19-ID-03 Committee:
Infectious Disease
Title: Case Definition for Non-pestis Yersiniosis ☒Check this box if this position statement is an update to an existing standardized surveillance case definition: 18-ID-02
Synopsis: This position statement updates the case definition for non-pestis yersiniosis through the clarification of laboratory criteria.
I. Statement of the Problem
Non-pestis yersiniosis is an infection caused most commonly by the bacteria Yersinia enterocolitica or Yersinia pseudotuberculosis. These bacteria are normal intestinal and oropharyngeal colonizers of swine, and most commonly cause infections in children under 10 years of age, or adults over 70 years of age, through contaminated food. After Salmonella, Shigella, Campylobacter, and Shiga-toxin producing E. coli, it is the 5th most commonly reported gastrointestinal bacterial illness reported through CDC Foodborne Diseases Active Surveillance Network (FoodNet), which monitors 10 sites in the United States for nine enteric pathogens transmitted through food. The increasing use of culture-independent diagnostic tests (CIDTs) in all parts of clinical medicine, and particularly for gastrointestinal illnesses, has also increased recognition of certain pathogens. Data from 2016 from FoodNet show a 29% increase in culture-confirmed and a 91% increase in CIDT-diagnosed Yersinia infections when compared to the 2013-2015 time frame.
Yersinia enterocolitica and/or Yersinia pseudotuberculosis infections are reportable in 38 states, but no
standard national definition exists for confirmed and probable cases. This position statement proposes a standardized case definition for non-pestis yersiniosis.
II. Background and Justification
Yersinia enterocolitica and Yersinia pseudotuberculosis are Gram negative rod-shaped or coccoid
organisms that can be isolated from many animals and are most often transmitted to humans from undercooked or contaminated pork. Pathogenic serotypes have also been found in numerous other foods, milk products, and water. Together, infection with either of these organisms is known as non-pestis yersiniosis. Y. enterocolitica is the more common of the two infections and most often causes gastrointestinal infections that can involve fever, diarrhea that may be bloody, and severe abdominal pain due to inflamed lymph nodes known as mesenteric adenitis. This abdominal pain can be so severe that it mimics appendicitis. Extra-intestinal manifestations include soft tissue abscesses, and post-infectious immune-mediated syndromes such as reactive arthritis and soft tissue swellings called erythema nodosum are also associated with Y. enterocolitica. This organism has also been described rarely as a cause of severe sepsis after transfusions with contaminated red blood cell transfusions. Y. pseudotuberculosis is much less common, but has similar animal reservoirs, transmission patterns, and clinical presentations. Both most commonly infect children less than 10 years of age, or adults older than 70 years of age, have an incubation period from 1-14 days, and illness lasts 7-14 days. The illness is often self-limited, but may require hospitalization. Diagnosis is via culture, serology, or nucleic acid amplification test (NAAT), and may be from specimens including stool, blood, urine, infected tissue, or pus.1 Four multiplex gastrointestinal panel NAAT CIDTs are currently commercially available, and three report 90-100% sensitivity for detection of Yersinia in clinical specimens.2 Three closely related species that may cause
disease, Y. intermedia, Y. fredericksenii, and Y. kristensenii, have high levels of cross-reactivity with the Y.
enterocolitca in these NAAT CIDTs,3 so laboratories may only report CIDTs to Yersinia genus level. Additionally, per FoodNet from sites reporting during 2010-2018, Y. enterocolitica was the most commonly
reported non-pestis Yersinia species (n=1324), followed by Y. fredericksenii (n=69), Y. intermedia (n=50),
- 19-ID-03
- 1
Y. kristensenii (n=18), Y. pseudotuberculosis (n=16), and Y. ruckeri (n=15). Most strains are susceptible to
tetracyclines and gentamicin. There are no vaccines for non-pestis yersiniosis at this time.1 Historically African-American children under 5 years of age were at highest risk of developing non-pestis yersiniosis. This was seen particularly in southern communities where chitterlings, a holiday dish made of pig intestines, was a commonly consumed food. Since a public education campaign on food safety was performed in Georgia, children under 5 remain the highest risk group for infection, but there is no longer a predominance of cases in African-American children.4 Overall rates had been decreasing with time until 2016, when a significant increase in both culture-confirmed and NAAT CIDT-diagnosed cases was noted.5 Since Yersinia is the 5th most commonly reported enteric bacterial pathogen in FoodNet-monitored sites and does not yet have a standard case definition, it would be beneficial to those 38 states who do have mandatory reporting, and any future jurisdictions who wish to expand to include non-pestis yersiniosis in their reporting for CSTE to create a national case definition for these illnesses.
III. Statement of the desired action(s) to be taken
CSTE recommends the following actions:
1. Implement a standardized surveillance case definition for non-pestis yersiniosis.
A. Utilize standard sources (e.g. reporting*) for case ascertainment for non-pestis yersiniosis.
Surveillance for non-pestis yersiniosis should use the recommended sources of data to the extent of coverage presented in Section V.
B. Utilize standardized criteria for case ascertainment for non-pestis yersiniosis presented in
Section VI and Table VI in Technical Supplement.
C. Utilize standardized criteria for case classification for non-pestis yersiniosis presented in
Sections VII and Table VII in Technical Supplement.
Note: this action does NOT add non-pestis yersiniosis to the Nationally Notifiable Condition List. If
requested by CDC, jurisdictions (e.g., States and Territories) conducting surveillance according to these methods may voluntarily submit case information to CDC.
IV. Goals of Surveillance
.
The goals of surveillance are to provide timely and standardized information in order to identify and control any transmission, as well as facilitate comparability in case counts across jurisdictions. This is not a recommendation to require national reporting.
V. Methods for Surveillance: Surveillance for non-pestis yersiniosis should use the recommended sources of data and the extent of coverage listed in Table III.
Data sources for case ascertainment include clinician and laboratory reporting. A positive culture for any Yersinia non-pestis species is a requirement to be a confirmed case; a positive PCR CIDT for any Yersinia non-pestis species or clinically compatible case with epidemiologic link to a confirmed or probable case is necessary to be a probable case.
Table V. Recommended sources of data and extent of coverage for ascertainment of cases of non-pestis yersiniosis.
Coverage
Source of data for case ascertainment
Clinician reporting Laboratory reporting
- Population-wide
- Sentinel sites
XX
- 19-ID-03
- 2
Reporting by other entities (e.g., hospitals, veterinarians, pharmacies, poison centers), specify: Death certificates Hospital discharge or outpatient records Extracts from electronic medical records Telephone survey xxxx
School-based survey Other, specify:
2019 Template
*Reporting: process of a healthcare provider or other entity submitting a report (case information) of a condition under public health surveillance TO local or state public health. Note: notification is addressed in a Nationally Notifiable Conditions Recommendation Statement and is the process of a local or state public health authority submitting a report (case information) of a condition on the Nationally Notifiable Conditions List TO CDC.
VI. Criteria for case ascertainment A. Narrative: A description of suggested criteria for case ascertainment of non-pestis Yersiniosis
Report any person or laboratory finding to public health authorities that meets any of the following:
A1. Clinical Criteria for Reporting:
•
Any person with fever, diarrhea, or abdominal pain who had recent contact with a laboratory confirmed case of non-pestis yersiniosis.
•
Any person with fever, diarrhea, or abdominal pain who had recent contact with a member of a risk group during an outbreak of non-pestis yersiniosis
A2. Laboratory Criteria for Reporting:
••
Isolation of any Yersinia non-pestis species by culture from a clinical specimen. Detection of any Yersinia non-pestis species using a CIDT.
A3. Epidemiologic Linkage Criteria for Reporting
•
Any person with fever, diarrhea, or abdominal pain who had recent contact with a presumptive or laboratory confirmed case of non-pestis yersiniosis.
•
Any person with fever, diarrhea, or abdominal pain who had recent contact with a member of a risk group during an outbreak of non-pestis yersiniosis
B. Disease-specific data elements to be included in the initial report
In the initial report, please include
•
Test result specimen source, and type of test (if CIDT, PCR or antibody test) OR
•
Brief clinical description including severity of illness, if case required hospitalization, and type of epidemiologic linkage.
VII. Case Definition for Case Classification A. Narrative: Description of criteria to determine how a case should be classified.
A1. Clinical Criteria
An illness with either diarrhea that may or may not be bloody or abdominal pain that may be severe enough to mimic appendicitis.
- 19-ID-03
- 3
Note: Extra-intestinal manifestations may also be present, such as abscess, which could be a source for testing, and reactive arthritis and erythema nodosum, which are often immunologic phenomena not directly caused by the infection. These manifestations are not required as part of the clinical criteria.
A2. Laboratory Criteria
Confirmatory laboratory evidence: Isolation of Yersinia enterocolitica, Y. pseudotuberculosis, Y. intermedia, Y. fredericksenii, Y. kristensenii, or Y. ruckeri by culture from a clinical specimen
Presumptive laboratory evidence: Detection of any Yersinia non-pestis species using a PCR CIDT Supportive laboratory evidence: N/A
A3. Epidemiologic Linkage
A person who has had contact with a case that meets the presumptive or confirmatory laboratory criteria.
A4. Case Classifications
Confirmed:
A case that meets the confirmed laboratory criteria.
Probable:
A case that meets the presumptive laboratory criteria OR A clinically compatible case that is epidemiologically linked to a case meeting confirmatory or presumptive laboratory criteria
B. Criteria to distinguish a new case of this disease or condition from reports or notifications which should not be enumerated as a new case for surveillance
A repeat culture or PCR CIDT result within 365 days of initial report should not be enumerated as a new case for surveillance. When two or more different Yersinia non-pestis species are identified in one or more specimens from the same individual, each should be reported as a separate case.
VIII. Period of Surveillance
Surveillance is expected to be on-going.
IX. Data sharing/release and print criteria
CSTE recommends the following case statuses be included in the CDC Print Criteria:
☒Confirmed ☒Probable ☐Suspect ☐Unknown
- 19-ID-03
- 4
X. Revision History
Position Statement ID 18-ID-02
Section of Document Section VII. A2. Confirmatory laboratory evidence.
Revision Description Added specific non-pestis
Yersinia species.
- 18-ID-02
- Technical Supplement Table VII. Edited for consistency with
- Laboratory evidence.
- Section VII. A2. Confirmatory
laboratory evidence.
XI. References
1.
Woods CR. Other Yersinia Species. In: Feigin and Cherry’s Textbook of Pediatric Infectious
Diseases. Philadelphia, PA: Elsevier Saunders; 2014:1514-1531.
- 2.
- Huang RSP, Johnson CL, Pritchard L, Hepler R, Ton TT, Dunn JJ. Performance of the
Verigene® enteric pathogens test, Biofire FilmArrayTM gastrointestinal panel and Luminex xTAG® gastrointestinal pathogen panel for detection of common enteric pathogens. Diagn Microbiol Infect Dis. 2016;86(4):336-339. doi:10.1016/j.diagmicrobio.2016.09.013. Noble MA, Barteluk RL, Freeman HJ, et al. Clinical significance of virulence-related assay of
Yersinia species. J Clin Micr. 1987;25(5):802-807.
Ong KL, Gould LH, Chen DL, et al. Changing Epidemiology of Yersinia enterocolitica Infections: Markedly decreased rates in young black children, Foodborne Diseases Active Surveillance Network ( FoodNet ), 1996 – 2009. 2015;54(0 5):S385-S390. Marder EP, Cieslak PR, Cronquiest AB, et al. Incidence and trends of infections with pathogens transmitted commonly through food and the effect of increasing use of cultureindependent diagnostic tests on surveillance —Foodborne Diseases Active Surveillance Network, 10 U.S. Sites, 2013-2016. MMWR. 2017;66(15):404-407.
3. 4.
5.
doi:http://dx.doi.org/10.15585/mmwr.mm6615a1.
XII. Coordination Subject Matter Expert (SME) Consultants:
- (1)
- Kirk Smith
Enteric Diseases Subcommittee Chair CSTE
(4) (5)
Logan Ray Epidemiologist, FoodNet Centers for Disease Control and Prevention
- (2)
- Ellyn Marder
- Sarah Labuda
Surveillance Epidemiologist, FoodNet Centers for Disease Control and Prevention 404-718-4722
Epidemic Intelligence Service Officer CDC, Assigned to Arkansas Department of Health
- [email protected]
- 4815 West Markham Street, Slot 32
Little Rock, AR 72205-3867
- 501-614-5278
- (3)
- Aimee Geissler
Epidemiologist, FoodNet Centers for Disease Control and Prevention [email protected]
[email protected]
- 19-ID-03
- 5
Agencies for Response
(1) Centers for Disease Control and Prevention
Robert R. Redfield, MD Director 1600 Clifton Rd Atlanta, GA 30333 404-639-7000 [email protected]
Agencies for Information
N/A
XIII. Author Information Submitting and Presenting Author
- (1)
- Dirk Haselow
State Epidemiologist Arkansas Department of Health 4815 West Markham Street, Slot 32 Little Rock, AR 72205-3867 501-614-5278 [email protected]
Co-Author: (Complete contact information must be provided for acceptance to review.)
- (1)
- Active Member
Krisandra Allen
Associate Member
Foodborne and Enteric Disease Epidemiologist Washington State Department of Health 1610 NE 150th Street Shoreline, WA 98155 206-418-5440 [email protected]
- 19-ID-03
- 6
Technical Supplement
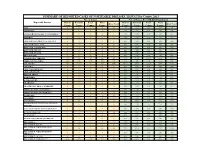
Table VI. Table of criteria to determine whether a case should be reported to public health authorities.
Criterion
Clinical Criteria for Reporting
Fever Diarrhea Abdominal pain
- Non-pestis yersiniosis
- Non-pestis yersiniosis
OOO
Laboratory Criteria for Reporting Isolation of any Yersinia non-pestis species by
culture from a clinical specimen
Detection of any Yersinia non-pestis species
using a CIDT
SS
Epidemiological Linkage Criteria for Reporting
Person had recent contact with a laboratory confirmed or probable case of non-pestis yersinosis Member of a risk group during an outbreak investigation of non-pestis yersiniosis
OO
2019 Template
Notes: S = This criterion alone is SUFFICIENT to report a case. O = At least one of these “O” (ONE OR MORE) criteria in each category (categories=clinical evidence, laboratory evidence, and epidemiological evidence) in the same column—in conjunction with all “N” criteria in the same column—is required to report a case.
Table VII. Classification Table: Criteria for defining a case of non-pestis Yersiniosis.
- Probable
- Probable
- Confirmed
Clinical Evidence
Diarrhea Abdominal pain
OO
Laboratory Evidence Isolation of Yersinia enterocolitica, Y. pseudotuberculosis, Y. intermedia, Y. fredericksenii, Y. kristensenii, or Y. ruckeri by culture from a clinical
specimen
S
Detection of any Yersinia non-pestis species using a PCR CIDT
Epidemiological Evidence
Epidemiologically linked to a confirmed or probable case of non-pestis yersiniosis
Criteria to distinguish a new case:
Not counted as a new case if occurred within 365 days of initial case
SN
N
- N
- N
2019 Template
Notes: S = This criterion alone is SUFFICIENT to classify a case. N = All “N” criteria in the same column are NECESSARY to classify a case. A number following an “N” indicates that this criterion is only required for a specific disease/condition subtype (see below). If the absence of a criterion (i.e., criterion NOT present) is required for the case to meet the classification criteria, list the absence of criterion as a necessary component.
O = At least one of these “O” (ONE OR MORE) criteria in each category (categories=clinical evidence, laboratory evidence, and epidemiologic evidence) in the same column—in conjunction with all “N” criteria in the same column—is required to classify a case. A number following an “O” indicates that this criterion is only required for a specific disease/condition subtype.
Technical Supplement: 19-ID-03