COVID-19: SEL System Recovery Plan Lewisham Borough
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

London Borough of Lewisham Catford Retail and Economic Impact Assessment Final Report for Consultation
Peter Brett Associates LLP 16 Brewhouse Yard London EC1V 4LJ t: 020 7566 8600 London Borough of Lewisham Catford Retail and Economic Impact Assessment Final Report for Consultation Final Report for Consultation January 2013 Peter Brett Associates LLP disclaims any responsibility to the Client and others in respect of any matters outside the scope of this report. This report has been prepared with reasonable skill, care and diligence within the terms of the Contract with the Client and generally in accordance with the appropriate ACE Agreement and taking account of the manpower, resources, investigations and testing devoted to it by agreement with the Client. This report is confidential to the Client and Peter Brett Associates LLP accepts no responsibility of whatsoever nature to third parties to whom this report or any part thereof is made known. Any such party relies upon the report at their own risk. © Peter Brett Associates LLP 2013 Job Number 27149-001 CONTENTS EXECUTIVE SUMMARY ..................................................................................................... i-iv 1 INTRODUCTION .................................................................................................................... 1 Terms of reference ................................................................................................................. 1 Challenges for Catford ........................................................................................................... 3 Structure of report ................................................................................................................. -

Working Together to Tackle Poverty in Lewisham
Working together to tackle poverty in Lewisham The final report of the Lewisham Poverty Commission October 2017 Contents Foreword 3 1. Introducing the Poverty Commission: a realistic but ambitious approach 4 The Commission 4 Focusing on poverty 4 The role of Lewisham Council in tackling poverty 5 Action at a local level 5 Working together to tackle poverty 5 2. Poverty in Lewisham 6 Lewisham and its people 6 The impacts of poverty 6 Quantifying poverty in Lewisham 8 The difficulties in getting well-paid, secure work 10 Children living in poverty 13 The price of unaffordable housing 14 The Commission’s focus 14 3. Supporting residents to access well-paid, secure jobs inside and outside of Lewisham 15 Works, skills and the role of anchor institutions 15 Recommendations 17 4. Tackling child poverty by supporting parents into decent work 20 Child poverty, child care and lone parent unemployment 20 Recommendations 21 5. Improving the local housing market 23 Housing in Lewisham 23 Recommendations 24 6. Strengthening support within communities 27 Increasing community resilience 27 Recommendations 29 7. Working together to tackle poverty: next steps and implementation 31 An immediate response 31 Change across the community 31 Advising national government 31 Staying the course 31 Appendix 1: Listening to Lewisham’s people and its organisations 32 Our approach to consultation and engagement 32 Further data and evidence 33 Summary of comments received from residents 34 2 Foreword Lewisham is a great place to live, with a strong and diverse community. Yet, despite being situated in the heart of London, on the doorsteps of one of the wealthiest cities in the world, tens of thousands of Lewisham residents live in poverty. -
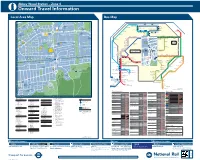
Abbey Wood Station – Zone 4 I Onward Travel Information Local Area Map Bus Map
Abbey Wood Station – Zone 4 i Onward Travel Information Local Area Map Bus Map 45 1 HARTSLOCK DRIVE TICKFORD CLOSE Y 1 GROVEBURY ROAD OAD 16 A ALK 25 River Thames 59 W AMPLEFORTH R AMPLEFORTH ROAD 16 Southmere Central Way S T. K A Crossway R 1 B I N S E Y W STANBROOK ROAD TAVY BRIDGE Linton Mead Primary School Hoveton Road O Village A B B E Y W 12 Footbridge T H E R I N E S N SEACOURT ROAD M E R E R O A D M I C H A E L’ S CLOSE A S T. AY ST. MARTINS CLOSE 1 127 SEWELL ROAD 1 15 Abbey 177 229 401 B11 MOUNTJOYCLOSE M Southmere Wood Park ROAD Steps Pumping GrGroroovoveburyryy RRoaadd Willow Bank Thamesmead Primary School Crossway Station W 1 Town Centre River Thames PANFIE 15 Central Way ANDW Nickelby Close 165 ST. HELENS ROAD CLO 113 O 99 18 Watersmeet Place 51 S ELL D R I V E Bentham Road E GODSTOW ROAD R S O U T H M E R E L D R O A 140 100 Crossway R Gallions Reach Health Centre 1 25 48 Emmanuel Baptist Manordene Road 79 STANBROOK ROAD 111 Abbey Wood A D Surgery 33 Church Bentham Road THAMESMEAD H Lakeside Crossway 165 1 Health Centre Footbridge Hawksmoor School 180 20 Lister Walk Abbey Y GODSTOW ROAD Footbridge N1 Belvedere BUR AY Central Way Wood Park OVE GROVEBURY ROAD Footbridge Y A R N T O N W Y GR ROAD A Industrial Area 242 Footbridge R Grasshaven Way Y A R N T O N W AY N 149 8 T Bentham Road Thamesmead 38 O EYNSHAM DRIVE Games N Southwood Road Bentham Road Crossway Crossway Court 109 W Poplar Place Curlew Close PANFIELD ROAD Limestone A Carlyle Road 73 Pet Aid Centre W O LV E R C O T E R O A D Y 78 7 21 Community 36 Bentham Road -

Planning Application Design & Access Statement Van-0387
PLANNING APPLICATION DESIGN & ACCESS STATEMENT VAN-0387 53 PERRY VALE, FOREST HILL, LONDON, SE23 2NE SEPTEMBER 2018 1.0 Contents VAN-0387 – 53 Perry Vale, Forest Hill, SE23 2NE, London Borough of Lewisham Design and Access Statement, July 2018 1.0 Contents 1 2.0 Introduction 2 3.0 Site analysis and Current Building 5 4.0 Description of the proposal 7 5.0 Use and Layout 10 6.0 Heritage Statement 12 7.0 Planning History and Policies 15 8.0 Architectural Character and Materials 15 9.0 Landscaping and Trees 19 10.0 Ecology 19 11.0 Extract, Ventilation and Services 20 12.0 Cycle Storage and Refuse 20 13.0 Sustainability and Renewable Energy Technology 21 14.0 Access & Mobility Statement 21 15.0 Transport, Traffic and parking Statement 22 16.0 Acoustics 22 17.0 Flood Risk 22 18.0 Statement of Community Engagement 23 19.0 Conclusion 24 1 2.0 Introduction VAN-0387 – 53 Perry Vale, Forest Hill, SE23 2NE, London Borough of Lewisham Design and Access Statement, July 2018 This application submission is prepared by db architects on behalf of Vanquish Iconic Developments for the site at 53 Perry Vale, Forest Hill, SE23 2NE. Vanquish are a family-run business and have been creating urban industrial interior designed developments for many years now across South East London. "We are a firm believer that property development should be creative, not made with basic materials to fit the standard criteria of a build. This is reflected in our interiors and exteriors of each finished development. -

Local Government Boundary Commission for England
LOCAL GOVERNMENT BOUNDARY COMMISSION FOR ENGLAND REVIEW OF GREATER LONDON, THE LONDON BOROUGHS AND THE CITY OF LONDON THE BOUNDARIES OF THE LONDON BOROUGHS OF BROMLEY, CROYDON, LAMBETH, LEWISHAM, AND SOUTHWARK IN THE VICINITY OF CRYSTAL PALACE. REPORT NO. 632 LOCAL GOVERNMENT BOUNDARY COMMISSION FOR ENGLAND REPORT NO 632 LOCAL GOVERNMENT BOUNDARY COMMISSION FOR ENGLAND CHAIRMAN SIR GEOFFREY ELLERTON CMG MBE MEMBERS MR K F J ENNALS CB MR G R PRENTICE MRS H R V SARKANY MR C W SMITH PROFESSOR K YOUNG SECRETARY OF STATE FOR THE ENVIRONMENT REVIEW OF GREATER LONDON, THE LONDON BOROUGHS AND THE CITY OF LONDON THE BOUNDARIES OF THE LONDON BOROUGHS OF BROMLEY, CROYDON, LAMBETH, LEWI SHAM AND SODTHWARK IN THE VICINITY OF CRYSTAL PALACE COMMISSION'S FINAL REPORT AND PROPOSALS INTRODUCTION 1. On 1 April 1987 we announced the start of the review of Greater London, the London Boroughs and the City of London, as part of the programme of reviews we are required to undertake by virtue of section 48(1) of the Local Government Act 1972. We wrote to each of the local authorities concerned. 2. Copies of our letter were sent to the appropriate county, district and parish councils bordering Greater London; the local authority associations; Members of Parliament with constituency interests; and the headquarters of the main political parties. In addition, copies were sent to the Metropolitan Police and to those government departments, regional health authorities, electricity, gas and water undertakings which might have an interest, as well as local television and radio stations serving the Greater London area and to a number of other interested persons and organisations. -

The Constitution of the London Borough of Lewisham Under Section 9P Local Government Act 2000
London Borough of Lewisham Constitution Approved 26 May 2021 Published 2 CONTENTS Page Nos. PART I SUMMARY 14 PART II ARTICLES 22 Article 1 Aims and Purposes 23 Article 2 Councillors and Elections 23 Article 3 Citizens and the Council 25 Article 4 The Council 26 Article 5 Chairing the Council 29 Article 6 Overview and Scrutiny 30 Article 7 The Executive 45 Article 8 Conflict Resolution 49 Article 9 Committees 49 Article 10 Local Choice 63 Article 11 Ethics 63 Article 12 Local Assemblies/Positive Ageing Council/Public Transport Liaison Forum 64 Article 13 Joint arrangements 66 Article 14 Staff 67 Article 15 Delegating decision making 72 Article 16 Principles of decision making Including Key Decisions 72 Article 17 Finance, Contract and Legal Matters 76 Article 18 Representation & Appeal Panels 77 Article 19 SACRE 78 Article 20 Schools forum 78 Article 21 Young mayor 78 Article 22 Review of Constitution 78 Article 23 Publication, Interpretation, Suspension 79 PART III LOCAL CHOICE FUNCTIONS 81 PART IV PROCEDURE RULES – STANDING ORDERS 85 A. PURPOSE 86 B. COUNCILLORS 86 1. Term of office 86 2. Entitlement to speak and vote 86 3. Resignation 86 4. Vacation of office for non-attendance 86 5. Qualifying attendance 86 3 6. Vacation of office – executive 87 7. Qualifying attendance – executive 87 8. Declaration of vacancy 87 9. Filling of casual vacancy 87 10. Period of office 88 11. Declaration of acceptance of office 88 12. Declaration of interests 88 C COUNCIL PROCEDURE RULES 89 1 Types of meeting 89 2 Annual meeting 89 (1) Where and when -

37 Brockley Rise, Forest Hill London, Se23 1Jg
37 BROCKLEY RISE, FOREST HILL LONDON, SE23 1JG PROMINENT RETAIL PREMISES TO LET 68.22 SQ. M. (734 SQ. FT.) RENT: £15,000 PER ANNUM EXCLUSIVE Location The premises are situated on Brockley Road (B218) directly linking the South Circular with New Cross Road (A2) and Lewisham Way (A20). Forest Hill continues to grow in popularity with an ever improving selection of independent retailers, cafes and restaurants. Honor Oak Park station is within walking distance which provides regular Overground (East London Line) and National Rail (Southern) services into Central London with the area well served by local buses. Description The property is arranged over ground floor with rear Kitchen and W/C facilities and benefits from a wide frontage and rear yard. Accommodation The property has the following approximate net internal areas: Ground: 57.43 sq. m. (618 sq. ft.) Kitchen: 10.79 sq. m. (116 sq. ft.) Total: 68.22 sq. m. (734 sq. ft.) Terms The property is to be let on a new full repairing and insuring lease for a term to be agreed. Rates The property is yet to be assessed. Interested parties should contact the local authority to confirm rates payable. Planning We understand the property may be used for A1 retail purposes with potential for A2 and A3 uses. However, the ingoing tenant must make their own enquiries of the planning authority to ensure that the proposed use is permissible prior to entering into any form of contract. Rent £15,000 per annum exclusive. Legal Costs & VAT Each party to pay their own legal fees. -

Deptford & New Cross
Lewisham’s unrivalled location, connectivity, talents and development opportunities make it the gateway to London’s prosperity. Deptford & Investment-ready with a confirmed pipeline of infrastructure, housing and New Cross commercial delivery, Lewisham will be one of the fastest growing parts of the London economy by 2027. The borough is determined to deliver sustainable character-led development to maintain Lewisham’s identity as the best place for present and future generations to live, work and learn in London. With 1,000 homes being built over 4 years, the needs of all residents are being catered for. Our assets ensure excellent value for businesses seeking a base in the capital and promote growth in the high-value, knowledge-based economy. Lewisham’s cultural, heritage and artistic assets attract a vibrant and aspirational population. More than 70 nationalities are represented with more than 170 languages spoken. A London Borough of Lewisham Lewisham Council Initiative About Visit www.lewisham.london Visit www.lewisham.london A2 Developments Development Status Sector BLACKHEATH Lewisham London Completed Commercial Deptford & New Cross On Site ResidentialMixed Use Millwall FC DEPTFORD 15 Pipeline Mixed Use A213 14 RIVER THAMES Retail Deptford Market ASYLUM 5 8 17 NEW CROSS 12 Public Realm 6 New Cross Road SOUTHWARK 7 9 18 1 2 Key developments 10 NEW CROSS ROAD 16 11 DEVELOPMENT DEVELOPER/OWNER STATUS 3 Deptford Project inc Lewisham Council, U+I Plc Completed 4 1 13 Deptford Market Yard A2 A2 2 Deptford Lounge Lewisham Council Completed -

Greennews Lewisham Deptford.Cdr
Lewisham Deptford Green Party News and views from the Green Party. Delivered to over 30,000 green news homes in Lewisham & Deptford. Autumn/ Winter 2007 www.lewishamgreens.org.uk Darren Johnson - working for you Lewisham councillor and Green Assembly Member, Darren Johnson, is bidding to be your local MP at the next General Election. Darren says, “I care about protecting our environment, care about making life fairer, and care about Lewisham. Greens have made a real difference on Lewisham Council and on the London Assembly. It's now Darren Johnson time for a Green MP.” Green London Assembly Member In election after election Greens have proved to be the only real alternative to Labour and Lewisham Councillor in Lewisham Deptford. Greens now have six councillors in the Lewisham Deptford seat. Labour have 11, the Lib-Dems 2, Others 2 and the Conservatives none at all! To support Darren's campaign contact [email protected] or phone 020 8694 9524. The state of the parties in Lewisham Deptford - 2006 Local Election results Labour (37%) Jenny Jones Green London Assembly Member Green (27%) Liberal Democrat (17%) Conservative (12%) Other (7%) Jean Lambert London's Green MEP Only Greens can beat Labour in Lewisham Deptford! Contact us if you'd like to hear more Join I can help deliver Green News in my street/estate I'd like more information about the Green Party The I'd like to make a donation to the Green Party name Greens address - postcode call 020 telephone email PLEASE RETURN TO: 202 Malpas Road, London SE4 1DH 8694 9524 email: [email protected] or call us on 020 8694 9524 Information on this form will be kept private and used only for Green Party contact. -

Buses from Old Kent Road
Buses from Old Kent Road 168 Newington Green 21 78 Belsize Park Hampstead Heath 453 Royal Free Hospital Shoreditch Marylebone Hoxton Church Chalk Farm 63 Baring Street King's Cross Moorfields Camden Town for St. Pancras International Liverpool Street Baker Street Eye Hospital for Madame Tussauds Mount Pleasant Euston Old Street CITY Eversholt Street Farringdon Aldgate Regent's Park Moorgate Tower Gateway Russell Square St. Paul's Finsbury Square Cathedral St. Paul's for Fenchurch Street , Tower Hill , Tower Millenium Pier 172 Bank and Tower of London Great Portland Street Holborn Ludgate Circus Route fi nder for City Thameslink Monument River Thames Oxford Circus Blackfriars Fleet Tower Bridge ROTHERHITHE Day buses including 24-hour routes Street City Hall Southwark Jamaica Road Jamaica Road Jamaica Road Rotherhithe Bus route Towards Bus stops Piccadilly Circus Aldwych Street Crucifix Lane Tanner Street Dockhead Abbey Street St.James's Road Bermondsey Tunnel Entrance Rotherhithe for Covent Garden and London London Bridge Tower Bridge Road Lewisham Transport Museum Blackfriars Road for Guy's Hospital and Druid Street Canada 21 Regent Street Southwark Street the London Dungeon Jamaica Road Lower Road Water Newington Green Tower Bridge Road Southwark Park Road Southwark Park Salter Road Stamford Street Abbey Street Kirby Estate Trafalgar Square BERMONDSEY 24 hour for Charing Cross Plumshead Tower Bridge Road Southwark Park Road 53 service and National Gallery Surrey Quays Redriff Road Waterloo Caledonian Market Stalham Street Leisure Park for IMAX Cinema, London Eye Borough Rotherhithe Whitehall and South Bank Arts Complex Police Station 53 Grange Road Southwark Park Road Whitehall Spa Road Southwark Park Road Honor Oak Anchor Street Surrey Quays 63 Horse Guards Southwark Great Dover Street Raymouth Road Shopping Centre Parade Old Vic The Roebuck Theatre Grange Road St. -

Monday 11 to Friday 15 January Saturday 16 and Sunday 17 January
Changes to train times This week Monday 11 to Friday 15 January A reduced train timetable is in operation as a result of the coronavirus lockdown, and will be amended by late night engineering work. Please check before you travel, using the online journey planners. Deal/Minster to Ramsgate Blackheath to Dartford via Charlton In order to maintain timetable frequency, an additional bus service will As a result of late night engineering work between the above stations, the As a result of late night engineering work between the above stations, the operate between Lewisham and Dartford via Charlton and Woolwich following train services are revised: following train services are revised: Arsenal: departing from Lewisham at 0010 (Tuesday to Friday only) • 2240 (Wednesday & Thursday only) Charing Cross to Ramsgate via • 0012 (Thursday & Friday only) Charing Cross to Dartford via Lewisham calling at Blackheath 0018, Charlton 0030, Woolwich Dockyard 0035, Dover Priory train is revised to terminate at Dover Priory at 0035; with and Woolwich Arsenal; Woolwich Arsenal 0041, Plumstead 0045, Abbey Wood 0051, Belvedere a connecting replacement bus service to Ramsgate, departing Dover • 0015 (Tuesday & Wednesday only) Cannon Street to Dartford via 0055, Erith 0100, Slade Green 0106 and terminates Dartford at 0117. Priory at 0050 (Thursday & Friday only), calling to set down passengers Lewisham and Woolwich Arsenal; at Martin Mill, Walmer, Deal and Sandwich and terminating at • 0042 (Thursday & Friday only) Charing Cross to Dartford via Lewisham Victoria -

Sydenham Thorpes Conservation Area Character Appraisal Part 2
1 History of the area Location and surrounded by suburban sprawl dating principally from the 19th population and 20th centuries, punctuated by The conservation area is situated substantial open spaces at Bell in Lower Sydenham between Green to the west and at Crystal Sydenham Road (the A212) and Palace, New Beckenham and Mayow Park. Its boundary, shown Dulwich outside the Borough of in Figure 1, is tightly drawn Lewisham. The local topography around the six roads comprising is undulating, and the site slopes the Thorpes Estate, an Edwardian uphill from south to north, away development on the site of the from Sydenham Road. The former garden of the Old House, population of the area is which stood next to Sydenham estimated to be about 770. Road until the early 20th century. The boundary encloses a compact Origins and area with a strong individual identity, both historically and in development terms of the modern townscape. of the area The name Sydenham (early The regional context of the variations of which include conservation area is shown in Sypenham, Sibbenham and Figure 2. To the west is the railway Cippenham) is possibly derived line and Sydenham Station and to from the Anglo-Saxon ‘Cippas’ the north Mayow Park. The area is settlement’, meaning the drunkard’s settlement. During the 6th century the then heavily forested area along the banks of the River Pool was cleared by Saxon or Jutish farmers moving south from Lewisham and the Thames. These colonisers settled on high ground near the river at Perry Hill, Bell Green and the eastern end of Sydenham Road.