FINAL CA Midwives Common Pregnancy Concerns.Pptx
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Original Bilberry Extract
® The original bilberry extract. These statements may not comply with your country’s laws and regulations or with Reg. EC n. 1924/2006 and have not been evaluated by the Food and Drug Administration. The products are not intended to diagnose, treat, cure or prevent any disease. Marketers of finished products containing this ingredient are responsible for ensuring compliance with the applicable legal framework. C90 M70 Y0 K0 NERO 100% 1. Indena: beyond quality, naturally There is a substantial amount of evidence supporting the strong connection between health and nutrition. Life expectancy is continuously increasing together with a higher attention to quality, this becoming a key factor for both consumers and the food industry. 2 Consumers are more and more aware of what is contained in food, they look for safe and effective ingredients and the presence of available evidence supporting new ingredients offered in terms of benefi ts and safety of their dietary supplementation may heavily infl uence their buying decision. On the other hand, the food industry is expected to meet consumer demands, bringing to the market safe and effective products containing safe and certifi ed ingredients. Natural products in various forms have been used all over the world since time immemorial for the treatment of pathological conditions or for health 1 benefi ts. Plants represent a rich source of new active principles and 1 Bombardelli E., Bombardelli V., botanical extracts can be used in different markets including health Twenty years experience in the foods and supplements. The overall quality is essential, together with botanical health food market, Fitoterapia 76, 495-507, 2006. -

Huckleberry Picking at Priest Lake
HUCKLEBERRY (Vaccinium Membranaceum) USDA Forest Service Other Common Names Northern Region Blueberry, Big Whortleberry, Black Idaho Panhandle Huckleberry, Bilberry. National Forests Description: The huckleberry is a low erect shrub, ranging from 1-5' tall. The flowers are shaped like tiny pink or white urns, which blossom in June and July, depending on elevation. The leaves are short, elliptical and alter- native on the stems. The bush turns brilliant red and sheds its leaves in the fall. The stem bark is reddish (often yellowish-green in shaded sites). The shape of the berry varies The United States Department of Agriculture (USDA) from round to oval and the color var- prohibits discrimination in its programs on the basis ies from purplish black to wine- of race, color, national origin, sex, religion, age, disa- colored red. Some species have a bility, political beliefs, and marital or familial status. dusky blue covering called bloom. (Not all prohibited bases apply to all programs.) Per- The berries taste sweet and tart, in sons with disabilities who require alternative means the same proportions. of communication of program information (braille, large print, audiotape, etc.) should contact USDA's Ripening Season: July-August TARGET Center at (202) 720-2600 (voice and TDD). Early in the season, by mid-July, the berries on sunny southern facing To file a complaint, write the Secretary of Agriculture, Huckleberry slopes and lower elevations are first U.S. Department of Agriculture, Washington, DC to ripen. They are most succulent in 20250, or call 1-800-795-3272 (voice) or 202-720- mid-summer. However, good pick- 6382 (TDD). -

What to Eat on the Autoimmune Protocol
WHAT TO EAT ON THE AUTOIMMUNE PROTOCOL All the foods listed here are great to include in your It’s time to create an epidemic of - health. And it starts with learning ents that will help regulate your immune system and how to eat more nutrient-dense food. your hormones and provide the building blocks that your body needs to heal. You don’t need to eat all of these foods (it’s okay if snails, frog legs, and crickets aren’t your thing, and it’s okay if you just can’t get kangaroo meat or mizuna), but the idea is both to give Poultry innovative ways to increase variety and nutrient density • chicken • grouse • pigeon by exploring new foods. • dove • guinea hen • quail • duck • ostrich • turkey • emu • partridge (essentially, Red Meat • goose • pheasant any bird) • antelope • deer • mutton • bear • elk • pork • beaver • goat • rabbit • beef • hare • sea lion • • horse • seal • boar • kangaroo • whale • camel • lamb (essentially, • caribou • moose any mammal) Amphibians and Reptiles • crocodile • frog • snake • turtle 1 22 Fish* Shellfish • anchovy • gar • • abalone • limpet • scallop • Arctic char • haddock • salmon • clam • lobster • shrimp • Atlantic • hake • sardine • cockle • mussel • snail croaker • halibut • shad • conch • octopus • squid • barcheek • herring • shark • crab • oyster • whelk goby • John Dory • sheepshead • • periwinkle • bass • king • silverside • • prawn • bonito mackerel • smelt • bream • lamprey • snakehead • brill • ling • snapper • brisling • loach • sole • carp • mackerel • • • mahi mahi • tarpon • cod • marlin • tilapia • common dab • • • conger • minnow • trout • crappie • • tub gurnard • croaker • mullet • tuna • drum • pandora • turbot Other Seafood • eel • perch • walleye • anemone • sea squirt • fera • plaice • whiting • caviar/roe • sea urchin • • pollock • • *See page 387 for Selenium Health Benet Values. -

CASCADE BILBERRY Decorated with Bear Grass and Bitter Cherry Bark
Plant Guide baskets include "Klikitat baskets" of cedar root CASCADE BILBERRY decorated with bear grass and bitter cherry bark. Each family would harvest and store approximately Vaccinium deliciosum Piper four or five pecks (ca. four to five gallons) of dried Plant Symbol = VADE berries for winter use (Perkins n.d. (1838-43), Book 1:10). Hunn (1990) estimates that there were 28-42 Contributed by: USDA NRCS National Plant Data huckleberry harvest days in a year. This resulted in a Center & Oregon Plant Materials Center total annual harvest of 63.9-80.2 kg/woman/year from the Tenino-Wishram area, and 90 kg/woman/year from the Umatilla area. The net result was a huckleberry harvest yield of 31 kcal/person/day in the Tenino-Wishram area and 42 kcal/person/day for the Umatilla area (Hunn 1981: 130-131). Vaccinium species contain 622 Kcal per 100 gm huckleberries, with 15.3 gm carbohydrate, 0.5 gm fat, 0.7 gm protein and 83.2 gm water (Hunn 1981:130-131). In the fall, after the harvest, it was common for the Sahaptin to burn these areas to create favorable habitat (Henry Lewis 1973, 1977). Fire creates sunny openings in the forest and edges that foster the rapid spread of nutritious herbs and shrubs that favors the huckleberries (Minore 1972:68). The leaves and berries are high in vitamin C. The Jeanne Russell Janish leaves and finely chopped stems contain quinic acid, Used with permission of the publishers © Stanford University a former therapeutic for gout said to inhibit uric acid Abrams & Ferris (1960) formation but never widely used because of mixed clinical results. -

Biocidin Throat Spray – Scientific Validation of Ingredients
Biocidin Throat Spray – Scientific Validation of Ingredients Bilberry extract (Vaccinium myrtillus) Medicinal Actions: Antiinflammatory, antimicrobial, antioxidant, urinary antiseptic.1-3 Scientific Evidence: Bilberry is rich in phenolic compounds which possess bacteriostatic and antimicrobial properties.4 This herb is renowned for its exceptionally high levels of anthocyanins, which are responsible for bilberry’s diverse antioxidant effects.5,6 As a natural antiinflammatory agents, bilberry polyphenols help reduce lipopolysaccharide (LPS)-induced nuclear factor kappa-beta (NF-Kβ) activation.7 Based on in vitro research, bilberry possesses antiadhesive and antimicrobial properties against the respiratory-associated pathogens Streptococcus pneumoniae and Neisseria meningitidis.8 Bilberry extract may also help protect against dental plaque by inhibiting biofilm formation of common oral bacteria including Streptococcus mutans, Fusobacterium nucleatum and Actinomyces naeslundii.9 In vitro trials also show that bilberry is able to inhibit the replication of several respiratory viruses including coxsackie virus B1 (CV-B1), human respiratory syncytial virus A2 (HRSV-A2) and influenza virus A/H3N2.10 Safety Summary: Considered safe at the recommended dose.1 No adverse effects expected during pregnancy and breastfeeding.2 Noni (Morinda citrifolia) Medicinal Actions: Antiinflammatory, antimicrobial, antioxidant.3,11 Scientific Evidence: To date, over 160 different phytochemical compounds have been identified in the noni plant. The major secondary metabolites include phenolic compounds, organic acids and alkaloids which give rise to noni’s potent antioxidant and antiinflammatory properties.11 In vitro research has shown that noni is highly effective at inhibiting hydroxyl radicals which are known to cause oxidative damage to proteins, lipids and deoxyribonucleic acid (DNA).11 Noni has also been shown to decrease nitric oxide production. -
Chapter 1 Definitions and Classifications for Fruit and Vegetables
Chapter 1 Definitions and classifications for fruit and vegetables In the broadest sense, the botani- Botanical and culinary cal term vegetable refers to any plant, definitions edible or not, including trees, bushes, vines and vascular plants, and Botanical definitions distinguishes plant material from ani- Broadly, the botanical term fruit refers mal material and from inorganic to the mature ovary of a plant, matter. There are two slightly different including its seeds, covering and botanical definitions for the term any closely connected tissue, without vegetable as it relates to food. any consideration of whether these According to one, a vegetable is a are edible. As related to food, the plant cultivated for its edible part(s); IT botanical term fruit refers to the edible M according to the other, a vegetable is part of a plant that consists of the the edible part(s) of a plant, such as seeds and surrounding tissues. This the stems and stalk (celery), root includes fleshy fruits (such as blue- (carrot), tuber (potato), bulb (onion), berries, cantaloupe, poach, pumpkin, leaves (spinach, lettuce), flower (globe tomato) and dry fruits, where the artichoke), fruit (apple, cucumber, ripened ovary wall becomes papery, pumpkin, strawberries, tomato) or leathery, or woody as with cereal seeds (beans, peas). The latter grains, pulses (mature beans and definition includes fruits as a subset of peas) and nuts. vegetables. Definition of fruit and vegetables applicable in epidemiological studies, Fruit and vegetables Edible plant foods excluding -
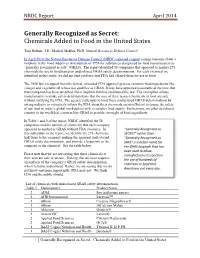
NRDC: Generally Recognized As Secret
NRDC Report April 2014 Generally Recognized as Secret: Chemicals Added to Food in the United States Tom Neltner, J.D., Maricel Maffini, Ph.D. Natural Resources Defense Council In April 2014, the Natural Resources Defense Council (NRDC) released a report raising concerns about a loophole in the Food Additives Amendment of 1958 for substances designated by food manufacturers as “generally recognized as safe” (GRAS). The report identified 56 companies that appeared to market 275 chemicals for use in food based on undisclosed GRAS safety determinations. For each chemical we identified in this study, we did not find evidence that FDA had cleared them for use in food. The 1958 law exempted from the formal, extended FDA approval process common food ingredients like vinegar and vegetable oil whose use qualifies as GRAS. It may have appeared reasonable at the time, but that exemption has been stretched into a loophole that has swallowed the law. The exemption allows manufacturers to make safety determinations that the uses of their newest chemicals in food are safe without notifying the FDA. The agency’s attempts to limit these undisclosed GRAS determinations by asking industry to voluntarily inform the FDA about their chemicals are insufficient to ensure the safety of our food in today’s global marketplace with a complex food supply. Furthermore, no other developed country in the world has a system like GRAS to provide oversight of food ingredients. In Table 1 and 2 of the report, NRDC identified the 56 companies and the number of chemicals that each company appeared to market as GRAS without FDA clearance. -

Finnish Food Offering: Berry Based Products Berries - Useful Links
Finnish Food Offering: Berry based products Berries - Useful Links Brochures of Finnish berries in different languages: http://arktisetaromit.fi/fi/arktiset+aromit/hankeaineistot/ Finnish Companies exporting bilberry based products: www.arcticbilberry.fi Finnish Companies exporting lingonberry based products: www.arcticlingonberry.fi Finnish Companies’ web-pages in English: http://arktisetaromit.fi/en/arktiset+aromit/links/ 7/21/2017 © Finpro 2 Berry based Products - export companies 3 7/21/2017 © Finpro Oat SINCE EMPLOYEES SIZE HEADQUARTER www.kiantama.fi/en/ 1973 < 50 Small Suomussalmi http://www.biokia.fi/en/ Kiantama is a Finnish company founded in 1973, specializing in the processing of wild berries. We produce and develop high-quality berry products and raw material for food, health supplement and cosmetics industries. Kiantama sells part of its products under Biokia brand name. Biokia berries are handpicked to ensure highest quality and sustainability of the forests. In addition to local berry pickers, hundreds of foreign berry pickers are also invited to come and pick berries during the season every year. We take responsibility for paying a reasonable salary for our berry pickers. All our operations comply with the ISO 26000 Guidance on Social Responsibility The juicy berries arrive are gently processed into delicious products. They are dried, frozen, powdered, cold pressed and coated gently, in accordance with meticulous and carefully supervised process. No additives, artificial sweeteners or preservatives are added to the berries. -

Icelandic Herbs and Their Medicinal Uses
Icelandic Herbs and Their Medicinal Uses Anna rósa róbertsdóttir Contents Foreword . ix Male Fern . 136. Acknowledgments . x. Mare’s-tail . 138 Introduction . .1 . Marsh Marigold . 140 Meadow Buttercup . .144 . Harvesting . .3 . Meadowsweet . 146. Uses of Herbs . 6 Mountain Avens . .150 . Alpine Bistort . 12. Nootka Lupine . 152. Angelica . .14 Northern Dock . 154. Arctic Poppy . 18. Pineappleweed . 158 Bearberry . 20. Polypody . 160 Bilberry . .24 Purging Flax . 162. Biting Stonecrop . 28. Purple Marshlocks. .164 . Bladderwrack . .30 Red Clover . 166. Bogbean . .32 . Ribwort Plantain . .170 . Butterwort . 36. Rose Bay Willow Herb . 174. Caraway . .38 . Roseroot . 176 Chickweed . 42. Rowan . .180 . Cold-weather Eyebright . .44 Scurvy Grass . 184. Coltsfoot . .48 . Sea Mayweed . 186. Common Sea-thrift . .50 Self-heal . .188 . Couch Grass . 52. Sheep’s Sorrel . 192 Cow Parsley . 54. Shepherd’s Purse . .194 . Creeping Thyme . 56. Silverweed . 198 Crowberry . .60 Sorrel . 202 Cuckooflower . .64 Speedwell . 204. Daisy . .66 Spotted Orchid . 206. Dandelion . .68 Stinging Nettle . 208. Devil’s Bit Scabious . .72 . Stone Bramble . 212. Downy Birch. 74. Sundew . 214 Dulse . .78 . Sweet Cicely . 216 Field Gentian . 82. Sweet Grass . 218 Fir Clubmoss . .84 Sweet Vernal Grass . 220 Grass of Parnassus . .86 Valerian . 222 Greater Burnet . 88. Water Avens . 226. Greater Plantain . .92 Water Forget-me-not . 228 Groundsel . 96. Water Speedwell . 230 Hawkweed . 98. White Dead-nettle . .232 . Heartsease . 100. Wild Strawberry . .234 . Heather . 102 Willow . .236 . Hemp-nettle . 104 Wood Cranesbill . 240 Horsetail . 106. Yarrow . .242 . Iceland Moss . 110. Yellow Rattle . 246. Irish Moss . 114. Juniper . 116 Glossary . 248 Kidney Vetch. 120. Bibliography . 252 Knotgrass . 122 Research Bibliography . 254 Lady’s Bedstraw . 126 Index . -

Vaccaria Pyramidata (L.) Medik. Synonym Saponaria Vaccaria L
V Vaccaria pyramidata (L.) Medik. anthocyanine enriched extracts of the fruit, in symptomatic treatment Synonym Saponaria vaccaria L. of problems related to varicose Family Caryophyllaceae. veins, such as heavy legs. (ESCOP.) Cranberry (Vaccinium sp.) is used Habitat Throughout India, as a weed. in urinary incontinence and for UTI prevention. (Sharon M. Herr.) English Soapwort, Cow Herb. Folk Musna, Saabuni. The main constituents of the Bil- berry fruit are anthocyanosides .%. Action Roots—used for cough, Other constituents include tannins, hy- asthma and other respiratory droxycinnamic and hydroxybenzoic disorders; for jaundice, liver and acids, flavonol glycosides, flavan--ols, spleen diseases (increases bile flow). iridoids, terpenes, pectins and organic Mucilaginous sap—used in scabies. plant acids. (ESCOP.) Saponins of the root showed haemo- In India, V. symplocifolium Alston, lytic activity. Lanostenol, stigmas- syn. V. leschenaultii Wight, known as terol, beta-sitosterol and diosgenin Kilapalam in Tamil Nadu, is abundant- have been isolated from the plant. ly found in the mountains of South In- Xanthones, vaccaxanthone and sapx- dia up to an altitude of , m V. neil- anthone, and a oligosaccharide, vac- gherrense Wight, known as Kalavu in carose, have also been isolated. Tamil Nadu and Olenangu in Karnata- ka, is commonly found in the hills of Kerala, Karnataka and Tamil Nadu at Vaccinium myrtillus Linn. altitudes of –, m. Family Vacciniaceae. Habitat UK, Europe and North Valeriana dubia Bunge. America. (About species of Vaccinium are found in India.) Synonym V. officinalis auct. non English Bilberry, Blueberry. Linn. Action Astringent, diuretic, Family Valerianacea. refrigerant. Habitat Western Himalayas, Key application Fruit—in non- Kashmir at Sonamarg at ,– specific,acute diarrhoea; topically in , m. -

Appendix 1 Vernacular Names
Appendix 1 Vernacular Names The vernacular names listed below have been collected from the literature. Few have phonetic spellings. Spelling is not helped by the difficulties of transcribing unwritten languages into European syllables and Roman script. Some languages have several names for the same species. Further complications arise from the various dialects and corruptions within a language, and use of names borrowed from other languages. Where the people are bilingual the person recording the name may fail to check which language it comes from. For example, in northern Sahel where Arabic is the lingua franca, the recorded names, supposedly Arabic, include a number from local languages. Sometimes the same name may be used for several species. For example, kiri is the Susu name for both Adansonia digitata and Drypetes afzelii. There is nothing unusual about such complications. For example, Grigson (1955) cites 52 English synonyms for the common dandelion (Taraxacum officinale) in the British Isles, and also mentions several examples of the same vernacular name applying to different species. Even Theophrastus in c. 300 BC complained that there were three plants called strykhnos, which were edible, soporific or hallucinogenic (Hort 1916). Languages and history are linked and it is hoped that understanding how lan- guages spread will lead to the discovery of the historical origins of some of the vernacular names for the baobab. The classification followed here is that of Gordon (2005) updated and edited by Blench (2005, personal communication). Alternative family names are shown in square brackets, dialects in parenthesis. Superscript Arabic numbers refer to references to the vernacular names; Roman numbers refer to further information in Section 4. -

Free Radical Scavenging Capacity and Cytotoxic and Antiproliferative Effects of Vaccinium Meridionale Sw
Revista Cubana de Plantas Medicinales 2014;19(2):172-184 ARTÍCULO ORIGINAL Free radical scavenging capacity and cytotoxic and antiproliferative effects of Vaccinium meridionale Sw. agains colon cancer cell lines Capacidad atrapadora de radicales libres, efectos citotóxicos y antiproliferativos de Vaccinium meridionale Sw. en líneas celulares de cáncer de colon Dra. Maria E. Maldonado-Celis,I MSc. Sandra Sulay Arango-Varela,II Dr. Benjamín Alberto RojanoIII I Grupo de Investigación en Alimentación y Nutrición Humana, Universidad de Antioquia. Medellín, Colombia. II Grupo Sinergia Ingeniería Biomédica, Facultad de Ingeniería, Instituto Tecnológico Metropolitano, Medellín, Colombia. III Grupo de Química de los Productos Naturales y los Alimentos. Universidad Nacional. Medellín, Colombia. ABSTRACT Introduction: Vaccinium meridionale Swartz, of the family Ericaceae, is commonly known as mortiño or agraz. The plant is considered a functional food, with a content of anthocyanins and antioxidants similar to or greater than that reported for other Vaccinium species. However, little is known about its nutraceutical and medicinal properties. Objectives: determine the antioxidant activity and cytotoxic and antiproliferative effect of mortiño fruit aqueous extract against colon adenocarcinoma cells (SW480) and their derived metastatic cells (SW620). Methods: total phenols and anthocyanins were determined by the Folin-Ciocalteu method. Caffeoyl derivatives were determined by HPLC-DAD. Antioxidant activity was analyzed as the ability to scavenge reactive oxygen species (ROS), reactive nitrogen species (RNI), peroxyl radicals and hydroxyl radicals. Cytotoxic and antiproliferative activities were studied by MTT and sulforhodamine B. Results: the following substances were found in 100 g of lyophilized extract: total phenols (2 546 mg GAE), anthocyanins (150.7 mg C3G), chlorogenic acid (126 mg), ferulic acid (108 mg) and coumaric acid (63 mg).