embassy Abuja Partners Channels Academy to Train Conflict Reporters The U.S. Embassy Abuja, in partnership with Channels Academy, has trained over 150 journalists on Conflict Reporting and Peace Journalism. In her opening remarks, the U.S. Embassy Spokesperson/Press Attaché Jeanne Clark noted that the United States recognized that security challenges exist in many forms throughout the country, and that journalists are confronted with responsibility to prioritize physical safety in addition to meeting standards of objectivity and integrity in conflict. She urged the journalists to share their experiences throughout the course of the three-day seminar and encouraged participants to identify new ways to address these security challenges. The trainer Professor Steven Youngblood from the U.S. Center for Global Peace Journalism – Park University defined and presented principles for peace journalism in conflict reporting. He cautioned journalists to refrain from what he termed war journalism. He said, "war journalism is a pattern of media coverage that includes overvaluing violent, reactive responses to conflict while undervaluing non-violent, developmental responses.” The Provost of Channels Academy, Mr Kingsley Uranta, showed appreciation for the continuous partnership with the U.S. Embassy and for bringing such training opportunities to Nigerian journalists. He also called on conflict reporters to be peace ambassadors. The training took place virtually via Zoom on June 22 – 24, 2021. Journalists converged in American Spaces in Abuja, Kano, Bauchi Sokoto, Maiduguri, Awka, and Ibadan. -

A Study of Awka Metropolis Anambra State, Nigeria
International Journal of Business and Social Science Vol. 7, No. 5; May 2016 Urban Poverty Incidence in Nigeria: A Study of Awka Metropolis Anambra State, Nigeria Mbah, Stella I., Ph.D Department of Business Administration Chukwuemeka Odumegwu Ojukwu University Igbariam, Anambra State Nigeria Mgbemena, Gabriel C. Department of Business Administration Chukwuemeka Odumegwu Ojukwu University Igbariam, Anambra State Nigeria Ejike, Daniel C. Department of Business Administration Chukwuemeka Odumegwu Ojukwu University Igbariam, Anambra State Nigeria Abstract This study examined poverty situation in Awka metropolis of Anambra State, Nigeria, using the P-alpha class of poverty measure. To achieve this objective, a structured questionnaire was administered to 399 heads of households selected from mixed socio-economic backgrounds. The study revealed that 49 percent of the respondents were considered to be poor, with 0.17 poverty gap index and a 0.03 severity of poverty index. However, the indicators were considered to be modest when compared with the national rates. The causes of poverty in Awka metropolis include: lack or inadequate supply of some identified basic necessities of life such as shelter, potable water, and sanitation, basic healthcare services, electricity and educational services. As a result of these inadequacies, there are psychological distress, increase in destitution, child labour, violent crime, and prostitution. It was therefore recommended among others that government should step up public investment in urban infrastructure, provision of credit facilities, involvement of the people in development decision that affects their lives or participatory budgetary process and most especially, good governance at the municipal level with accountability and transparency to stamp out corrupt tendencies which has inhibited past developmental efforts of the government. -

Nigeria's Constitution of 1999
PDF generated: 26 Aug 2021, 16:42 constituteproject.org Nigeria's Constitution of 1999 This complete constitution has been generated from excerpts of texts from the repository of the Comparative Constitutions Project, and distributed on constituteproject.org. constituteproject.org PDF generated: 26 Aug 2021, 16:42 Table of contents Preamble . 5 Chapter I: General Provisions . 5 Part I: Federal Republic of Nigeria . 5 Part II: Powers of the Federal Republic of Nigeria . 6 Chapter II: Fundamental Objectives and Directive Principles of State Policy . 13 Chapter III: Citizenship . 17 Chapter IV: Fundamental Rights . 20 Chapter V: The Legislature . 28 Part I: National Assembly . 28 A. Composition and Staff of National Assembly . 28 B. Procedure for Summoning and Dissolution of National Assembly . 29 C. Qualifications for Membership of National Assembly and Right of Attendance . 32 D. Elections to National Assembly . 35 E. Powers and Control over Public Funds . 36 Part II: House of Assembly of a State . 40 A. Composition and Staff of House of Assembly . 40 B. Procedure for Summoning and Dissolution of House of Assembly . 41 C. Qualification for Membership of House of Assembly and Right of Attendance . 43 D. Elections to a House of Assembly . 45 E. Powers and Control over Public Funds . 47 Chapter VI: The Executive . 50 Part I: Federal Executive . 50 A. The President of the Federation . 50 B. Establishment of Certain Federal Executive Bodies . 58 C. Public Revenue . 61 D. The Public Service of the Federation . 63 Part II: State Executive . 65 A. Governor of a State . 65 B. Establishment of Certain State Executive Bodies . -

Purple Hibiscus
1 A GLOSSARY OF IGBO WORDS, NAMES AND PHRASES Taken from the text: Purple Hibiscus by Chimamanda Ngozi Adichie Appendix A: Catholic Terms Appendix B: Pidgin English Compiled & Translated for the NW School by: Eze Anamelechi March 2009 A Abuja: Capital of Nigeria—Federal capital territory modeled after Washington, D.C. (p. 132) “Abumonye n'uwa, onyekambu n'uwa”: “Am I who in the world, who am I in this life?”‖ (p. 276) Adamu: Arabic/Islamic name for Adam, and thus very popular among Muslim Hausas of northern Nigeria. (p. 103) Ade Coker: Ade (ah-DEH) Yoruba male name meaning "crown" or "royal one." Lagosians are known to adopt foreign names (i.e. Coker) Agbogho: short for Agboghobia meaning young lady, maiden (p. 64) Agwonatumbe: "The snake that strikes the tortoise" (i.e. despite the shell/shield)—the name of a masquerade at Aro festival (p. 86) Aja: "sand" or the ritual of "appeasing an oracle" (p. 143) Akamu: Pap made from corn; like English custard made from corn starch; a common and standard accompaniment to Nigerian breakfasts (p. 41) Akara: Bean cake/Pea fritters made from fried ground black-eyed pea paste. A staple Nigerian veggie burger (p. 148) Aku na efe: Aku is flying (p. 218) Aku: Aku are winged termites most common during the rainy season when they swarm; also means "wealth." Akwam ozu: Funeral/grief ritual or send-off ceremonies for the dead. (p. 203) Amaka (f): Short form of female name Chiamaka meaning "God is beautiful" (p. 78) Amaka ka?: "Amaka say?" or guess? (p. -

South – East Zone
South – East Zone Abia State Contact Number/Enquires ‐08036725051 S/N City / Town Street Address 1 Aba Abia State Polytechnic, Aba 2 Aba Aba Main Park (Asa Road) 3 Aba Ogbor Hill (Opobo Junction) 4 Aba Iheoji Market (Ohanku, Aba) 5 Aba Osisioma By Express 6 Aba Eziama Aba North (Pz) 7 Aba 222 Clifford Road (Agm Church) 8 Aba Aba Town Hall, L.G Hqr, Aba South 9 Aba A.G.C. 39 Osusu Rd, Aba North 10 Aba A.G.C. 22 Ikonne Street, Aba North 11 Aba A.G.C. 252 Faulks Road, Aba North 12 Aba A.G.C. 84 Ohanku Road, Aba South 13 Aba A.G.C. Ukaegbu Ogbor Hill, Aba North 14 Aba A.G.C. Ozuitem, Aba South 15 Aba A.G.C. 55 Ogbonna Rd, Aba North 16 Aba Sda, 1 School Rd, Aba South 17 Aba Our Lady Of Rose Cath. Ngwa Rd, Aba South 18 Aba Abia State University Teaching Hospital – Hospital Road, Aba 19 Aba Ama Ogbonna/Osusu, Aba 20 Aba Ahia Ohuru, Aba 21 Aba Abayi Ariaria, Aba 22 Aba Seven ‐ Up Ogbor Hill, Aba 23 Aba Asa Nnetu – Spair Parts Market, Aba 24 Aba Zonal Board/Afor Une, Aba 25 Aba Obohia ‐ Our Lady Of Fatima, Aba 26 Aba Mr Bigs – Factory Road, Aba 27 Aba Ph Rd ‐ Udenwanyi, Aba 28 Aba Tony‐ Mas Becoz Fast Food‐ Umuode By Express, Aba 29 Aba Okpu Umuobo – By Aba Owerri Road, Aba 30 Aba Obikabia Junction – Ogbor Hill, Aba 31 Aba Ihemelandu – Evina, Aba 32 Aba East Street By Azikiwe – New Era Hospital, Aba 33 Aba Owerri – Aba Primary School, Aba 34 Aba Nigeria Breweries – Industrial Road, Aba 35 Aba Orie Ohabiam Market, Aba 36 Aba Jubilee By Asa Road, Aba 37 Aba St. -

Fault Detection on Power System Transmission Line Using Artificial Neural Network (A Comparative Case Study of Onitsha – Awka – Enugu Transmission Line
American Journal of Engineering Research (AJER) 2019 American Journal of Engineering Research (AJER) e-ISSN: 2320-0847 p-ISSN : 2320-0936 Volume-8, Issue-4, pp-32-57 www.ajer.org Research Paper Open Access Fault Detection on Power System Transmission Line Using Artificial Neural Network (A Comparative Case Study of Onitsha – Awka – Enugu Transmission Line V. C. Ogboh1., E. C. Nwangugu2., A. E. Anyalebechi3 1Department of Electrical of Engineering, NnamdiAzikiwe University Awka.Anambra State Nigeria 2Department of Electrical of Engineering, NnamdiAzikiwe University Awka.Anambra State Nigeria 3Department of Electrical of Engineering, NnamdiAzikiwe University Awka.Anambra State Nigeria Corresponding Author; V. C. Ogboh ABSTRACT:This paper dwelt on the use of artificial neural network (ANN) method with Matlab Simulink 2016 to detect faults on the power system transmission line using Onitsha – Awka – Enugu as a cast study. The Onitsha - Awka – Enugu transmission line was modeled with Matlab Simulink 2016 using the transmission line pre-fault and daily fault data. Single line to ground (A – G), Double line to ground (AB – G), Line to line (A – B) and three phase (ABC) faults were simulated with the ANN method using Matlab Simulink 2016. However, the ANNshow detail detection and analysis of faults on the line. It was able to detect faults, classify them and locate thefault distance. The output results of the method where compared with the symmetrical component method (the conventional method). The comparison was done based on robustness/simplicity, less error, accuracy and efficiency. ANN was found the best in terms of the above comparative factors. KEYWORDS: Fast Fourier Transform, Wavelet Transform, Artificial Neural Network, Symmetrical Components, Travelling Wave. -

THE ARCHITECTURE of the URBAN FRONTS, the CASE of URBAN EXPERIENCE and PRESSURE on the INFRASTRUCTURE -- Bons N
Mgbakoigba, Journal of African Studies. Vol.7, No.2. June 2018 THE ARCHITECTURE OF THE URBAN FRONTS, THE CASE OF URBAN EXPERIENCE AND PRESSURE ON THE INFRASTRUCTURE -- Bons N. Obiadi, Nzewi, N.U. The Architecture of the Urban Fronts, the Case of Urban Experience and Pressure on the Infrastructure. Bons N. Obiadi Department of Architecture Nnamdi Azikiwe University, Awka and Nzewi, N.U. Department of Architecture Nnamdi Azikiwe University, Awka Abstract: A generalized perception of Architecture locates the discipline within the narrow boundaries of design and erection of buildings. While this may be acceptable in certain quarters, the fact remains that the spatial emergence and generic function guiding the relationship between human beings and space have, for centuries, guided the architecture of cities. Architecture, according to definitions, is practiced by licensed professionals in the industry however; literature has proven that almost everyone practices architecture in different ways and not, exclusively limiting to the design and erection of buildings. The dumping of communities solid wastes redefine the configuration of the area's environment and it is architectural, and deals with human beings and spaces. The design, construction and erection of roads, bridges and community street security gates are architectural and negatively impacting on the environment and particularly, architecture of the area. Objectively, the aim of this study is to create awareness and point to the fact, that the Nigerian players (policy makers) have in the past, designed models to direct positive growth and development in the country, but failed to properly implement the programmes and that is detrimental to the country's built environment and especially, architecture and infrastructure. -

A Case Study of Awka and Onitsha in Anambra State, Nigeria
Journal of Law, Policy and Globalization www.iiste.org ISSN 2224-3240 (Paper) ISSN 2224-3259 (Online) Vol.19, 2013 Urban Flooding and Vulnerability of Nigerian Cities: A Case Study of Awka and Onitsha in Anambra State, Nigeria Kingsley Efobi * Christopher Anierobi Department of Urban and Regional Planning, University of Nigeria, Enugu campus PMB 01129,Nigeria * E-mail of the corresponding author: [email protected] ABSTRACT The climate change phenomenon with its associated increase in global temperature, precipitation and rise in sea levels has also ushered in an increased frequency of flooding in recent times. In the year 2012, many Nigerian cities suffered from the ravaging effects of flooding. This led to lose of lives, internal displacements, destruction of properties, disruption of socio-economic, cultural and religious activities; and splintering of family ties. The cities of Awka and Onitsha in Anambra state, Nigeria featured among the vulnerable cities which are susceptible to flooding. This study set out to find out the causes of flooding in these cities with a view to recommending measures that will help ameliorate the situation. Direct observations and structured interview methods were used to acquire the needed primary data from residents of identified flood prone areas and in addition to secondary data obtained from official records of the State Ministry of Environment. The result revealed that although flooding gives the residents of Awka and Onitsha nightmares, especially during the rainy seasons; it had received only 15% of government intervention activities on environmental problems. There is gross inadequacy in the provision of drainage channels, coupled with poor designs, poor construction and blocked drainage channels. -

Christianity and Awka Socio-Religio-Cultural Identity Crisis: Areas of Conflict
CHRISTIANITY AND AWKA SOCIO-RELIGIO-CULTURAL IDENTITY CRISIS: AREAS OF CONFLICT Patrick Enoch Nmah http://dx.doi.org/10.4314/og.v12i s1.5 Abstract The problem of religious and cultural conflict still baffles many scholars of religion, sociology and anthropology. This article was designed to investigate and x-ray critically the religious values, beliefs and practices among the Awka people of Nigeria that were involved in the socio-religious conflict. Findings showed that the issues involved in the conflict were the Imo Awka festival, burial rites ( ikponye aja n’ili - dust-to-dust rite), and okuko onye uwa (hen sacrificed to family deity to validate a marriage bond). It was recommended among others that the church and Awka people should in the way of resolving conflict situation use the least expensive method without much acrimony. The main aim of this research was to shed some light on the consequences of this socio-religio-cultural conflict. The method applied in the research work was historio- phenomenological approach with the review of related literature. Introduction This article aims at articulating the socio-religious and cultural conflicts associated with Imoka festival, burial rites and okukoonyeuwa (hen sacrificed to idol) in Awka. There is the need to give accurate information that will correct the misinterpretation and misinformation going round in the Awka in respect of the three issues raised above. The significance of the research is that it will be useful for academic knowledge and practical aims. The method applied is historio-phenomenological approach. Related extant materials were used in the course of the research.In summary, what is being said is that every community has its own religion. -

Access Bank Branches Nationwide
LIST OF ACCESS BANK BRANCHES NATIONWIDE ABUJA Town Address Ademola Adetokunbo Plot 833, Ademola Adetokunbo Crescent, Wuse 2, Abuja. Aminu Kano Plot 1195, Aminu Kano Cresent, Wuse II, Abuja. Asokoro 48, Yakubu Gowon Crescent, Asokoro, Abuja. Garki Plot 1231, Cadastral Zone A03, Garki II District, Abuja. Kubwa Plot 59, Gado Nasko Road, Kubwa, Abuja. National Assembly National Assembly White House Basement, Abuja. Wuse Market 36, Doula Street, Zone 5, Wuse Market. Herbert Macaulay Plot 247, Herbert Macaulay Way Total House Building, Opposite NNPC Tower, Central Business District Abuja. ABIA STATE Town Address Aba 69, Azikiwe Road, Abia. Umuahia 6, Trading/Residential Area (Library Avenue). ADAMAWA STATE Town Address Yola 13/15, Atiku Abubakar Road, Yola. AKWA IBOM STATE Town Address Uyo 21/23 Gibbs Street, Uyo, Akwa Ibom. ANAMBRA STATE Town Address Awka 1, Ajekwe Close, Off Enugu-Onitsha Express way, Awka. Nnewi Block 015, Zone 1, Edo-Ezemewi Road, Nnewi. Onitsha 6, New Market Road , Onitsha. BAUCHI STATE Town Address Bauchi 24, Murtala Mohammed Way, Bauchi. BAYELSA STATE Town Address Yenagoa Plot 3, Onopa Commercial Layout, Onopa, Yenagoa. BENUE STATE Town Address Makurdi 5, Ogiri Oko Road, GRA, Makurdi BORNO STATE Town Address Maiduguri Sir Kashim Ibrahim Way, Maiduguri. CROSS RIVER STATE Town Address Calabar 45, Muritala Mohammed Way, Calabar. Access Bank Cash Center Unicem Mfamosing, Calabar DELTA STATE Town Address Asaba 304, Nnebisi, Road, Asaba. Warri 57, Effurun/Sapele Road, Warri. EBONYI STATE Town Address Abakaliki 44, Ogoja Road, Abakaliki. EDO STATE Town Address Benin 45, Akpakpava Street, Benin City, Benin. Sapele Road 164, Opposite NPDC, Sapele Road. -
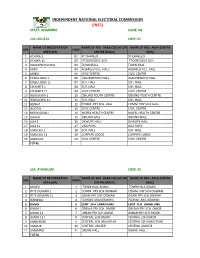
State: Anambra Code: 04
INDEPENDENT NATIONAL ELECTORAL COMMISSION (INEC) STATE: ANAMBRA CODE: 04 LGA :AGUATA CODE: 01 NAME OF REGISTRATION NAME OF REG. AREA COLLATION NAME OF REG. AREA CENTRE S/N CODE AREA (RA) CENTRE (RACC) (RAC) 1 ACHINA 1 01 ST CHARLED ST CHARLED 2 ACHINA 11 02 PTOGRESSIVE SCH. PTOGRESSIVE SCH. 3 AGULEZECHUKWU 03 TOWN HALL TOWN HALL 4 AKPO 04 AGBAELU VILL. HALL AGBAELU VILL. HALL 5 AMESI 05 CIVIC CENTRE CIVIC CENTRE 6 EKWULOBIA 1 06 UMUEZENOFO HALL. UMUEZENOFO HALL. 7 EKWULOBIA 11 07 SCH. HALL SCH. HALL 8 EZENIFITE 1 08 SCH. HALL SCH. HALL 9 EZENIFITE 11 09 CIVIC CENTRE CIVIC CENTRE 10 IGBOUKWU 1 10 OBIUNO YOUTH CENTRE OBIUNO YOUTH CENTRE 11 IGBOUKWU 11 11 SCH. HALL SCH. HALL 12 IKENGA 12 COMM. PRY SCH. HALL COMM. PRY SCH. HALL 13 ISUOFIA 13 CIVIC CENTRE CIVIC CENTRE 14 NKPOLOGWU 14 MOFEL HEALTH CENTRE MOFEL HEALTH CENTRE 15 ORAERI 15 OBIUNO HALL OBIUNO HALL 16 UGA 1 16 OKWUTE HALL OKWUTE HALL 17 UGA 11 17 UGA BOYS UGA BOYS 18 UMUCHU 1 18 SCH. HALL SCH. HALL 19 UMUCHU 11 19 CORPERS LODGE CORPERS LODGE 20 UMOUNA 20 CIVIC CENTRE CIVIC CENTRE TOTAL LGA: AYAMELUM CODE: 02 NAME OF REGISTRATION NAME OF REG. AREA COLLATION NAME OF REG. AREA CENTRE S/N CODE AREA (RA) CENTRE (RACC) (RAC) 1 ANAKU 1 TOWN HALL ANAKU TOWN HALL ANAKU 2 IFITE OGWARI 1 2 COMM. PRY SCH.OGWARI COMM. PRY SCH.OGWARI 3 IFITE OGWARI 11 3 OGARI PRY SCH.OGWARI OGARI PRY SCH.OGWARI 4 IGBAKWU 4 ISIOKWE ARA,IGBAKWU ISIOKWE ARA,IGBAKWU 5 OMASI 5 CENT. -

Performance Evaluation of Satellite-Based Rainfall Products Over Nigeria
climate Article Performance Evaluation of Satellite-Based Rainfall Products over Nigeria 1, , 2 3 Kingsley N. Ogbu * y , Nina Rholan Hounguè , Imoleayo E. Gbode and Bernhard Tischbein 1 1 Center for Development Research, University of Bonn, Genscherallee 3, D-53113 Bonn, Germany; [email protected] 2 Geography Institute, University of Bonn, Meckenheimer Allee 166, 53115 Bonn, Germany; [email protected] 3 Department of Meteorology and Climate Science, Federal University of Technology, 340252 Akure, Nigeria; [email protected] * Correspondence: [email protected] or [email protected] Current address: Department of Agricultural and Bioresources Engineering, Faculty of Engineering, y Nnamdi Azikiwe University, 420221 Awka, Nigeria. Received: 15 August 2020; Accepted: 22 September 2020; Published: 24 September 2020 Abstract: Understanding the variability of rainfall is important for sustaining rain-dependent agriculture and driving the local economy of Nigeria. Paucity and inadequate rain gauge network across Nigeria has made satellite-based rainfall products (SRPs), which offer a complete spatial and consistent temporal coverage, a better alternative. However, the accuracy of these products must be ascertained before use in water resource developments and planning. In this study, the performances of Climate Hazards Group Infrared Precipitation with Station data (CHIRPS), Precipitation estimation from Remotely Sensed Information using Artificial Neural Networks–Climate Data Record (PERSIANN-CDR), and Tropical Applications of Meteorology using SATellite data and ground-based observations (TAMSAT), were evaluated to investigate their ability to reproduce long term (1983–2013) observed rainfall characteristics derived from twenty-four (24) gauges in Nigeria. Results show that all products performed well in terms of capturing the observed annual cycle and spatial trends in all selected stations.