De Quervain's Tenosynovitis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Multiple Pulley Rupture Following Corticosteroid Injection for Trigger Digit: Case Report
SCIENTIFIC ARTICLE Multiple Pulley Rupture Following Corticosteroid Injection for Trigger Digit: Case Report Cassie Gyuricza, MD, Eva Umoh, BA, Scott W. Wolfe, MD We report a case of pulley rupture following repeated local corticosteroid injections for trigger digit. The treatment involved exploration, tenolysis, and reconstruction using the palmaris longus tendon. (J Hand Surg 2009;34A:1444–1448. © 2009 Published by Elsevier Inc. on behalf of the American Society for Surgery of the Hand.) Key words Corticosteroid, pulley rupture, trigger digit. RIGGER DIGIT, OR stenosing tenosynovitis,isa local corticosteroid injection through a lateral approach condition characterized by painful locking or at the proximal phalanx10 (0.5 mL local anesthetic and Tsnapping of a digit caused by mechanical im- 0.5 mL triamcinolone acetonide 40 mg/mL [Kenalog- pingement of the flexor tendon passing through a hy- 40, Bristol-Meyers Squibb Co, Princeton, NJ]). Her pertrophic A1 pulley. Initial conservative management symptoms of pain temporarily improved, but 4 months of trigger digits with various corticosteroid preparations later, the patient returned with recurrent pain and a is well described.1–4 Side effects, including subcutane- second local corticosteroid injection was administered, ous fat atrophy, pain, depigmentation of the skin, and again using the lateral approach. During the ensuing 8 transient elevation of urine and blood glucose levels in months, the patient had persistent pain and tenderness patients with diabetes, are generally mild and self- over the A2 pulley. The patient also developed pain at limiting.5,6 We are aware of 2 previously reported cases the A1 pulley, and a third injection (0.5 mL local of delayed flexor tendon rupture following corticoste- anesthetic and 0.5 mL triamcinolone acetonide 40 mg/ 7,8 roid injections for trigger digit thought to be the result mL) was given into the palmar surface overlying the A1 of intratendinous injection. -

Fundamental Shoulder Exercises
FUNDAMENTAL SHOULDER EXERCISES RANGE OF MOTION EXERCISES 1. L-BAR FLEXION Lie on back and grip L-Bar between index finger and thumb, elbows straight. Raise both arms overhead as far as possible keeping thumbs up. Hold for _____ seconds and repeat _____ times. 2. L-BAR EXTERNAL ROTATION, SCAPULAR PLANE Lie on back with involved arm 450 from body and elbow bent at 900. Grip L-Bar in the hand of involved arm and keep elbow in flexed position. Using unin- volved arm, push involved arm into external rotation. Hold for _____ seconds, return to starting position. Repeat _____ times. 3. L-BAR INTERNAL ROTATION, SCAPULAR PLANE Lie on back with involved arm 450 from body and elbow bent at 900. Grip L-Bar in the hand of involved arm and keep elbow in flexed position. Using the uninvolved arm, push involved arm into internal rotation. Hold for _____ seconds, return to starting position. Repeat _____ times. Dr. Meisterling (800) 423-1088 1 of 2 STRENGTHENING EXERCISES 1. TUBING, EXTERNAL ROTATION Standing with involved elbow fixed at side, elbow bent to 900 and involved arm across the front of the body. Grip tubing handle while the other end of tubing is fixed. Pull out with arm, keeping elbow at side. Return tubing slowly and controlled. Perform _____ sets of _____ reps. 2. TUBING, INTERNAL ROTATION Standing with elbow at side fixed at 900 and shoulder rotated out. Grip tubing handle while other end of tubing is fixed. Pull arm across body keeping elbow at side. Return tubing slowly and controlled. -

Top Hand, and Wrist Problems
12/10/2016 TOP HAND, AND WRIST Disclosures PROBLEMS: HOW TO • None SPOT THEM IN CLINIC Nicolas H. Lee, MS MD [email protected] UCSF Dept of Orthopaedic Surgery Assistant Clinical Professor Hand, Upper Extremity and Microvascular Surgery Dec. 10 th , 2016 Outline Outline • Carpal Tunnel Syndrome •Carpal Tunnel Syndrome • Trigger Finger • • Basal Joint arthritis Trigger Finger • Basal Joint arthritis • De Quervain tenosynovitis • De Quervain tenosynovitis • Mallet Finger • Mallet Finger • Ganglion cyst • Ganglion cyst 1 12/10/2016 Carpal Tunnel Syndrome • Compression of median nerve in carpal tunnel • Irritation of the nerve presents as numbness/pain 10 structures 9 flexor tendons Median nerve https://www.pinterest.com/pin/429812358163325007/ Anatomy (motor) Etiology 1. Idiopathic – most common 2. Anatomic – rare • Thenar Muscle (OAF) 3. Systemic – DM, hypothyroidism • Opponens Pollicis (deep) 4. **** Occupational Exposure • Abductor Pollicis Brevis (superficial) **** “A direct relationship between repetitive work • Flexor Pollicis Brevis activity (eg, keyboarding) and CTS has never been (superficial 1/2) objectively demonstrated.” 1 http://teachmeanatomy.info/upper-limb/muscles/hand/ 2 12/10/2016 Rare anatomic causes Carpal Tunnel Syndrome ● HPI – systemic risk factors Tenosynovitis CMC arthritis ◦ More common in: Ganglion Fracture 1) Diabetics 2) Hypothyroidism 3) Pregnancy (20-45%) Persistent Median artery Acromegaly Abnormal muscle Tumor Carpal Tunnel Syndrome ● CC: ◦ “I wake up at night and my hands are asleep” ◦ “I have to shake them to get the blood flowing again” ◦ “I have to run them under warm water and then I can go back to sleep” ◦ “Fingers go numb when I drive” ◦ “My hand goes numb when I use my cell phone” ◦ “I am always dropping things” Carpal Tunnel Syndrome Cranford, C.S. -
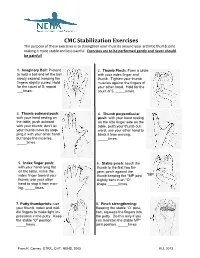
CMC Stabilization Exercises the Purpose of These Exercises Is to Strengthen Your Muscles Around Your Arthritic Thumb Joint Making It More Stable and Less Painful
CMC Stabilization Exercises The purpose of these exercises is to strengthen your muscles around your arthritic thumb joint making it more stable and less painful. Exercises are to be performed gently and never should be painful! 1. Imaginary Ball: Pretend 2. Thumb Pinch: Form a circle to hold a ball and let the ball with your index finger and slowly expand, keeping the thumb. Tighten your thumb fingers slightly curled. Hold muscles against the fingers of for the count of 5, repeat your other hand. Hold for the ___times. count of 5, _____times. 3. Thumb outward push: 4. Thumb perpendicular with your hand resting on push: with your hand resting the table, push outward on the little finger side on the with your thumb; don’t let table, push your thumb out- your thumb move by stop- ward; use your other hand to ping it with your other hand block it from moving. but tense the muscles. _____times. _____times. 5. Index finger push: 6. Stable pinch: touch the with your hand lying flat thumb to the first two fin- on the table, move the gers; pinch against the index finger toward your thumb keeping the *MP joint *MP thumb; use your other slightly bent in an “O” hand to stop it from mov- shape. _____times. ing. _____times. 7. Putty thumbprints: use 8. Pinch strengthening: your thumb, index and mid- Keeping the stable “O” posi- dle fingers to make light im- tion, squeeze the fingers into pressions in the putty. Keep the putty. Do this only if you the stable “O” position. -

Post-Operative Instructions for Flexor Tendon Repair Purpose of Surgery
Post-Operative Instructions for Flexor Tendon Repair Purpose of surgery The goal of the operation is to repair or reattach lacerated or detached flexor tendons. The flexor tendons (muscles) are responsible for flexing (bending) your fingers. What to expect after surgery? You will have a firm splint covering your forearm and the back of your hand and fingers holding your fingers flexed (bent). All your fingers will be included in the splint for any finger flexor tendon repair; and, only your thumb will be included in the splint for a thumb flexor tendon repair. You will be able to see the tips of your fingers/thumb to insure they are getting good circulation. The palm side of your fingers/thumb will be protected by a soft padding that they will be resting on while the plaster will keep your fingers bent from the nail side. You may have some numbness or tingling of fingers/thumb due to the local anesthetic injections used to help control post-operative pain (this should wear off within about 24 hours). After this first 24 hours, you may still experience some numbness and tingling in parts of the operative finger(s)/thumb if you also had a nerve repair. What should you do to help recover? While we do not anticipate significant swelling following this procedure, it would be helpful to keep your hand/wrist elevated as best you can for the first 24 hours after surgery. The thickness of the dressing will prevent the effective placement of a cold-pack. Please do not move your fingers, even if they were not operated on. -

Your Guide to Trigger Finger Surgery Brian J
Your Guide to Trigger Finger Surgery Brian J. Bear, MD OrthoIllinois Hand, Wrist, and Elbow Center of Excellence Care Team and Contact Numbers: Brian J. Bear, MD Main Phone line . 815-398-9491 OrthoIllinois Kailey - Lead Nurse . .815-398-9491 324 Roxbury Road Ronda - Surgery Scheduler . 815-484-6969 Rockford, IL Sadie - Office Scheduler . .815-484-6996 TABLE OF CONTENTS Learn about Dr. Bear . 2 What is Trigger Finger/Trigger Thumb?. 3 Surgical Treatment v Description of Trigger Finger Release . 3 The Surgical Experience v Information to Keep in Mind Prior to Surgery . 4 v Pre-Admission Guide for Surgery . 5 v Pre-operative Phase . 6 v Intra-operative Phase . 7 v Post-operative Phase . 8 After Surgery v While You Recover at Home . 9 Commonly Asked Questions . 10-11 What Can I Do After Surgery? . 13 1 Learn More About Dr. Bear I would like to take this opportunity to tell you more about myself and my experience in health care. Originally from Winnetka, Illinois, I attended Northwestern University graduating in 1987, cum laude, president of Mortar Board Senior Honor Society and a member of Phi Betta Kappa. I continued my studies at Northwestern University School of Medicine, receiving my medical degree in 1991 as a member of Alpha Omega Alpha honor society. Following my graduation, I pursued advanced orthopedic training at Cornell Hospital for Special Surgery, which is ranked as the top orthopedic hospital in the United States. In addition, I completed a specialized training fellowship program in elbow and hand surgery at the Mayo Clinic. My practice is focused on shoulder, elbow, hand, microvascular, traumatic, and reconstructive surgery. -

Self Range of Motion Exercises for Arm and Hand
Self-Range of Motion Exercises for the Arm and Hand After a stroke, it is important to do the exercises in this handout for your affected arm and hand. You can do them on your own by using your unaffected arm and hand. These gentle movements are called “self-range of motion” exercises, and they help to maintain your movement, prevent stiffness, improve blood flow, and increase awareness of your affected arm and hand. Complete the exercises slowly and do not force movements. Stop if you feel pain. If you have any questions or concerns, please contact your Occupational Therapist: _______________________________ Do the exercises in this handout _____ times each day. Page - 1 Self-range of motion exercises for the arm and hand 1. Shoulder: Forward Arm Lift Interlock your fingers, or hold your wrist. With your elbows straight and thumbs facing the ceiling, lift your arms to shoulder height. Slowly lower your arms to starting position. Hold for ____ seconds. Repeat ____ times. Page - 2 Self-range of motion exercises for the arm and hand 2. Shoulder: “Rock the Baby” Stretch Hold your affected arm by supporting the elbow, forearm and wrist (as if cradling a baby). Slowly move your arms to the side, away from your body, lifting to shoulder height. Repeat this motion in the other direction. Slowly rock your arms side-to-side, and keep your body from turning. Repeat ____ times. Page - 3 Self-range of motion exercises for the arm and hand 3. Shoulder: Rotation Stretch Interlock your fingers, or hold your wrist. With your elbows bent at 90 degrees, keep your affected arm at your side. -

Laparoscopic Sacralcolpopexy and Enterocele Repair with Mesh
124 State of the Art Atlas and Textbook of Laparoscopic Suturing INTRODUCTION The anatomy, pathophysiology, and treatment of pelvic organ prolapse has significantly evolved over the last decade with increasing understanding of anatomy and development of minimally invasive surgical procedures. Although support for the pelvic viscera, the vagina, and neighboring structures involves a complex interplay between muscles, fascia, nerve supply, and appropriate anatomic orientation, the endopelvic fascia and pelvic floor muscles provide most of the support function in the female pelvis. Laparoscopic reconstructive pelvic surgery requires a thorough knowledge of pelvic floor anatomy and its supportive components before repair of defective anatomy is attempted. This chapter reviews the Fig. 13.1: Level 1 (apical suspension) and level 2 (lateral anatomy and laparoscopic repair of vaginal vault attachment). Level 1—paracolpium suspends the vagina apex prolapse and enterocele with Y-mesh sacralcolpopexy. from the lateral pelvic sidewall via the uterosacral-cardinal complex. Level 2—the anterior vaginal wall is attached laterally ANATOMY OF PELVIC SUPPORT to arcus tendinous fascia pelvis and the posterior vaginal wall is attached laterally to the fascia overlying the levator ani Endopelvic Fascia muscle To understand the pelvic support system of the female pelvic organs, it is useful to subdivide the third of the vagina to the bony sacrum. This complex pelvic support system into three axes: can be described as two separate entities: the cardinal 1. The upper vertical axis ligament and the uterosacral ligament. The cardinal 2. The midhorizontal axis ligament is a fascial sheath of collagen that envelops 3. The lower vertical axis. the internal iliac vessels and then continues along The endopelvic fascia—a network of connective the uterine artery, merging into the visceral capsule tissue and smooth muscle—constitutes the physical of the cervix, lower uterine segment and upper matrix which envelops the pelvic viscera and main- vagina. -

Trigger Finger
PATIENT EDUCATION Trigger Finger Trigger Finger "Trigger finger" sounds like a malady that might affect gunslingers or hunters. In fact, this common condition results in a finger bent as if to pull a trigger. People over 40 years of age with a history of diabetes or rheumatoid arthritis are especially at risk to develop this condition. How it develops Although the exact cause of trigger finger is unknown, the progression of the condition is well documented. Trigger finger involves the tendons and pulleys in the hand that bend the finger. The tendons connect the muscles of the forearm with the bones of the fingers. Each tendon is covered by a slick lining or sheath. When you bend your fingers, the tendons glide back and forth, guided by a restraining pulley or yoke. When the tendon sheath becomes inflamed, it swells and may develop a knot or thickening in the tendon. The knot passes through the pulley as the finger bends, but gets stuck as the finger straightens. This causes further irritation and results in a vicious circle of irritation, swelling, catching and more irritation until finally, the finger locks in a bent position. Diagnosis No Xrays are needed to diagnose trigger finger. Your doctor will examine your hand and fingers, and use the findings to make the diagnosis. The finger may be swollen and there may be a bump, or nodule, over the joint in the palm of the hand. The finger may be stiff and painful. Although it may seem that the problem is in the knuckles, it is actually at the joint nearest the palm of the hand. -

Upper Extremity Extensor Tendon Repair Protocol
Department of Rehabilitation Services Primary Upper Extremity and Hand Extensor Tendon Repair Protocol This protocol is not intended to be a substitute for one’s clinical decision making regarding the progression of a patient’s post-operative course based on their physical exam/findings, individual progress, and/or the presence of post-operative complications. If a clinician requires assistance in the progression of a patient, they should consult with the referring surgeon. The time frames of phases I-IV are examples and can be adjusted based on the given procedure. Progression to the next phase based on the clinical criteria and/or time frames, as appropriate. MALLET FINGER: ZONE I: Over the distal phalangeal joint (DIP)-Mallet deformity ZONE II: Over the middle phalanx/triangular ligament Goal: Protect extensor zone I and II with DIP held in extension with PIP joint free. Photo: Wikem.org/w/index.php?title Precautions: During orthotic/cast check out, keep DIP joints fully extended 100%. Frequency: one to two times/week for 6 to 10 weeks if needed for orthosis/cast checks. Primary Extensor Tendon Repair Protocol Copyright © 2020 The Brigham and Women's Hospital, Inc., Department of Rehabilitation Services. All rights reserved 1 PHASE ORTHOTIC THERAPEUTIC EXERCISE: CONSIDERATIONS: ongoing treatment is variable. Phase I immediate phase: Orthosis or circumferential cast Active PIP flexion of affected Patient to perform daily skin day 1 to 6 to 8 weeks. finger with adjacent finger(s) held check while keeping DIP Non-op: DIP 10°-0 in extension. extended. hyperextension for tendinous mallet 6-8 weeks. Consider taping DIP in extension. -

De Quervain's Tenosynovitis
PATIENT & CAREGIVER EDUCATION De Quervain's Tenosynovitis This information explains the causes, symptoms, and treatment of de Quervain’s tenosynovitis (da-cur-vains teno-sin-o-vitis). De Quervain’s tenosynovitis is a common and painful condition that affects the tendons (tissue that connects muscles to bones) of the wrist. A tendon sheath (protective covering) wraps around these tendons so that they can slide easily (see Figure 1). This allows you to turn your wrist, grip, and pinch with your hand. With de Quervain’s tenosynovitis, the tendon sheath becomes swollen. This causes pain and limited movement in your wrist and thumb. Figure 1. Wrist with De Quervain’s tenosynovitis Causes of De Quervain’s Tenosynovitis Some causes of de Quervain’s tenosynovitis include: Overusing your wrist with repetitive movements, such as: Typing Knitting De Quervain's Tenosynovitis 1/4 Using a hammer Holding an infant for a long time Carrying heavy grocery bags Strain or injury to the wrist area. Conditions that cause swelling throughout the body, such as rheumatoid arthritis. Symptoms of De Quervain’s Tenosynovitis De Quervain’s tenosynovitis can cause different symptoms, such as: Pain at the side of your wrist under the base of your thumb. Moving your thumb can increase this pain. Wrist pain that has spread into your forearm and thumb. Mild swelling, redness, or warmth at your wrist. A fluid-filled cyst near the thumb side of your wrist. Your doctor can see if you have de Quervain’s tenosynovitis based on your symptoms and a physical exam. They will also ask you to do certain movements with your hand, wrist, and thumb. -

CONSTRUCTION WORK and CUMULATIVE TRAUMA DISORDERS What Are Cumulative Trauma Disorders?
Connecticut Department of Public Health Environmental and Occupational Health Assessment Program 410 Capitol Avenue MS # 11OSP, PO Box 340308 Hartford, CT 06134-0308 (860) 509-7740 http://www.ct.gov/dph CONSTRUCTION WORK and CUMULATIVE TRAUMA DISORDERS What are Cumulative Trauma Disorders? Cumulative trauma disorders (CTDs) also known as repetitive strain injuries, repetitive motion disorders, overuse syndrome, and work-related musculoskeletal disorders are the largest cause of occupational disease in the United States and the most frequently reported type of occupational disease in Connecticut. CTDs are injuries of the musculoskeletal system (joints, muscles, tendons, ligaments, nerves, and blood vessels) which are caused by over use as a result of stressful work over a period of time. CTDs are usually caused by a combination of the following risk factors common to construction work: • repetitive motions • forceful exertions - pulling, pushing, lifting, and gripping • awkward postures - body positions that are not the natural resting position • static postures - body positions held without moving • mechanical compression of soft tissues in the hand against edges or ridges, such as using tools or objects which press against the palm • fast movement of body parts • vibration, especially in the presence of cold conditions • lack of sufficient recovery time (rest breaks, days off), which will increase the risk of developing a CTD by any of the above factors. Cumulative trauma disorders most often occur in the upper body. Common symptoms of CTDs include pain and swelling of the body parts that are performing work duties involving the above risk factors. Although back injuries are excluded from the definition of CTDs, back injuries are often caused by similar risk factors and occur quite frequently in construction workers.