ED Elbow and Forearm Fractures Safety Checklist
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Median Nerve Compression at Pronator Teres
1 Median Nerve Compression at Pronator Teres Surgical Indications and Considerations Anatomical Considerations: The median nerve and brachial artery travel together down the arm. Therefore, one must be very careful not to interfere with either the median nerve or the brachial artery, especially when conducting surgical procedures. In the area of the pronator teres, there are many tendons as well. It is important to identify, as much as possible, the correct site of compression. Pathogenesis: The median nerve can get entrapped or compressed by several structures in the arm. The pronator teres muscle is the most common. Others entrapment sites include the flexor digitorum superficialis arch, the lacertus fibrosis (bicipital aponeurosis), and ligament of Struthers (frequency occurs in that order). For compression of the median nerve at the pronator teres and flexor digitorum superficialis, the cause is almost always due to hypertrophy of the respected muscle. This hypertrophy is from quick, forceful and repeated movements to the involved muscle. Examples include a carpenter or a baseball batter. As the muscle hypertrophies, the signal from the median nerve is diminished resulting in paresthesias in the median nerve distribution (lateral arm and hand) distal to the site of compression. Pain in the volar part of the forearm, often aggravated by repetitive supination and pronation, is a common symptom of pronator involvement. Another indicator is forearm pain with the compression of muscle such as pain in the volar part of the forearm implicating pronator teres. Onset is typically insidious and diagnosis is usually delayed 9 months to 2 years. Epidemiology: Pronator teres syndrome is the second most common cause of median nerve compression behind carpal tunnel syndrome. -

Fundamental Shoulder Exercises
FUNDAMENTAL SHOULDER EXERCISES RANGE OF MOTION EXERCISES 1. L-BAR FLEXION Lie on back and grip L-Bar between index finger and thumb, elbows straight. Raise both arms overhead as far as possible keeping thumbs up. Hold for _____ seconds and repeat _____ times. 2. L-BAR EXTERNAL ROTATION, SCAPULAR PLANE Lie on back with involved arm 450 from body and elbow bent at 900. Grip L-Bar in the hand of involved arm and keep elbow in flexed position. Using unin- volved arm, push involved arm into external rotation. Hold for _____ seconds, return to starting position. Repeat _____ times. 3. L-BAR INTERNAL ROTATION, SCAPULAR PLANE Lie on back with involved arm 450 from body and elbow bent at 900. Grip L-Bar in the hand of involved arm and keep elbow in flexed position. Using the uninvolved arm, push involved arm into internal rotation. Hold for _____ seconds, return to starting position. Repeat _____ times. Dr. Meisterling (800) 423-1088 1 of 2 STRENGTHENING EXERCISES 1. TUBING, EXTERNAL ROTATION Standing with involved elbow fixed at side, elbow bent to 900 and involved arm across the front of the body. Grip tubing handle while the other end of tubing is fixed. Pull out with arm, keeping elbow at side. Return tubing slowly and controlled. Perform _____ sets of _____ reps. 2. TUBING, INTERNAL ROTATION Standing with elbow at side fixed at 900 and shoulder rotated out. Grip tubing handle while other end of tubing is fixed. Pull arm across body keeping elbow at side. Return tubing slowly and controlled. -

Early Passive Motion After Surgery
www.western -ortho.com www.denvershoulder.com Early Passive Motion after Shoulder Surgery Passive motion involves someone else moving the affected arm through the motion described. Or, in the case of elbow flexion/extension, you can use your opposite (non-affected arm) to move through the motion. Do 5 repetitions of each stretch 3 times per day. When you feel a slight ‘tightness’ with your arm in the position diagrammed, hold that position for 30 seconds. If lying down is difficult, the stretches can be done while seated. Shoulder Flexion Support arm at the wrist and elbow. With the thumb pointed forward, gently bring the arm up and forward then back to the side. Shoulder Abduction Support arm at wrist and elbow. With the thumb pointed away from the body and palm up, gently bring the arm out to the side. www.western -ortho.com www.denvershoulder.com Shoulder Internal/External Rotation Support arm at wrist and elbow. With the elbow at the side and bent to a 90 degree angle, gently rotate the hand away from the body down toward the table the individual is lying on. Elbow Flexion/Extension Forearm Pronation/Supination Grasp the wrist of your affected arm with your unaffected With your elbow and forearm supported on a table, hand. With your affected elbow against your side and your gently turn forearm so your palm is down, then turn palm up, gently bend and straighten your elbow. forearm so your palm is up. This can be done actively (without assistance from your other hand). . -

Pronator Syndrome: Clinical and Electrophysiological Features in Seven Cases
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.39.5.461 on 1 May 1976. Downloaded from Journal ofNeurology, Neurosurgery, and Psychiatry, 1976, 39, 461-464 Pronator syndrome: clinical and electrophysiological features in seven cases HAROLD H. MORRIS AND BRUCE H. PETERS From the Department ofNeurology, University of Texas Medical Branch, Galveston, Texas, USA SYNOPSIS The clinical and electrophysiological picture of seven patients with the pronator syndrome is contrasted with other causes ofmedian nerve neuropathy. In general, these patients have tenderness over the pronator teres and weakness of flexor pollicis longus as well as abductor pollicis brevis. Conduction velocity of the median nerve in the proximal forearm is usually slow but the distal latency and sensory nerve action potential at the wrist are normal. Injection of corticosteroids into the pronator teres has produced relief of symptoms in a majority of patients. Protected by copyright. In the majority of isolated median nerve dys- period 101 cases of the carpal tunnel syndrome functions the carpal tunnel syndrome is appropri- and the seven cases of the pronator syndrome ately first suspected. The median nerve can also reported here were identified. Median nerve be entrapped in the forearm giving rise to a conduction velocity determinations were made on similar picture and an erroneous diagnosis. all of these patients. The purpose of this report is to draw full attention to the pronator syndrome and to the REPORT OF CASES features which allow it to be distinguished from Table 1 provides clinical details of seven cases of the median nerve entrapment at other sites. -
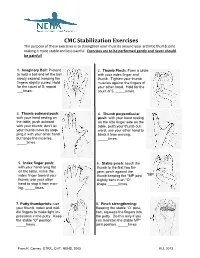
CMC Stabilization Exercises the Purpose of These Exercises Is to Strengthen Your Muscles Around Your Arthritic Thumb Joint Making It More Stable and Less Painful
CMC Stabilization Exercises The purpose of these exercises is to strengthen your muscles around your arthritic thumb joint making it more stable and less painful. Exercises are to be performed gently and never should be painful! 1. Imaginary Ball: Pretend 2. Thumb Pinch: Form a circle to hold a ball and let the ball with your index finger and slowly expand, keeping the thumb. Tighten your thumb fingers slightly curled. Hold muscles against the fingers of for the count of 5, repeat your other hand. Hold for the ___times. count of 5, _____times. 3. Thumb outward push: 4. Thumb perpendicular with your hand resting on push: with your hand resting the table, push outward on the little finger side on the with your thumb; don’t let table, push your thumb out- your thumb move by stop- ward; use your other hand to ping it with your other hand block it from moving. but tense the muscles. _____times. _____times. 5. Index finger push: 6. Stable pinch: touch the with your hand lying flat thumb to the first two fin- on the table, move the gers; pinch against the index finger toward your thumb keeping the *MP joint *MP thumb; use your other slightly bent in an “O” hand to stop it from mov- shape. _____times. ing. _____times. 7. Putty thumbprints: use 8. Pinch strengthening: your thumb, index and mid- Keeping the stable “O” posi- dle fingers to make light im- tion, squeeze the fingers into pressions in the putty. Keep the putty. Do this only if you the stable “O” position. -

Post-Operative Instructions for Flexor Tendon Repair Purpose of Surgery
Post-Operative Instructions for Flexor Tendon Repair Purpose of surgery The goal of the operation is to repair or reattach lacerated or detached flexor tendons. The flexor tendons (muscles) are responsible for flexing (bending) your fingers. What to expect after surgery? You will have a firm splint covering your forearm and the back of your hand and fingers holding your fingers flexed (bent). All your fingers will be included in the splint for any finger flexor tendon repair; and, only your thumb will be included in the splint for a thumb flexor tendon repair. You will be able to see the tips of your fingers/thumb to insure they are getting good circulation. The palm side of your fingers/thumb will be protected by a soft padding that they will be resting on while the plaster will keep your fingers bent from the nail side. You may have some numbness or tingling of fingers/thumb due to the local anesthetic injections used to help control post-operative pain (this should wear off within about 24 hours). After this first 24 hours, you may still experience some numbness and tingling in parts of the operative finger(s)/thumb if you also had a nerve repair. What should you do to help recover? While we do not anticipate significant swelling following this procedure, it would be helpful to keep your hand/wrist elevated as best you can for the first 24 hours after surgery. The thickness of the dressing will prevent the effective placement of a cold-pack. Please do not move your fingers, even if they were not operated on. -

Self Range of Motion Exercises for Arm and Hand
Self-Range of Motion Exercises for the Arm and Hand After a stroke, it is important to do the exercises in this handout for your affected arm and hand. You can do them on your own by using your unaffected arm and hand. These gentle movements are called “self-range of motion” exercises, and they help to maintain your movement, prevent stiffness, improve blood flow, and increase awareness of your affected arm and hand. Complete the exercises slowly and do not force movements. Stop if you feel pain. If you have any questions or concerns, please contact your Occupational Therapist: _______________________________ Do the exercises in this handout _____ times each day. Page - 1 Self-range of motion exercises for the arm and hand 1. Shoulder: Forward Arm Lift Interlock your fingers, or hold your wrist. With your elbows straight and thumbs facing the ceiling, lift your arms to shoulder height. Slowly lower your arms to starting position. Hold for ____ seconds. Repeat ____ times. Page - 2 Self-range of motion exercises for the arm and hand 2. Shoulder: “Rock the Baby” Stretch Hold your affected arm by supporting the elbow, forearm and wrist (as if cradling a baby). Slowly move your arms to the side, away from your body, lifting to shoulder height. Repeat this motion in the other direction. Slowly rock your arms side-to-side, and keep your body from turning. Repeat ____ times. Page - 3 Self-range of motion exercises for the arm and hand 3. Shoulder: Rotation Stretch Interlock your fingers, or hold your wrist. With your elbows bent at 90 degrees, keep your affected arm at your side. -

Morphological Study of Palmaris Longus Muscle
International INTERNATIONAL ARCHIVES OF MEDICINE 2017 Medical Society SECTION: HUMAN ANATOMY Vol. 10 No. 215 http://imedicalsociety.org ISSN: 1755-7682 doi: 10.3823/2485 Humberto Ferreira Morphological Study of Palmaris Arquez1 Longus Muscle ORIGINAL 1 University of Cartagena. University St. Thomas. Professor Human Morphology, Medicine Program, University of Pamplona. Morphology Laboratory Abstract Coordinator, University of Pamplona. Background: The palmaris longus is one of the most variable muscle Contact information: in the human body, this variations are important not only for the ana- tomist but also radiologist, orthopaedic, plastic surgeons, clinicians, Humberto Ferreira Arquez. therapists. In view of this significance is performed this study with Address: University Campus. Kilometer the purpose to determine the morphological variations of palmaris 1. Via Bucaramanga. Norte de Santander, longus muscle. Colombia. Suramérica. Tel: 75685667-3124379606. Methods and Findings: A total of 17 cadavers with different age groups were used for this study. The upper limbs region (34 [email protected] sides) were dissected carefully and photographed in the Morphology Laboratory at the University of Pamplona. Of the 34 limbs studied, 30 showed normal morphology of the palmaris longus muscle (PL) (88.2%); PL was absent in 3 subjects (8.85% of all examined fo- rearm). Unilateral absence was found in 1 male subject (2.95% of all examined forearm); bilateral agenesis was found in 2 female subjects (5.9% of all examined forearm). Duplicated palmaris longus muscle was found in 1 male subject (2.95 % of all examined forearm). The palmaris longus muscle was innervated by branches of the median nerve. The accessory palmaris longus muscle was supplied by the deep branch of the ulnar nerve. -

Laparoscopic Sacralcolpopexy and Enterocele Repair with Mesh
124 State of the Art Atlas and Textbook of Laparoscopic Suturing INTRODUCTION The anatomy, pathophysiology, and treatment of pelvic organ prolapse has significantly evolved over the last decade with increasing understanding of anatomy and development of minimally invasive surgical procedures. Although support for the pelvic viscera, the vagina, and neighboring structures involves a complex interplay between muscles, fascia, nerve supply, and appropriate anatomic orientation, the endopelvic fascia and pelvic floor muscles provide most of the support function in the female pelvis. Laparoscopic reconstructive pelvic surgery requires a thorough knowledge of pelvic floor anatomy and its supportive components before repair of defective anatomy is attempted. This chapter reviews the Fig. 13.1: Level 1 (apical suspension) and level 2 (lateral anatomy and laparoscopic repair of vaginal vault attachment). Level 1—paracolpium suspends the vagina apex prolapse and enterocele with Y-mesh sacralcolpopexy. from the lateral pelvic sidewall via the uterosacral-cardinal complex. Level 2—the anterior vaginal wall is attached laterally ANATOMY OF PELVIC SUPPORT to arcus tendinous fascia pelvis and the posterior vaginal wall is attached laterally to the fascia overlying the levator ani Endopelvic Fascia muscle To understand the pelvic support system of the female pelvic organs, it is useful to subdivide the third of the vagina to the bony sacrum. This complex pelvic support system into three axes: can be described as two separate entities: the cardinal 1. The upper vertical axis ligament and the uterosacral ligament. The cardinal 2. The midhorizontal axis ligament is a fascial sheath of collagen that envelops 3. The lower vertical axis. the internal iliac vessels and then continues along The endopelvic fascia—a network of connective the uterine artery, merging into the visceral capsule tissue and smooth muscle—constitutes the physical of the cervix, lower uterine segment and upper matrix which envelops the pelvic viscera and main- vagina. -

Upper Extremity Extensor Tendon Repair Protocol
Department of Rehabilitation Services Primary Upper Extremity and Hand Extensor Tendon Repair Protocol This protocol is not intended to be a substitute for one’s clinical decision making regarding the progression of a patient’s post-operative course based on their physical exam/findings, individual progress, and/or the presence of post-operative complications. If a clinician requires assistance in the progression of a patient, they should consult with the referring surgeon. The time frames of phases I-IV are examples and can be adjusted based on the given procedure. Progression to the next phase based on the clinical criteria and/or time frames, as appropriate. MALLET FINGER: ZONE I: Over the distal phalangeal joint (DIP)-Mallet deformity ZONE II: Over the middle phalanx/triangular ligament Goal: Protect extensor zone I and II with DIP held in extension with PIP joint free. Photo: Wikem.org/w/index.php?title Precautions: During orthotic/cast check out, keep DIP joints fully extended 100%. Frequency: one to two times/week for 6 to 10 weeks if needed for orthosis/cast checks. Primary Extensor Tendon Repair Protocol Copyright © 2020 The Brigham and Women's Hospital, Inc., Department of Rehabilitation Services. All rights reserved 1 PHASE ORTHOTIC THERAPEUTIC EXERCISE: CONSIDERATIONS: ongoing treatment is variable. Phase I immediate phase: Orthosis or circumferential cast Active PIP flexion of affected Patient to perform daily skin day 1 to 6 to 8 weeks. finger with adjacent finger(s) held check while keeping DIP Non-op: DIP 10°-0 in extension. extended. hyperextension for tendinous mallet 6-8 weeks. Consider taping DIP in extension. -

De Quervain's Tenosynovitis
PATIENT & CAREGIVER EDUCATION De Quervain's Tenosynovitis This information explains the causes, symptoms, and treatment of de Quervain’s tenosynovitis (da-cur-vains teno-sin-o-vitis). De Quervain’s tenosynovitis is a common and painful condition that affects the tendons (tissue that connects muscles to bones) of the wrist. A tendon sheath (protective covering) wraps around these tendons so that they can slide easily (see Figure 1). This allows you to turn your wrist, grip, and pinch with your hand. With de Quervain’s tenosynovitis, the tendon sheath becomes swollen. This causes pain and limited movement in your wrist and thumb. Figure 1. Wrist with De Quervain’s tenosynovitis Causes of De Quervain’s Tenosynovitis Some causes of de Quervain’s tenosynovitis include: Overusing your wrist with repetitive movements, such as: Typing Knitting De Quervain's Tenosynovitis 1/4 Using a hammer Holding an infant for a long time Carrying heavy grocery bags Strain or injury to the wrist area. Conditions that cause swelling throughout the body, such as rheumatoid arthritis. Symptoms of De Quervain’s Tenosynovitis De Quervain’s tenosynovitis can cause different symptoms, such as: Pain at the side of your wrist under the base of your thumb. Moving your thumb can increase this pain. Wrist pain that has spread into your forearm and thumb. Mild swelling, redness, or warmth at your wrist. A fluid-filled cyst near the thumb side of your wrist. Your doctor can see if you have de Quervain’s tenosynovitis based on your symptoms and a physical exam. They will also ask you to do certain movements with your hand, wrist, and thumb. -

Muscles of the Upper Limb.Pdf
11/8/2012 Muscles Stabilizing Pectoral Girdle Muscles of the Upper Limb Pectoralis minor ORIGIN: INNERVATION: anterior surface of pectoral nerves ribs 3 – 5 ACTION: INSERTION: protracts / depresses scapula coracoid process (scapula) (Anterior view) Muscles Stabilizing Pectoral Girdle Muscles Stabilizing Pectoral Girdle Serratus anterior Subclavius ORIGIN: INNERVATION: ORIGIN: INNERVATION: ribs 1 - 8 long thoracic nerve rib 1 ---------------- INSERTION: ACTION: INSERTION: ACTION: medial border of scapula rotates scapula laterally inferior surface of scapula stabilizes / depresses pectoral girdle (Lateral view) (anterior view) Muscles Stabilizing Pectoral Girdle Muscles Stabilizing Pectoral Girdle Trapezius Levator scapulae ORIGIN: INNERVATION: ORIGIN: INNERVATION: occipital bone / spinous accessory nerve transverse processes of C1 – C4 dorsal scapular nerve processes of C7 – T12 ACTION: INSERTION: ACTION: INSERTION: stabilizes / elevates / retracts / upper medial border of scapula elevates / adducts scapula acromion / spine of scapula; rotates scapula lateral third of clavicle (Posterior view) (Posterior view) 1 11/8/2012 Muscles Stabilizing Pectoral Girdle Muscles Moving Arm Rhomboids Pectoralis major (major / minor) ORIGIN: INNERVATION: ORIGIN: INNERVATION: spinous processes of C7 – T5 dorsal scapular nerve sternum / clavicle / ribs 1 – 6 dorsal scapular nerve INSERTION: ACTION: INSERTION: ACTION: medial border of scapula adducts / rotates scapula intertubucular sulcus / greater tubercle flexes / medially rotates / (humerus) adducts