Evaluating the Child with Unsteady Gait
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Syndrome-Based Clinical Approach for Clerkship Students General Comments 1. This Is Not an All-Inclusive “Cookbook” for Ev
A Syndrome-Based Clinical Approach for Clerkship Students General Comments 1. This is not an all-inclusive “cookbook” for every Neurology patient, but a set of guidelines to help you rationally approach patients with certain syndromes (sets of signs and symptoms which suggest a lesion in particular parts of the nervous system). 2. As you obtain a history and perform a neurological physical exam, try initially to localize all the patient’s signs and symptoms to one, single lesion in the nervous system. It may be surprising that a variety of signs and symptoms, at first glance apparently unrelated, on second thought can localize accurately to a single lesion. If this approach fails, then consider multiple, separate lesions for the patient’s signs and symptoms. 3. The tempo or rate at which signs and symptoms develop or occur often suggests the underlying pathological process. a. sudden onset---favors stroke (ischemia or hemorrhage), seizure, migraine (or other headache syndromes), and trauma b. subacute onset---favors inflammatory, infectious or immune-mediated disorders c. chronic onset---favors degenerative disorders, tumors Toximetabolic disorders, potentially treatable and reversible, may mimic lesions in the nervous system, and can evolve at variable tempos. Hereditary conditions may be congenital (present at birth) and nonprogressive or static, or develop later in life, with variable rates of progression. Family members affected by the same genetic disorder may be remarkably similar with regards to onset and clinical severity, while some genetic disorders vary widely regarding when and how severely family members are affected. 4. In the central nervous system, “positive symptoms or phenomena,” such as flashes of light, or a tingling sensation, suggest “excitation” or increased activity in the nervous system: migraine or seizure. -

Inherited Neuropathies
407 Inherited Neuropathies Vera Fridman, MD1 M. M. Reilly, MD, FRCP, FRCPI2 1 Department of Neurology, Neuromuscular Diagnostic Center, Address for correspondence Vera Fridman, MD, Neuromuscular Massachusetts General Hospital, Boston, Massachusetts Diagnostic Center, Massachusetts General Hospital, Boston, 2 MRC Centre for Neuromuscular Diseases, UCL Institute of Neurology Massachusetts, 165 Cambridge St. Boston, MA 02114 and The National Hospital for Neurology and Neurosurgery, Queen (e-mail: [email protected]). Square, London, United Kingdom Semin Neurol 2015;35:407–423. Abstract Hereditary neuropathies (HNs) are among the most common inherited neurologic Keywords disorders and are diverse both clinically and genetically. Recent genetic advances have ► hereditary contributed to a rapid expansion of identifiable causes of HN and have broadened the neuropathy phenotypic spectrum associated with many of the causative mutations. The underlying ► Charcot-Marie-Tooth molecular pathways of disease have also been better delineated, leading to the promise disease for potential treatments. This chapter reviews the clinical and biological aspects of the ► hereditary sensory common causes of HN and addresses the challenges of approaching the diagnostic and motor workup of these conditions in a rapidly evolving genetic landscape. neuropathy ► hereditary sensory and autonomic neuropathy Hereditary neuropathies (HN) are among the most common Select forms of HN also involve cranial nerves and respiratory inherited neurologic diseases, with a prevalence of 1 in 2,500 function. Nevertheless, in the majority of patients with HN individuals.1,2 They encompass a clinically heterogeneous set there is no shortening of life expectancy. of disorders and vary greatly in severity, spanning a spectrum Historically, hereditary neuropathies have been classified from mildly symptomatic forms to those resulting in severe based on the primary site of nerve pathology (myelin vs. -

THE NEUROLOGY Exam & Clinical Pearls
THE NEUROLOGY Exam & Clinical Pearls Gaye McCafferty, RN, MS, NP-BC, MSCS, SCRN NPANYS-SPHP Education Day Troy, New York April 7, 2018 Objectives I. Describe the core elements of the neurology exam II. List clinical pearls of the neuro exam Neurology Exam . General Physical Exam . Mental Status . Cranial Nerves . Motor Exam . Reflex Examination . Sensory Exam . Coordination . Gait and Station 1 General Systemic Physical Exam Head Trauma Dysmorphism Neck Tone Thyromegaly Bruits MSOffice1 General Systemic Physical Exam .Cardiovascular . Heart rate, rhythm, murmur; peripheral pulses, JVD .Pulmonary . Breathing pattern, cyanosis, Mallampati airway .General Appearance Hygiene, grooming, weight (signs of self neglect) .Funduscopic Exam Mental Status Level of Consciousness . Awake . Drowsy . Somnolent . Comatose 2 Slide 5 MSOffice1 , 6/14/2009 Orientation & Attention . Orientation . Time . Place . Person Orientation & Attention . Attention . Digit Span-have the patient repeat a series of numbers, start with 3 or 4 in a series and increase until the patient makes several mistakes. Then explain that you want the numbers backwards. Normal-seven forward, five backward Hint; use parts of telephone numbers you know Memory Immediate recall and attention Tell the patient you want him to remember a name and address – Jim Green – 20 Woodlawn Road, Chicago Note how many errors are made in repeating it and how many times you have to repeat it before it is repeated correctly. Normal: Immediate registration 3 Memory . Short-term memory . About 5 minutes after asking the patient to remember the name and address, ask him to repeat it. Long –term memory . Test factual knowledge . Dates of WWII . Name a president who was shot dead Memory Mini-Mental State Exam – 30 items Mini-Cog – Rapid Screen for Cognitive Impairment – A Composite of 3 item recall and clock drawing – Takes about 5 minutes to administer Mini-Cog Mini-Cog Recall 0 Recall 1-2 Recall 3 Demented Non-demented Abnormal Clock Normal Clock Demented Non-demented 4 Memory . -
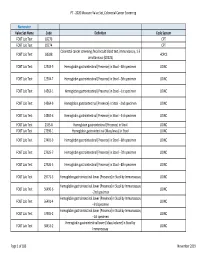
2020 Measure Value Set Colorectal Cancer Screening
PT ‐ 2020 Measure Value Set_Colorectal Cancer Screening Numerator Value Set Name Code Definition Code System FOBT Lab Test 82270 CPT FOBT Lab Test 82274 CPT Colorectal cancer screening; fecal occult blood test, immunoassay, 1‐3 FOBT Lab Test G0328 HCPCS simultaneous (G0328) FOBT Lab Test 12503‐9 Hemoglobin.gastrointestinal [Presence] in Stool ‐‐4th specimen LOINC FOBT Lab Test 12504‐7 Hemoglobin.gastrointestinal [Presence] in Stool ‐‐5th specimen LOINC FOBT Lab Test 14563‐1 Hemoglobin.gastrointestinal [Presence] in Stool ‐‐1st specimen LOINC FOBT Lab Test 14564‐9 Hemoglobin.gastrointestinal [Presence] in Stool ‐‐2nd specimen LOINC FOBT Lab Test 14565‐6 Hemoglobin.gastrointestinal [Presence] in Stool ‐‐3rd specimen LOINC FOBT Lab Test 2335‐8 Hemoglobin.gastrointestinal [Presence] in Stool LOINC FOBT Lab Test 27396‐1 Hemoglobin.gastrointestinal [Mass/mass] in Stool LOINC FOBT Lab Test 27401‐9 Hemoglobin.gastrointestinal [Presence] in Stool ‐‐6th specimen LOINC FOBT Lab Test 27925‐7 Hemoglobin.gastrointestinal [Presence] in Stool ‐‐7th specimen LOINC FOBT Lab Test 27926‐5 Hemoglobin.gastrointestinal [Presence] in Stool ‐‐8th specimen LOINC FOBT Lab Test 29771‐3 Hemoglobin.gastrointestinal.lower [Presence] in Stool by Immunoassay LOINC Hemoglobin.gastrointestinal.lower [Presence] in Stool by Immunoassay FOBT Lab Test 56490‐6 LOINC ‐‐2nd specimen Hemoglobin.gastrointestinal.lower [Presence] in Stool by Immunoassay FOBT Lab Test 56491‐4 LOINC ‐‐3rd specimen Hemoglobin.gastrointestinal.lower [Presence] in Stool by Immunoassay FOBT Lab Test 57905‐2 -

9781441967237.Pdf
The Neurologic Diagnosis wwwwwwwwww Jack N. Alpert The Neurologic Diagnosis A Practical Bedside Approach Jack N. Alpert, MD St. Luke’s Episcopal Hospital Department of Neurology University of Texas Medical School at Houston Houston, TX, USA [email protected] ISBN 978-1-4419-6723-7 e-ISBN 978-1-4419-6724-4 DOI 10.1007/978-1-4419-6724-4 Springer New York Dordrecht Heidelberg London Library of Congress Control Number: 2011941214 © Springer Science+Business Media, LLC 2012 All rights reserved. This work may not be translated or copied in whole or in part without the written permission of the publisher (Springer Science+Business Media, LLC, 233 Spring Street, New York, NY 10013, USA), except for brief excerpts in connection with reviews or scholarly analysis. Use in connection with any form of information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed is forbidden. The use in this publication of trade names, trademarks, service marks, and similar terms, even if they are not identifi ed as such, is not to be taken as an expression of opinion as to whether or not they are subject to proprietary rights. While the advice and information in this book are believed to be true and accurate at the date of going to press, neither the authors nor the editors nor the publisher can accept any legal responsibility for any errors or omissions that may be made. The publisher makes no warranty, express or implied, with respect to the material contained herein. Printed on acid-free paper Springer is part of Springer Science+Business Media (www.springer.com) In Memory of Morris B. -

Physical Therapy Practice
Physical Therapy Practice THE MAGAZINE OF THE ORTHOPAEDIC SECTION, APTA VOL. 18, NO. 2 2006 ORTHOPAEDIC CARDON REHABILITATION PRODUCTS, INC.™ Wurlitzer Industrial Park, 908 Niagara Falls Blvd. North Tonawanda, NY 14120 Telephone: 1-800-944-7868 • Fax: 716-297-0411 E-mail: [email protected] THE ACCEPTED STANDARD OF PERFORMANCE The Cardon Mobilization Table . Going beyond the third dimension . Now available with the patented option which eliminates the use of flexion and rotation levers. This allows the therapist to perform advanced manual therapy techniques with complete confidence and comfort with an ergonomically friendly design. The unique design provides more efficient and smooth setup while providing superior patient comfort. The option enhances patient care by allowing unsurpassed opportunity for more preciseness of treatment and monitoring of segments and joints. he design and concepts make this “T the best mobilization table manufactured today.” Professor Freddy Kaltenborn Autho, Int’l Lecturer in Manual Therapy he various sections have minimum flex “T allowing very accurate application of specific manual therapy techniques.” Olaf Evjenth ES! I would like to preview the Author, Int’l Lecturer in Manual Therapy Y Cardon Mobilization Table. Please rush your 15 minute VHS video (for standard model): SEE FOR Name: Title: YOURSELF Clinic/Institution: THESE Address: OUTSTANDING City: State: Zip Code: Telephone: Signature: FEATURES: CARDON REHABILITATION PRODUCTS, INC.™ • Accurate localization of the vertebral segment Wurlitzer Industrial Park, 908 Niagara Falls Blvd. • Precision and versatility of technique North Tonawanda, NY 14120 • Absolute control of the mobilization forces Telephone: 1-800-944-7868 • Fax: 716-297-0411 • Excellent stability for manipulation. E-mail: [email protected] Orthopaedic Practice Vol. -

Neurological History and Physical Examination
emedicine.medscape.com eMedicine Specialties > Clinical Procedures > none Neurological History and Physical Examination Kalarickal J Oommen, MD, FAAN, Professor and Crofoot Chair of Epilepsy, Department of Neurology, Chief, Section of Epilepsy, Texas Tech University Health Sciences Center; Medical Director, Texas Tech University Health Sciences Center (TTUHSC) Covenant Comprehensive Epilepsy Center Updated: Nov 25, 2009 Neurological History "From the brain and the brain only arise our pleasures, joys, laughter and jests, as well as our sorrows, pains, griefs, and tears.... These things we suffer all come from the brain, when it is not healthy, but becomes abnormally hot, cold, moist or dry." —Hippocrates The Sacred Disease, Section XVII Taking the patient's history is traditionally the first step in virtually every clinical encounter. A thorough neurologic history allows the clinician to define the patient's problem and, along with the result of physical examination, assists in formulating an etiologic and/or pathologic diagnosis in most cases.[1 ] Solid knowledge of the basic principles of the various disease processes is essential for obtaining a good history. As Goethe stated, "The eyes see what the mind knows." To this end, the reader is referred to the literature about the natural history of diseases. The purpose of this article is to highlight the process of the examination rather than to provide details about the clinical and pathologic features of specific diseases. The history of the presenting illness or chief complaint should -
Movement Disorders and Gait Disturbances
Movement disorders and gait disturbances Kovács Norbert PTE ÁOK Neurológiai Klinika Pécs 1 MD pathophysiology z Genetic mutation or environmental injury of basal ganglia functioning z Pallidum, thalamus, subthalamic nucleus, caudate nucleus, pedunculopintine nucleus 2 Vitek JL. Mov Disord 2002;17(Supp 3):S49-62 Phenomenology in MD Hyperkinetic Isokinetic Hypokinetic • Tremor (regular) • Ataxia • Rigidity • Chorea • Bradykinesia • Ballism • Hypokinesia • Dystonia • Athetosis • Myoclonus (jerky) • Tic (jerky) 3 Hyperkinetic movements 4 Tremor classification More or less regular, sinusoid movements Any body parts can be affected (e.g. limbs, neck, trunc, vocal cords) Classification: • Intensity (invisible, barely visible, moderate, severe) • Frequency (slow or fast) • Position – Rest tremor (e.g. Parkinsonism) – Postural tremor (e.g. hyperthyroidism) – Kinetic tremor (e.g. essential tremor) – Intention tremor (e.g. cerebellar tremor) 5 Rest tremor Cognition (e.g. counting), gait or talking about the disease 6 usually increases the amplitude Intention tremor The tremor amplitude is the highest at the target. Usually 7 caused by cerebellar problems. Postural –kinetic tremor 8 Postural –kinetic tremor 9 Essential tremor is the most frequent cause of kinetic tremor. Postural –kinetic tremor 10 Always examine water drinking, writing and tableware use -- QoL Deep brain stimulation for tremor 11 Chorea The word chorea denotes rapid irregular muscle jerks that occur involuntarily and unpredictably in different parts of the body. Most important cause is12 Parkinson’s disease Ballism Large involuntary movements involving the whole extremity. Usually accompanies the chorea. Vascular lesion e.g. in the area of subthalamic13 nucleus can produce Athetosis abnormal movements that are slow, sinuous, and writhing in character. 14 Dystonia • Not a disease, it is a syndrome • Involuntary phasic, movement and/or • Sustained, involuntary, abnormal muscle contractions. -
GAIT DISORDERS, FALLS, IMMOBILITY Mov7 (1)
GAIT DISORDERS, FALLS, IMMOBILITY Mov7 (1) Gait Disorders, Falls, Immobility Last updated: April 17, 2019 GAIT DISORDERS ..................................................................................................................................... 1 CLINICAL FEATURES .............................................................................................................................. 1 CLINICO-ANATOMICAL SYNDROMES .............................................................................................. 1 CLINICO-PHYSIOLOGICAL SYNDROMES ......................................................................................... 1 Dyssynergy Syndromes .................................................................................................................... 1 Frontal gait ............................................................................................................................ 2 Sensory Gait Syndromes .................................................................................................................. 2 Sensory ataxia ........................................................................................................................ 2 Vestibular ataxia .................................................................................................................... 2 Visual ataxia .......................................................................................................................... 2 Multisensory disequilibrium ................................................................................................. -
Mobile Gait Analysis: from Prototype Towards Clinical Grade Wearable
FAU Studien aus der Informatik 6 Julius Hannink Mobile Gait Analysis: From Prototype towards Clinical Grade Wearable Julius Hannink Mobile Gait Analysis: From Prototype towards Clinical Grade Wearable FAU Studien aus der Informatik Band 6 Herausgeber der Reihe: Björn Eskofier, Richard Lenz, Andreas Maier, Michael Philippsen, Lutz Schröder, Wolfgang Schröder-Preikschat, Marc Stamminger, Rolf Wanka Julius Hannink Mobile Gait Analysis: From Prototype towards Clinical Grade Wearable Erlangen FAU University Press 2019 Bibliografische Information der Deutschen Nationalbibliothek: Die Deutsche Nationalbibliothek verzeichnet diese Publikation in der Deutschen Nationalbibliografie; detaillierte bibliografische Daten sind im Internet über http://dnb.d-nb.de abrufbar. Das Werk, einschließlich seiner Teile, ist urheberrechtlich geschützt. Die Rechte an allen Inhalten liegen bei ihren jeweiligen Autoren. Sie sind nutzbar unter der Creative Commons Lizenz BY-NC. Der vollständige Inhalt des Buchs ist als PDF über den OPUS Server der Friedrich-Alexander-Universität Erlangen-Nürnberg abrufbar: https://opus4.kobv.de/opus4-fau/home Bitte zitieren als Hannink, Julius. 2019. Mobile Gait Analysis: From Prototype towards Clinical Grade Wearable. FAU Studies FAU Studien aus der Informatik Band 6. Erlangen: FAU University Press. DOI: 10.25593/978-3-96147-173-7 Verlag und Auslieferung: FAU University Press, Universitätsstraße 4, 91054 Erlangen Druck: docupoint GmbH ISBN: 978-3-96147-172-0 (Druckausgabe) eISBN: 978-3-96147-173-7 (Online-Ausgabe) ISSN: 2509-9981 DOI: 10.25593/978-3-96147-173-7 Mobile Gait Analysis: From Prototype towards Clinical Grade Wearable Mobile Ganganalyse: Vom Prototyp in Richtung klinisch anwendbarer Systeme Der Technischen Fakultät der Friedrich-Alexander-Universität Erlangen-Nürnberg zur Erlangung des Doktorgrades Dr.-Ing. -

A Dictionary of Neurological Signs.Pdf
A DICTIONARY OF NEUROLOGICAL SIGNS THIRD EDITION A DICTIONARY OF NEUROLOGICAL SIGNS THIRD EDITION A.J. LARNER MA, MD, MRCP (UK), DHMSA Consultant Neurologist Walton Centre for Neurology and Neurosurgery, Liverpool Honorary Lecturer in Neuroscience, University of Liverpool Society of Apothecaries’ Honorary Lecturer in the History of Medicine, University of Liverpool Liverpool, U.K. 123 Andrew J. Larner MA MD MRCP (UK) DHMSA Walton Centre for Neurology & Neurosurgery Lower Lane L9 7LJ Liverpool, UK ISBN 978-1-4419-7094-7 e-ISBN 978-1-4419-7095-4 DOI 10.1007/978-1-4419-7095-4 Springer New York Dordrecht Heidelberg London Library of Congress Control Number: 2010937226 © Springer Science+Business Media, LLC 2001, 2006, 2011 All rights reserved. This work may not be translated or copied in whole or in part without the written permission of the publisher (Springer Science+Business Media, LLC, 233 Spring Street, New York, NY 10013, USA), except for brief excerpts in connection with reviews or scholarly analysis. Use in connection with any form of information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed is forbidden. The use in this publication of trade names, trademarks, service marks, and similar terms, even if they are not identified as such, is not to be taken as an expression of opinion as to whether or not they are subject to proprietary rights. While the advice and information in this book are believed to be true and accurate at the date of going to press, neither the authors nor the editors nor the publisher can accept any legal responsibility for any errors or omissions that may be made. -

Gait Disorders
What are the classical Gait Patterns for the Following Conditions? • Alzheimers Disease Gait Disorders • Hemiparetic Stroke • Parkinsons Disease T.Masud • Osteomalacia Nottingham University Hospitals NHS Trust • Lateral popliteal nerve palsy University of Nottingham University of Derby • Knee OA University of Southern Denmark • Vitamin B12 deficiency with dorsal column loss Statistical summaries of risk factors for falls From cohort studies- Perell 2001 RISK FACTOR Mean RR/OR Range Muscle weakness 4.4 (1.5-10.3) Falls history 3.0 (1.7-7.0) Gait deficit 2.9 (1.3-5.6) Balance deficit 2.9 (1.6-5.4) Use of assistive devices 2.6 (1.2-4.6) Visual deficit 2.5 (1.6-3.5) Arthritis 2.4 (1.9-2.7) Impaired ADLs 2.3 (1.5-3.1) Depression 2.2 (1.7-2.5) Cognitive impairment 1.8 (1.0-2.3) Age > 80 1.7 (1.1-2.5) Simple Model for Balance Balance Vision FALLS Vestibular Musculo- skeletal Proprioception Tactile sensation Activity & environmental hazards CNS Gait cycle [weight bearing] [progress] Running: stance 50% - swing 50%, then Asymmetry no double support period Stance phase Condition Disabled: increased bilateral stance phase Pain, weakness to increase double support period Impaired balance: vestibular, cerebellum dysfunction Clinical gait analysis Pattern Recognition of Gait Pattern recognition Hemiplegic Parkinsonian - Most quickly, recall from memory Apraxic Structured Approach Neuropathic - Hypothetico-deductive Ataxic - Basic gait knowledge / Anatomy Waddling Exhaustive strategy Spastic - Comprehensive and systematic evaluation Hyperkinetic Antalgic Gait Disorder in Older People High Level Gait Disorders by level of Sensorimotor Deficit Frontal Related • Apraxic •Cerebrovascular • Magnetic Low • Freezing High Middle •Dementia Level Level Level From- Alexander, Goldberg, Cleveland Clinic J Med 2005; 72: 592-600 High Level Gait Disorders High Level Gait Disorders Frontal Related Frontal Related •Cerebrovascular •Cerebrovascular •Dementia •Dementia •N.P.