Splinting Techniques
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Median Nerve Compression at Pronator Teres
1 Median Nerve Compression at Pronator Teres Surgical Indications and Considerations Anatomical Considerations: The median nerve and brachial artery travel together down the arm. Therefore, one must be very careful not to interfere with either the median nerve or the brachial artery, especially when conducting surgical procedures. In the area of the pronator teres, there are many tendons as well. It is important to identify, as much as possible, the correct site of compression. Pathogenesis: The median nerve can get entrapped or compressed by several structures in the arm. The pronator teres muscle is the most common. Others entrapment sites include the flexor digitorum superficialis arch, the lacertus fibrosis (bicipital aponeurosis), and ligament of Struthers (frequency occurs in that order). For compression of the median nerve at the pronator teres and flexor digitorum superficialis, the cause is almost always due to hypertrophy of the respected muscle. This hypertrophy is from quick, forceful and repeated movements to the involved muscle. Examples include a carpenter or a baseball batter. As the muscle hypertrophies, the signal from the median nerve is diminished resulting in paresthesias in the median nerve distribution (lateral arm and hand) distal to the site of compression. Pain in the volar part of the forearm, often aggravated by repetitive supination and pronation, is a common symptom of pronator involvement. Another indicator is forearm pain with the compression of muscle such as pain in the volar part of the forearm implicating pronator teres. Onset is typically insidious and diagnosis is usually delayed 9 months to 2 years. Epidemiology: Pronator teres syndrome is the second most common cause of median nerve compression behind carpal tunnel syndrome. -
ICD-10 Diagnoses on Router
L ARTHRITIS R L HAND R L ANKLE R L FRACTURES R OSTEOARTHRITIS: PRIMARY, 2°, POST TRAUMA, POST _____ CONTUSION ACHILLES TEN DYSFUNCTION/TENDINITIS/RUPTURE FLXR TEN CLAVICLE: STERNAL END, SHAFT, ACROMIAL END CRYSTALLINE ARTHRITIS: GOUT: IDIOPATHIC, LEAD, CRUSH INJURY AMPUTATION TRAUMATIC LEVEL SCAPULA: ACROMION, BODY, CORACOID, GLENOID DRUG, RENAL, OTHER DUPUYTREN’S CONTUSION PROXIMAL HUMERUS: SURGICAL NECK 2 PART 3 PART 4 PART CRYSTALLINE ARTHRITIS: PSEUDOGOUT: HYDROXY LACERATION: DESCRIBE STRUCTURE CRUSH INJURY PROXIMAL HUMERUS: GREATER TUBEROSITY, LESSER TUBEROSITY DEP DIS, CHONDROCALCINOSIS LIGAMENT DISORDERS EFFUSION HUMERAL SHAFT INFLAMMATORY: RA: SEROPOSITIVE, SERONEGATIVE, JUVENILE OSTEOARTHRITIS PRIMARY/SECONDARY TYPE _____ LOOSE BODY HUMERUS DISTAL: SUPRACONDYLAR INTERCONDYLAR REACTIVE: SECONDARY TO: INFECTION ELSEWHERE, EXTENSION OR NONE INTESTINAL BYPASS, POST DYSENTERIC, POST IMMUNIZATION PAIN OCD TALUS HUMERUS DISTAL: TRANSCONDYLAR NEUROPATHIC CHARCOT SPRAIN HAND: JOINT? OSTEOARTHRITIS PRIMARY/SECONDARY TYPE _____ HUMERUS DISTAL: EPICONDYLE LATERAL OR MEDIAL AVULSION INFECT: PYOGENIC: STAPH, STREP, PNEUMO, OTHER BACT TENDON RUPTURES: EXTENSOR OR FLEXOR PAIN HUMERUS DISTAL: CONDYLE MEDIAL OR LATERAL INFECTIOUS: NONPYOGENIC: LYME, GONOCOCCAL, TB TENOSYNOVITIS SPRAIN, ANKLE, CALCANEOFIBULAR ELBOW: RADIUS: HEAD NECK OSTEONECROSIS: IDIOPATHIC, DRUG INDUCED, SPRAIN, ANKLE, DELTOID POST TRAUMATIC, OTHER CAUSE SPRAIN, ANKLE, TIB-FIB LIGAMENT (HIGH ANKLE) ELBOW: OLECRANON WITH OR WITHOUT INTRA ARTICULAR EXTENSION SUBLUXATION OF ANKLE, -

Fundamental Shoulder Exercises
FUNDAMENTAL SHOULDER EXERCISES RANGE OF MOTION EXERCISES 1. L-BAR FLEXION Lie on back and grip L-Bar between index finger and thumb, elbows straight. Raise both arms overhead as far as possible keeping thumbs up. Hold for _____ seconds and repeat _____ times. 2. L-BAR EXTERNAL ROTATION, SCAPULAR PLANE Lie on back with involved arm 450 from body and elbow bent at 900. Grip L-Bar in the hand of involved arm and keep elbow in flexed position. Using unin- volved arm, push involved arm into external rotation. Hold for _____ seconds, return to starting position. Repeat _____ times. 3. L-BAR INTERNAL ROTATION, SCAPULAR PLANE Lie on back with involved arm 450 from body and elbow bent at 900. Grip L-Bar in the hand of involved arm and keep elbow in flexed position. Using the uninvolved arm, push involved arm into internal rotation. Hold for _____ seconds, return to starting position. Repeat _____ times. Dr. Meisterling (800) 423-1088 1 of 2 STRENGTHENING EXERCISES 1. TUBING, EXTERNAL ROTATION Standing with involved elbow fixed at side, elbow bent to 900 and involved arm across the front of the body. Grip tubing handle while the other end of tubing is fixed. Pull out with arm, keeping elbow at side. Return tubing slowly and controlled. Perform _____ sets of _____ reps. 2. TUBING, INTERNAL ROTATION Standing with elbow at side fixed at 900 and shoulder rotated out. Grip tubing handle while other end of tubing is fixed. Pull arm across body keeping elbow at side. Return tubing slowly and controlled. -

Upper Extremity
Upper Extremity Shoulder Elbow Wrist/Hand Diagnosis Left Right Diagnosis Left Right Diagnosis Left Right Adhesive capsulitis M75.02 M75.01 Anterior dislocation of radial head S53.015 [7] S53.014 [7] Boutonniere deformity of fingers M20.022 M20.021 Anterior dislocation of humerus S43.015 [7] S43.014 [7] Anterior dislocation of ulnohumeral joint S53.115 [7] S53.114 [7] Carpal Tunnel Syndrome, upper limb G56.02 G56.01 Anterior dislocation of SC joint S43.215 [7] S43.214 [7] Anterior subluxation of radial head S53.012 [7] S53.011 [7] DeQuervain tenosynovitis M65.42 M65.41 Anterior subluxation of humerus S43.012 [7] S43.011 [7] Anterior subluxation of ulnohumeral joint S53.112 [7] S53.111 [7] Dislocation of MCP joint IF S63.261 [7] S63.260 [7] Anterior subluxation of SC joint S43.212 [7] S43.211 [7] Contracture of muscle in forearm M62.432 M62.431 Dislocation of MCP joint of LF S63.267 [7] S63.266 [7] Bicipital tendinitis M75.22 M75.21 Contusion of elbow S50.02X [7] S50.01X [7] Dislocation of MCP joint of MF S63.263 [7] S63.262 [7] Bursitis M75.52 M75.51 Elbow, (recurrent) dislocation M24.422 M24.421 Dislocation of MCP joint of RF S63.265 [7] S63.264 [7] Calcific Tendinitis M75.32 M75.31 Lateral epicondylitis M77.12 M77.11 Dupuytrens M72.0 Contracture of muscle in shoulder M62.412 M62.411 Lesion of ulnar nerve, upper limb G56.22 G56.21 Mallet finger M20.012 M20.011 Contracture of muscle in upper arm M62.422 M62.421 Long head of bicep tendon strain S46.112 [7] S46.111 [7] Osteochondritis dissecans of wrist M93.232 M93.231 Primary, unilateral -

Early Passive Motion After Surgery
www.western -ortho.com www.denvershoulder.com Early Passive Motion after Shoulder Surgery Passive motion involves someone else moving the affected arm through the motion described. Or, in the case of elbow flexion/extension, you can use your opposite (non-affected arm) to move through the motion. Do 5 repetitions of each stretch 3 times per day. When you feel a slight ‘tightness’ with your arm in the position diagrammed, hold that position for 30 seconds. If lying down is difficult, the stretches can be done while seated. Shoulder Flexion Support arm at the wrist and elbow. With the thumb pointed forward, gently bring the arm up and forward then back to the side. Shoulder Abduction Support arm at wrist and elbow. With the thumb pointed away from the body and palm up, gently bring the arm out to the side. www.western -ortho.com www.denvershoulder.com Shoulder Internal/External Rotation Support arm at wrist and elbow. With the elbow at the side and bent to a 90 degree angle, gently rotate the hand away from the body down toward the table the individual is lying on. Elbow Flexion/Extension Forearm Pronation/Supination Grasp the wrist of your affected arm with your unaffected With your elbow and forearm supported on a table, hand. With your affected elbow against your side and your gently turn forearm so your palm is down, then turn palm up, gently bend and straighten your elbow. forearm so your palm is up. This can be done actively (without assistance from your other hand). . -

Pronator Syndrome: Clinical and Electrophysiological Features in Seven Cases
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.39.5.461 on 1 May 1976. Downloaded from Journal ofNeurology, Neurosurgery, and Psychiatry, 1976, 39, 461-464 Pronator syndrome: clinical and electrophysiological features in seven cases HAROLD H. MORRIS AND BRUCE H. PETERS From the Department ofNeurology, University of Texas Medical Branch, Galveston, Texas, USA SYNOPSIS The clinical and electrophysiological picture of seven patients with the pronator syndrome is contrasted with other causes ofmedian nerve neuropathy. In general, these patients have tenderness over the pronator teres and weakness of flexor pollicis longus as well as abductor pollicis brevis. Conduction velocity of the median nerve in the proximal forearm is usually slow but the distal latency and sensory nerve action potential at the wrist are normal. Injection of corticosteroids into the pronator teres has produced relief of symptoms in a majority of patients. Protected by copyright. In the majority of isolated median nerve dys- period 101 cases of the carpal tunnel syndrome functions the carpal tunnel syndrome is appropri- and the seven cases of the pronator syndrome ately first suspected. The median nerve can also reported here were identified. Median nerve be entrapped in the forearm giving rise to a conduction velocity determinations were made on similar picture and an erroneous diagnosis. all of these patients. The purpose of this report is to draw full attention to the pronator syndrome and to the REPORT OF CASES features which allow it to be distinguished from Table 1 provides clinical details of seven cases of the median nerve entrapment at other sites. -

2014 Newsletter – Winter
NEWS ISSUE 14 I WINTER 2014 Welcome to our Winter edition of Orthosports News Winter is the time when Alpine Injuries present themselves WHO ORTHOSPORTS – Dr Doron Sher covers the most common types of alpine ARE WE? LOCATIONS injuries. Dr Kwan Yeoh takes a look at Mallet Finger and Orthosports is > Concord 02 9744 2666 “Imaging of the knee” is covered by Dr Sher in our Key a professional > Hurstville 02 9580 6066 Examination Points Section. association of > Penrith 02 4721 7799 Many GPs have attended our Category 1 Education Modules; AOA Orthopaedic > Randwick 02 9399 5333 A USTRAL I A N ORTHOPA EDIC Surgeons based Or visit our website there are 4 remaining dates for our 2014 RACGP approved A S S O CIA T I O N modules. See page 4 for details. in Sydney. www.orthosports.com.au We hope you enjoy this issue – The Team at Orthosports elbow injuries and more comminuted clavicle fractures. Alpine Injuries Shoulder dislocation is also very common. Snowboarders do not usually injure their legs when both feet are attached Skiing and snowboarding are exhilarating sports. They to the board but injuries to the knee are not uncommon are physically demanding and require co-ordination, getting on and off lifts when only one foot is bound to the strength, fitness and lots of specialized equipment. More board (more common in beginners). If they do injure their people ski than snowboard and snowboarders are generally knee, it is almost always in a terrain park landing from younger than skiers. Skiing and snowboarding injuries a big jump. -
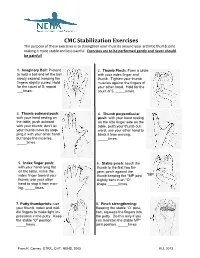
CMC Stabilization Exercises the Purpose of These Exercises Is to Strengthen Your Muscles Around Your Arthritic Thumb Joint Making It More Stable and Less Painful
CMC Stabilization Exercises The purpose of these exercises is to strengthen your muscles around your arthritic thumb joint making it more stable and less painful. Exercises are to be performed gently and never should be painful! 1. Imaginary Ball: Pretend 2. Thumb Pinch: Form a circle to hold a ball and let the ball with your index finger and slowly expand, keeping the thumb. Tighten your thumb fingers slightly curled. Hold muscles against the fingers of for the count of 5, repeat your other hand. Hold for the ___times. count of 5, _____times. 3. Thumb outward push: 4. Thumb perpendicular with your hand resting on push: with your hand resting the table, push outward on the little finger side on the with your thumb; don’t let table, push your thumb out- your thumb move by stop- ward; use your other hand to ping it with your other hand block it from moving. but tense the muscles. _____times. _____times. 5. Index finger push: 6. Stable pinch: touch the with your hand lying flat thumb to the first two fin- on the table, move the gers; pinch against the index finger toward your thumb keeping the *MP joint *MP thumb; use your other slightly bent in an “O” hand to stop it from mov- shape. _____times. ing. _____times. 7. Putty thumbprints: use 8. Pinch strengthening: your thumb, index and mid- Keeping the stable “O” posi- dle fingers to make light im- tion, squeeze the fingers into pressions in the putty. Keep the putty. Do this only if you the stable “O” position. -

Hughston Health Alert US POSTAGE PAID the Hughston Foundation, Inc
HughstonHughston HealthHealth AlertAlert 6262 Veterans Parkway, PO Box 9517, Columbus, GA 31908-9517 • www.hughston.com/hha VOLUME 26, NUMBER 4 - FALL 2014 Fig. 1. Knee Inside... anatomy and • Rotator Cuff Disease ACL injury. Extended (straight) knee • Bunions and Lesser Toe Deformities Femur • Tendon Injuries of the Hand (thighbone) Patella In Perspective: (kneecap) Anterior Cruciate Ligament Tears Medial In 1992, Dr. Jack C. Hughston (1917-2004), one of the meniscus world’s most respected authorities on knee ligament surgery, MCL LCL shared some of his thoughts regarding injuries to the ACL. (medial “You tore your anterior cruciate ligament.” On hearing (lateral collateral collateral your physician speak those words, you are filled with a sense ligament) of dread. You envision the end of your athletic life, even ligament) recreational sports. Today, a torn ACL (Fig. 1) has almost become a household Tibia word. Through friends, newspapers, television, sports Fibula (shinbone) magazines, and even our physicians, we are inundated with the hype that the knee joint will deteriorate and become arthritic if the ACL is not operated on as soon as possible. You have been convinced that to save your knee you must Flexed (bent) knee have an operation immediately to repair the ligament. Your surgery is scheduled for the following day. You are scared. Patella But there is an old truism in orthopaedic surgery that says, (kneecap) “no knee is so bad that it can’t be made worse by operating Articular Torn ACL on it.” cartilage (anterior For many years, torn ACLs were treated as an emergency PCL cruciate and were operated on immediately, even before the initial (posterior ligament) pain and swelling of the injury subsided. -

Post-Operative Instructions for Flexor Tendon Repair Purpose of Surgery
Post-Operative Instructions for Flexor Tendon Repair Purpose of surgery The goal of the operation is to repair or reattach lacerated or detached flexor tendons. The flexor tendons (muscles) are responsible for flexing (bending) your fingers. What to expect after surgery? You will have a firm splint covering your forearm and the back of your hand and fingers holding your fingers flexed (bent). All your fingers will be included in the splint for any finger flexor tendon repair; and, only your thumb will be included in the splint for a thumb flexor tendon repair. You will be able to see the tips of your fingers/thumb to insure they are getting good circulation. The palm side of your fingers/thumb will be protected by a soft padding that they will be resting on while the plaster will keep your fingers bent from the nail side. You may have some numbness or tingling of fingers/thumb due to the local anesthetic injections used to help control post-operative pain (this should wear off within about 24 hours). After this first 24 hours, you may still experience some numbness and tingling in parts of the operative finger(s)/thumb if you also had a nerve repair. What should you do to help recover? While we do not anticipate significant swelling following this procedure, it would be helpful to keep your hand/wrist elevated as best you can for the first 24 hours after surgery. The thickness of the dressing will prevent the effective placement of a cold-pack. Please do not move your fingers, even if they were not operated on. -

Hand Rehabilitation Current Awareness Newsletter
1 Hand Rehabilitation Current Awareness Newsletter JANUARY 2016 2 Your Local Librarian Whatever your information needs, the library is here to help. As your outreach librarian I offer literature searching services as well as training and guidance in searching the evidence and critical appraisal – just email me at library @uhbristol.nhs.uk OUTREACH: Your Outreach Librarian can help facilitate evidence-based practise for all in the Orthogeriatrics team, as well as assisting with academic study and research. We can help with literature searching, obtaining journal articles and books, and setting up individual current awareness alerts. We also offer one-to-one or small group training in literature searching, accessing electronic journals, and critical appraisal. Get in touch: [email protected] LITERATURE SEARCHING: We provide a literature searching service for any library member. For those embarking on their own research it is advisable to book some time with one of the librarians for a 1 to 1 session where we can guide you through the process of creating a well-focused literature research and introduce you to the health databases access via NHS Evidence. Please email requests to [email protected] 3 Contents New from Cochrane Database of Systematic Reviews ........................................................................... 4 Abstract .................................................................................................................................................. 4 New Activity in Up-to-Date .................................................................................................................... -

Self Range of Motion Exercises for Arm and Hand
Self-Range of Motion Exercises for the Arm and Hand After a stroke, it is important to do the exercises in this handout for your affected arm and hand. You can do them on your own by using your unaffected arm and hand. These gentle movements are called “self-range of motion” exercises, and they help to maintain your movement, prevent stiffness, improve blood flow, and increase awareness of your affected arm and hand. Complete the exercises slowly and do not force movements. Stop if you feel pain. If you have any questions or concerns, please contact your Occupational Therapist: _______________________________ Do the exercises in this handout _____ times each day. Page - 1 Self-range of motion exercises for the arm and hand 1. Shoulder: Forward Arm Lift Interlock your fingers, or hold your wrist. With your elbows straight and thumbs facing the ceiling, lift your arms to shoulder height. Slowly lower your arms to starting position. Hold for ____ seconds. Repeat ____ times. Page - 2 Self-range of motion exercises for the arm and hand 2. Shoulder: “Rock the Baby” Stretch Hold your affected arm by supporting the elbow, forearm and wrist (as if cradling a baby). Slowly move your arms to the side, away from your body, lifting to shoulder height. Repeat this motion in the other direction. Slowly rock your arms side-to-side, and keep your body from turning. Repeat ____ times. Page - 3 Self-range of motion exercises for the arm and hand 3. Shoulder: Rotation Stretch Interlock your fingers, or hold your wrist. With your elbows bent at 90 degrees, keep your affected arm at your side.