Hand, Wrist and Elbow Problems: How to Spot Them in Clinic
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Fundamental Shoulder Exercises
FUNDAMENTAL SHOULDER EXERCISES RANGE OF MOTION EXERCISES 1. L-BAR FLEXION Lie on back and grip L-Bar between index finger and thumb, elbows straight. Raise both arms overhead as far as possible keeping thumbs up. Hold for _____ seconds and repeat _____ times. 2. L-BAR EXTERNAL ROTATION, SCAPULAR PLANE Lie on back with involved arm 450 from body and elbow bent at 900. Grip L-Bar in the hand of involved arm and keep elbow in flexed position. Using unin- volved arm, push involved arm into external rotation. Hold for _____ seconds, return to starting position. Repeat _____ times. 3. L-BAR INTERNAL ROTATION, SCAPULAR PLANE Lie on back with involved arm 450 from body and elbow bent at 900. Grip L-Bar in the hand of involved arm and keep elbow in flexed position. Using the uninvolved arm, push involved arm into internal rotation. Hold for _____ seconds, return to starting position. Repeat _____ times. Dr. Meisterling (800) 423-1088 1 of 2 STRENGTHENING EXERCISES 1. TUBING, EXTERNAL ROTATION Standing with involved elbow fixed at side, elbow bent to 900 and involved arm across the front of the body. Grip tubing handle while the other end of tubing is fixed. Pull out with arm, keeping elbow at side. Return tubing slowly and controlled. Perform _____ sets of _____ reps. 2. TUBING, INTERNAL ROTATION Standing with elbow at side fixed at 900 and shoulder rotated out. Grip tubing handle while other end of tubing is fixed. Pull arm across body keeping elbow at side. Return tubing slowly and controlled. -
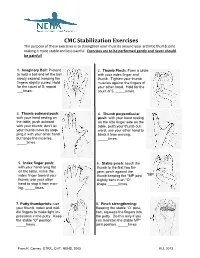
CMC Stabilization Exercises the Purpose of These Exercises Is to Strengthen Your Muscles Around Your Arthritic Thumb Joint Making It More Stable and Less Painful
CMC Stabilization Exercises The purpose of these exercises is to strengthen your muscles around your arthritic thumb joint making it more stable and less painful. Exercises are to be performed gently and never should be painful! 1. Imaginary Ball: Pretend 2. Thumb Pinch: Form a circle to hold a ball and let the ball with your index finger and slowly expand, keeping the thumb. Tighten your thumb fingers slightly curled. Hold muscles against the fingers of for the count of 5, repeat your other hand. Hold for the ___times. count of 5, _____times. 3. Thumb outward push: 4. Thumb perpendicular with your hand resting on push: with your hand resting the table, push outward on the little finger side on the with your thumb; don’t let table, push your thumb out- your thumb move by stop- ward; use your other hand to ping it with your other hand block it from moving. but tense the muscles. _____times. _____times. 5. Index finger push: 6. Stable pinch: touch the with your hand lying flat thumb to the first two fin- on the table, move the gers; pinch against the index finger toward your thumb keeping the *MP joint *MP thumb; use your other slightly bent in an “O” hand to stop it from mov- shape. _____times. ing. _____times. 7. Putty thumbprints: use 8. Pinch strengthening: your thumb, index and mid- Keeping the stable “O” posi- dle fingers to make light im- tion, squeeze the fingers into pressions in the putty. Keep the putty. Do this only if you the stable “O” position. -

Post-Operative Instructions for Flexor Tendon Repair Purpose of Surgery
Post-Operative Instructions for Flexor Tendon Repair Purpose of surgery The goal of the operation is to repair or reattach lacerated or detached flexor tendons. The flexor tendons (muscles) are responsible for flexing (bending) your fingers. What to expect after surgery? You will have a firm splint covering your forearm and the back of your hand and fingers holding your fingers flexed (bent). All your fingers will be included in the splint for any finger flexor tendon repair; and, only your thumb will be included in the splint for a thumb flexor tendon repair. You will be able to see the tips of your fingers/thumb to insure they are getting good circulation. The palm side of your fingers/thumb will be protected by a soft padding that they will be resting on while the plaster will keep your fingers bent from the nail side. You may have some numbness or tingling of fingers/thumb due to the local anesthetic injections used to help control post-operative pain (this should wear off within about 24 hours). After this first 24 hours, you may still experience some numbness and tingling in parts of the operative finger(s)/thumb if you also had a nerve repair. What should you do to help recover? While we do not anticipate significant swelling following this procedure, it would be helpful to keep your hand/wrist elevated as best you can for the first 24 hours after surgery. The thickness of the dressing will prevent the effective placement of a cold-pack. Please do not move your fingers, even if they were not operated on. -

Self Range of Motion Exercises for Arm and Hand
Self-Range of Motion Exercises for the Arm and Hand After a stroke, it is important to do the exercises in this handout for your affected arm and hand. You can do them on your own by using your unaffected arm and hand. These gentle movements are called “self-range of motion” exercises, and they help to maintain your movement, prevent stiffness, improve blood flow, and increase awareness of your affected arm and hand. Complete the exercises slowly and do not force movements. Stop if you feel pain. If you have any questions or concerns, please contact your Occupational Therapist: _______________________________ Do the exercises in this handout _____ times each day. Page - 1 Self-range of motion exercises for the arm and hand 1. Shoulder: Forward Arm Lift Interlock your fingers, or hold your wrist. With your elbows straight and thumbs facing the ceiling, lift your arms to shoulder height. Slowly lower your arms to starting position. Hold for ____ seconds. Repeat ____ times. Page - 2 Self-range of motion exercises for the arm and hand 2. Shoulder: “Rock the Baby” Stretch Hold your affected arm by supporting the elbow, forearm and wrist (as if cradling a baby). Slowly move your arms to the side, away from your body, lifting to shoulder height. Repeat this motion in the other direction. Slowly rock your arms side-to-side, and keep your body from turning. Repeat ____ times. Page - 3 Self-range of motion exercises for the arm and hand 3. Shoulder: Rotation Stretch Interlock your fingers, or hold your wrist. With your elbows bent at 90 degrees, keep your affected arm at your side. -

Laparoscopic Sacralcolpopexy and Enterocele Repair with Mesh
124 State of the Art Atlas and Textbook of Laparoscopic Suturing INTRODUCTION The anatomy, pathophysiology, and treatment of pelvic organ prolapse has significantly evolved over the last decade with increasing understanding of anatomy and development of minimally invasive surgical procedures. Although support for the pelvic viscera, the vagina, and neighboring structures involves a complex interplay between muscles, fascia, nerve supply, and appropriate anatomic orientation, the endopelvic fascia and pelvic floor muscles provide most of the support function in the female pelvis. Laparoscopic reconstructive pelvic surgery requires a thorough knowledge of pelvic floor anatomy and its supportive components before repair of defective anatomy is attempted. This chapter reviews the Fig. 13.1: Level 1 (apical suspension) and level 2 (lateral anatomy and laparoscopic repair of vaginal vault attachment). Level 1—paracolpium suspends the vagina apex prolapse and enterocele with Y-mesh sacralcolpopexy. from the lateral pelvic sidewall via the uterosacral-cardinal complex. Level 2—the anterior vaginal wall is attached laterally ANATOMY OF PELVIC SUPPORT to arcus tendinous fascia pelvis and the posterior vaginal wall is attached laterally to the fascia overlying the levator ani Endopelvic Fascia muscle To understand the pelvic support system of the female pelvic organs, it is useful to subdivide the third of the vagina to the bony sacrum. This complex pelvic support system into three axes: can be described as two separate entities: the cardinal 1. The upper vertical axis ligament and the uterosacral ligament. The cardinal 2. The midhorizontal axis ligament is a fascial sheath of collagen that envelops 3. The lower vertical axis. the internal iliac vessels and then continues along The endopelvic fascia—a network of connective the uterine artery, merging into the visceral capsule tissue and smooth muscle—constitutes the physical of the cervix, lower uterine segment and upper matrix which envelops the pelvic viscera and main- vagina. -

Upper Extremity Extensor Tendon Repair Protocol
Department of Rehabilitation Services Primary Upper Extremity and Hand Extensor Tendon Repair Protocol This protocol is not intended to be a substitute for one’s clinical decision making regarding the progression of a patient’s post-operative course based on their physical exam/findings, individual progress, and/or the presence of post-operative complications. If a clinician requires assistance in the progression of a patient, they should consult with the referring surgeon. The time frames of phases I-IV are examples and can be adjusted based on the given procedure. Progression to the next phase based on the clinical criteria and/or time frames, as appropriate. MALLET FINGER: ZONE I: Over the distal phalangeal joint (DIP)-Mallet deformity ZONE II: Over the middle phalanx/triangular ligament Goal: Protect extensor zone I and II with DIP held in extension with PIP joint free. Photo: Wikem.org/w/index.php?title Precautions: During orthotic/cast check out, keep DIP joints fully extended 100%. Frequency: one to two times/week for 6 to 10 weeks if needed for orthosis/cast checks. Primary Extensor Tendon Repair Protocol Copyright © 2020 The Brigham and Women's Hospital, Inc., Department of Rehabilitation Services. All rights reserved 1 PHASE ORTHOTIC THERAPEUTIC EXERCISE: CONSIDERATIONS: ongoing treatment is variable. Phase I immediate phase: Orthosis or circumferential cast Active PIP flexion of affected Patient to perform daily skin day 1 to 6 to 8 weeks. finger with adjacent finger(s) held check while keeping DIP Non-op: DIP 10°-0 in extension. extended. hyperextension for tendinous mallet 6-8 weeks. Consider taping DIP in extension. -

De Quervain's Tenosynovitis
PATIENT & CAREGIVER EDUCATION De Quervain's Tenosynovitis This information explains the causes, symptoms, and treatment of de Quervain’s tenosynovitis (da-cur-vains teno-sin-o-vitis). De Quervain’s tenosynovitis is a common and painful condition that affects the tendons (tissue that connects muscles to bones) of the wrist. A tendon sheath (protective covering) wraps around these tendons so that they can slide easily (see Figure 1). This allows you to turn your wrist, grip, and pinch with your hand. With de Quervain’s tenosynovitis, the tendon sheath becomes swollen. This causes pain and limited movement in your wrist and thumb. Figure 1. Wrist with De Quervain’s tenosynovitis Causes of De Quervain’s Tenosynovitis Some causes of de Quervain’s tenosynovitis include: Overusing your wrist with repetitive movements, such as: Typing Knitting De Quervain's Tenosynovitis 1/4 Using a hammer Holding an infant for a long time Carrying heavy grocery bags Strain or injury to the wrist area. Conditions that cause swelling throughout the body, such as rheumatoid arthritis. Symptoms of De Quervain’s Tenosynovitis De Quervain’s tenosynovitis can cause different symptoms, such as: Pain at the side of your wrist under the base of your thumb. Moving your thumb can increase this pain. Wrist pain that has spread into your forearm and thumb. Mild swelling, redness, or warmth at your wrist. A fluid-filled cyst near the thumb side of your wrist. Your doctor can see if you have de Quervain’s tenosynovitis based on your symptoms and a physical exam. They will also ask you to do certain movements with your hand, wrist, and thumb. -

Common Hand, Wrist and Elbow Problems
12/15/2018 COMMON HAND, WRIST Disclosures AND ELBOW PROBLEMS: Research Support: HOW TO SPOT THEM IN San Francisco DPH CLINIC Standard Cyborg Nicolas H. Lee, MD UCSF Dept of Orthopaedic Surgery Assistant Clinical Professor Hand, Upper Extremity and Microvascular Surgery Dec. 15th, 2018 DIP joint pathologies Mucous Cyst – ganglion cyst of DIP joint 1. Mucous Cyst 2. Mallet Finger 3. Jersey Finger 1 12/15/2018 Xray Treatment “Jammed Finger” Mallet Finger • Recurrence rate with aspiration/needling? 40-70% • Recurrence rate with surgical debridement of osteophyte? Jersey Finger 0-3% • Do nail deformities resolve with surgery? Yes - 75% 2 12/15/2018 Mallet Finger Mallet finger Soft Tissue Mallet • 6 weeks DIP immobilization in extension • Night time splinting for 4 weeks Bony Mallet http://www.specialisedhandtherapy.com.au/ Red Flag Mallet Finger Red Flag Jersey Finger When to Refer: Flexor Digitorum Profundus (FDP) 1. Big fragment strength testing 2. Volar subluxation of the distal phalanx http://nervesurgery.wustl.edu/ http://www.orthobullets.com REFER ALL JERSEY FINGERS ASAP!!! 3 12/15/2018 Trigger Finger and Thumb Trigger finger • Presentation • Clicking or frank locking • Especially at night or morning • May also present with just pain at the A1 pulley Trigger Finger Primary Trigger Finger • Physical Examination • Most Common • Locking or clicking over the A1 pulley • “Idiopathic” • Tenderness at the A1 pulley • No known cause 4 12/15/2018 Secondary “Congenital” • Associated with known disease • Infantile form • Disease cause thickening in tendon/pulley • “congenital” is a misnomer • Diabetes • Rheumatoid arthritis • Amyloidosis • Sarcoidosis Treatment Options Trigger finger Splinting •Nonoperative • Splint to prevent MCP or •Observation PIP flexion. -
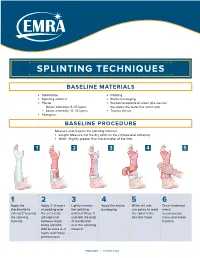
Splinting Techniques
SPLINTING TECHNIQUES BASELINE MATERIALS l Stockinette l Padding l Splinting material l Elastic bandaging l Plaster l Bucket/receptacle of water (the warmer — Upper extremity: 8–10 layers the water, the faster the splint sets) — Lower extremity: 10–12 layers l Trauma shears l Fiberglass BASELINE PROCEDURE Measure and prepare the splinting material. l Length: Measure out the dry splint on the contralateral extremity l Width: Slightly greater than the diameter of the limb 1 2 3 4 5 1 2 3 4 5 6 Apply the Apply 2–3 layers Lightly moisten Apply the elastic While still wet, Once hardened, stockinette to of padding over the splinting bandaging. use palms to mold check extend 2" beyond the area to be material. Place it the splint to the neruovascular the splinting splinted and and fold the ends desired shape. status and motor material. between digits of stockinette function. being splinted. over the splinting Add an extra 2–3 material. layers over bony prominences. EMRA.ORG | 972.550.0920 POSTERIOR LONG ARM VOLAR SPLINT SPLINT INDICATIONS INDICATIONS l Olecranon fractures l Soft tissue injuries of the hand and wrist l Humerus fractures l Carpal bone fractures l Radial head and neck fractures l 2nd–5th metacarpal head fractures CONSTRUCTION CONSTRUCTION l Start at posterior proximal arm l Start at palm at the metacarpal heads l Down the ulnar forearm l Down the volar forearm l End at the metacarpophalangeal joints l End at distal forearm APPLICATION APPLICATION l Cut hole in stockinette for thumb l Cut hole in stockinette for thumb l Elbow at 90º -

Common Elbow Injuries Symptoms
During the summer months, many people stay active by playing golf or tennis. These sports, however, carry a risk of injury to the tendons – bands of tissue that connect muscles to bones – in the elbow. This month’s AT Corner will explain how these injuries happen, how to treat them if they occur and, most importantly, how to prevent them. Common Elbow Injuries Tendonitis: Inflammation, pain and difficulty using the joint caused by repetitive activities and/or sudden trauma. Tendonosis: A degeneration (breakdown) or tear of tendons which occurs as a result of aging. Symptoms of tendonosis usually last more than a few weeks. Note: Your risk of tendonitis and tendonosis increases with age. They also occur more frequently in those who routinely perform activities that require repetitive movement, as this places greater amounts of stress on the tendons. Tennis elbow: Also referred to as lateral epicondylitis, this condition occurs when there is an injury to the outer elbow tendon. Golfers’ elbow: Also referred to as medial epicondylitis, this condition occurs when there is an injury to the inner elbow tendon. Note: Injuries to these tendons can occur in other sports and activities that use the wrist and forearm muscles. Most times, the dominant arm is the one affected. Symptoms • Pain that spreads from the elbow into the upper arm or down the forearm • Forearm weakness • Pain that can begin suddenly or gradually worsen over time • Difficulty with activities that require arm strength Treatment Over-the-counter medications: NSAIDs, such as ibuprofen (Advil®, Motrin®) and naproxen (Aleve®), or acetaminophen (Tylenol®) can provide pain relief. -

Information for Patients About Hand & Elbow Surgery
Information for Patients about Hand & Elbow Surgery Clinical Professor Allan Wang FRACS PhD FAOrthA Shoulder and Upper Limb Surgeon www.allanwangorthopaedics.com.au MURDOCH SUBIACO Murdoch Orthopaedic Clinic St John of God Subiaco Clinic St John of God Murdoch Clinic Suite 302, 25 McCourt St Suite 10, 100 Murdoch Drive Subiaco WA 6008 Murdoch WA 6150 Telephone: 08 6332 6390 Page | 2 Page | 3 Information for Patients about Hand and Elbow Surgery Introduction We have put this information booklet together to educate our patients about their Hand and Elbow condition, treatment options and post-surgical care. Please keep this booklet for future reference. It is not a detailed source of information and you may also wish to refer to our website www.allanwangorthopaedics.com.au for animated videos of surgical procedures. If you require further information or have concerns regarding your treatment please contact the office to discuss with Dr Wang or his staff. Contents Pages 1. Carpal Tunnel Syndrome 4 2. Cubital Tunnel Syndrome 6 3. Trigger Finger 7 4. De Quervain’s Tenodonitis 8 5. Ganglion Cysts 9 6. Arthritis at the Base of the Thumb 10 7. Wrist Arthroscopy 11 8. Dupuytren’s Disease 12 9. Lateral Epicondylitis 13 10. Elbow Arthroscopy 14 11. Post-Operative Instructions Hand & Elbow Surgery 15 Page | 4 Carpal Tunnel Syndrome What is it? Figure 1 Carpal tunnel syndroe is a condition aused by copression o te median nerve at te level o te wrist oint Here te edian nerve passes into te arpal tunnel along wit leor tendons and te tendon lining called tenosynoviu Carpal tunnel syndroe ocurs wen pressure builds up in te tunnel and tis an be due to swelling o te tenosynoviu ratures artritis luid retention during pregnany and certain conditions suc as diabetes and tyroid disease Symptoms en te pressure on te edian nerve becoes severe, you ay notice wrist pain tingling and nubness and lusiness in and oveents. -

Mallet Finger Injuries
Give Me Back My Hand and Fingers- Part 2 Thomas V Gocke, MS, ATC, PA-C, DFAAPA President/Founder Orthopaedic Educational Services, Inc. Boone, North Carolina www.orthoedu.com [email protected] Orthopaedic Educational Services, Inc. © 2016 Orthopaedic Educational Services, Inc. all rights reserved. Faculty Disclosures • Orthopaedic Educational Services, Inc. Financial Intellectual Property No off label product discussions American Academy of Physician Assistants Financial PA Course Director, PA’s Guide to the MSK Galaxy Urgent Care Association of America Financial Intellectual Property Faculty, MSK Workshops Ferring Pharmaceuticals Consultant Orthopaedic 2 Educational Services, Inc. © 2016 Orthopaedic Educational Services, Inc. all rights reserved. Learning Goals Attendees will be able to develop skills in the assessment of ……….. • Hand/Finger Extensor Tendon Injuries • Hand/Finger Flexor Tendon Injuries • Human/Fight Bite wounds to the Fingers • Finger High Pressure Injection Injuries • Metacarpalphalangeal (MCP) joint dislocations • Phalanx fractures • Finger tip trauma Orthopaedic 3 Educational Services, Inc. © 2016 Orthopaedic Educational Services, Inc. all rights reserved. Boutonniere Finger Injuries Orthopaedic Educational Services, Inc. © 2016 Orthopaedic Educational Services, Inc. all rights reserved. • Boutonniere Deformity • Zone II extensor injury • Affects PIP & DIP joints – Extrinsic mechanism: Extensor Digitorium Communis (EDC) – Intrinsic mechanism: Lumbricals • Injury Mechanism – Rupture central slip extensor tendon/hood