The Cognitive Impairment Study (CARES) Trial 1
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Episodic Memory in Transient Global Amnesia: Encoding, Storage, Or Retrieval Deficit?
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.66.2.148 on 1 February 1999. Downloaded from 148 J Neurol Neurosurg Psychiatry 1999;66:148–154 Episodic memory in transient global amnesia: encoding, storage, or retrieval deficit? Francis Eustache, Béatrice Desgranges, Peggy Laville, Bérengère Guillery, Catherine Lalevée, Stéphane SchaeVer, Vincent de la Sayette, Serge Iglesias, Jean-Claude Baron, Fausto Viader Abstract evertheless this division into processing stages Objectives—To assess episodic memory continues to be useful in helping understand (especially anterograde amnesia) during the working of memory systems”. These three the acute phase of transient global amne- stages may be defined in the following way: (1) sia to diVerentiate an encoding, a storage, encoding, during which perceptive information or a retrieval deficit. is transformed into more or less stable mental Methods—In three patients, whose am- representations; (2) storage (or consolidation), nestic episode fulfilled all current criteria during which mnemonic information is associ- for transient global amnesia, a neuro- ated with other representations and maintained psychological protocol was administered in long term memory; (3) retrieval, during which included a word learning task which the subject can momentarily reactivate derived from the Grober and Buschke’s mnemonic representations. These definitions procedure. will be used in the present study. Results—In one patient, the results sug- Regarding the retrograde amnesia of TGA, it gested an encoding deficit, -
Mnemonics in a Mnutshell: 32 Aids to Psychiatric Diagnosis
Mnemonics in a mnutshell: 32 aids to psychiatric diagnosis Clever, irreverent, or amusing, a mnemonic you remember is a lifelong learning tool ® Dowden Health Media rom SIG: E CAPS to CAGE and WWHHHHIMPS, mnemonics help practitioners and trainees recall Fimportant lists (suchCopyright as criteriaFor for depression,personal use only screening questions for alcoholism, or life-threatening causes of delirium, respectively). Mnemonics’ effi cacy rests on the principle that grouped information is easi- er to remember than individual points of data. Not everyone loves mnemonics, but recollecting diagnostic criteria is useful in clinical practice and research, on board examinations, and for insurance reimbursement. Thus, tools that assist in recalling di- agnostic criteria have a role in psychiatric practice and IMAGES teaching. JUPITER In this article, we present 32 mnemonics to help cli- © nicians diagnose: • affective disorders (Box 1, page 28)1,2 Jason P. Caplan, MD Assistant clinical professor of psychiatry • anxiety disorders (Box 2, page 29)3-6 Creighton University School of Medicine 7,8 • medication adverse effects (Box 3, page 29) Omaha, NE • personality disorders (Box 4, page 30)9-11 Chief of psychiatry • addiction disorders (Box 5, page 32)12,13 St. Joseph’s Hospital and Medical Center Phoenix, AZ • causes of delirium (Box 6, page 32).14 We also discuss how mnemonics improve one’s Theodore A. Stern, MD Professor of psychiatry memory, based on the principles of learning theory. Harvard Medical School Chief, psychiatric consultation service Massachusetts General Hospital How mnemonics work Boston, MA A mnemonic—from the Greek word “mnemonikos” (“of memory”)—links new data with previously learned information. -

Memory Reconsolidation
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Current Biology Vol 23 No 17 R746 emerged from the pattern of amnesia consequence of this dynamic process Memory collectively caused by all these is that established memories, which reconsolidation different types of interventions. have reached a level of stability, can be Memory consolidation appeared to bidirectionally modulated and modified: be a complex and quite prolonged they can be weakened, disrupted Cristina M. Alberini1 process, during which different types or enhanced, and be associated and Joseph E. LeDoux1,2 of amnestic manipulation were shown to parallel memory traces. These to disrupt different mechanisms in the possibilities for trace strengthening The formation, storage and use of series of changes occurring throughout or weakening, and also for qualitative memories is critical for normal adaptive the consolidation process. The initial modifications via retrieval and functioning, including the execution phase of consolidation is known to reconsolidation, have important of goal-directed behavior, thinking, require a number of regulated steps behavioral and clinical implications. problem solving and decision-making, of post-translational, translational and They offer opportunities for finding and is at the center of a variety of gene expression mechanisms, and strategies that could change learning cognitive, addictive, mood, anxiety, blockade of any of these can impede and memory to make it more efficient and developmental disorders. Memory the entire consolidation process. and adaptive, to prevent or rescue also significantly contributes to the A century of studies on memory memory impairments, and to help shaping of human personality and consolidation proposed that, despite treat diseases linked to abnormally character, and to social interactions. -

The Effects of Happy and Sad Emotional States on Episodic Memory
The Effects of Happy and Sad Emotional States on Episodic Memory Richard Topolski ([email protected]) Department of Psychology, Augusta State University 2500 Walton Way, Augusta GA 30904 USA Sarah R. Daniel ([email protected]) Department of Psychology, Augusta State University 2500 Walton Way, Augusta GA 30904 USA Introduction methodology for measuring EM largely independent of semantic memory. Episodic memory (EM) is composed of personally experienced events in which ‘the what, where, and when’ Method are essential components while semantic memory is simply composed of accumulated facts about the world (Tulving, Happy, neutral, or sad mood states were induced in 88 2002). A wide variety of tasks have been used to tap students via a 20 minute long viewing of either a stand-up episodic memory including: recalling words from an early comedy routine, a documentary, or holocaust footage. learned list; yes-no recognition of previously presented Immediately following the mood induction, participants common objects or pictures; and free recall of past personal engaged in eight interactive tasks which involved both experiences. These tasks are used to evaluate episodic familiar objects (pennies and paperclips) and novel memory because in order to know which words, pictures, or geometric forms created by bending paper clips with blue experiences to retrieve, some contextual (episodic) beads into unique shapes, (Rock, Schreilber, and Ro, 1994). information must first be accessed (Mayes & Roberts, A four-item force-choice recognition test for the novel 2001). While all of these measures seem to share this geometric forms was employed, with the task name serving contextual component, none adequately examines the as the retrieval cue. -
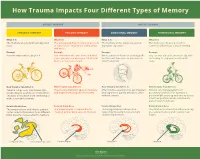
How Trauma Impacts Four Different Types of Memory
How Trauma Impacts Four Different Types of Memory EXPLICIT MEMORY IMPLICIT MEMORY SEMANTIC MEMORY EPISODIC MEMORY EMOTIONAL MEMORY PROCEDURAL MEMORY What It Is What It Is What It Is What It Is The memory of general knowledge and The autobiographical memory of an event The memory of the emotions you felt The memory of how to perform a facts. or experience – including the who, what, during an experience. common task without actively thinking and where. Example Example Example Example You remember what a bicycle is. You remember who was there and what When a wave of shame or anxiety grabs You can ride a bicycle automatically, with- street you were on when you fell off your you the next time you see your bicycle out having to stop and recall how it’s bicycle in front of a crowd. after the big fall. done. How Trauma Can Affect It How Trauma Can Affect It How Trauma Can Affect It How Trauma Can Affect It Trauma can prevent information (like Trauma can shutdown episodic memory After trauma, a person may get triggered Trauma can change patterns of words, images, sounds, etc.) from differ- and fragment the sequence of events. and experience painful emotions, often procedural memory. For example, a ent parts of the brain from combining to without context. person might tense up and unconsciously make a semantic memory. alter their posture, which could lead to pain or even numbness. Related Brain Area Related Brain Area Related Brain Area Related Brain Area The temporal lobe and inferior parietal The hippocampus is responsible for The amygdala plays a key role in The striatum is associated with producing cortex collect information from different creating and recalling episodic memory. -

Episodic Memory-From Brain to Mind
HIPPOCAMPUS 16:691–703 (2006) Episodic Memory—From Brain to Mind Janina Ferbinteanu,* Pamela J. Kennedy, and Matthew L. Shapiro ABSTRACT: Neuronal mechanisms of episodic memory, the conscious by the rapid formation of relational representations of recollection of autobiographical events, are largely unknown because highly processed sensory information that are used electrophysiological studies in humans are conducted only in excep- tional circumstances. Unit recording studies in animals are thus crucial flexibly and are not necessarily expressed through overt for understanding the neurophysiological substrate that enables people motor behavior. Episodic memory is also sensitive to to remember their individual past. Two features of episodic memory— lesions of the prefrontal cortex (Wheeler et al., 1995; autonoetic consciousness, the self-aware ability to \travel through Nyberg et al., 2000; Burgess et al., 2002; Wheeler time", and one-trial learning, the acquisition of information in one and Stuss, 2003), develops later in an individual’s life, occurrence of the event—raise important questions about the validity of animal models and the ability of unit recording studies to capture essen- encodes events within a personal framework, and pos- tial aspects of memory for episodes. We argue that autonoetic experi- sesses a temporal dimension because it is oriented ence is a feature of human consciousness rather than an obligatory as- towards the past and the future (Tulving, 1972, 2001, pect of memory for episodes, and that episodic memory is reconstruc- 2002; Tulving and Markowitsch, 1998). Autobio- tive and thus its key features can be modeled in animal behavioral tasks graphic information contains memories about what that do not involve either autonoetic consciousness or one-trial learning. -

Cognitive Functions of the Brain: Perception, Attention and Memory
IFM LAB TUTORIAL SERIES # 6, COPYRIGHT c IFM LAB Cognitive Functions of the Brain: Perception, Attention and Memory Jiawei Zhang [email protected] Founder and Director Information Fusion and Mining Laboratory (First Version: May 2019; Revision: May 2019.) Abstract This is a follow-up tutorial article of [17] and [16], in this paper, we will introduce several important cognitive functions of the brain. Brain cognitive functions are the mental processes that allow us to receive, select, store, transform, develop, and recover information that we've received from external stimuli. This process allows us to understand and to relate to the world more effectively. Cognitive functions are brain-based skills we need to carry out any task from the simplest to the most complex. They are related with the mechanisms of how we learn, remember, problem-solve, and pay attention, etc. To be more specific, in this paper, we will talk about the perception, attention and memory functions of the human brain. Several other brain cognitive functions, e.g., arousal, decision making, natural language, motor coordination, planning, problem solving and thinking, will be added to this paper in the later versions, respectively. Many of the materials used in this paper are from wikipedia and several other neuroscience introductory articles, which will be properly cited in this paper. This is the last of the three tutorial articles about the brain. The readers are suggested to read this paper after the previous two tutorial articles on brain structure and functions [17] as well as the brain basic neural units [16]. Keywords: The Brain; Cognitive Function; Consciousness; Attention; Learning; Memory Contents 1 Introduction 2 2 Perception 3 2.1 Detailed Process of Perception . -

Test Anxiety and Metamemory: General Preference for External Over Internal Information Storage
Personality and Individual Differences 30 (2001) 775±781 www.elsevier.com/locate/paid Test anxiety and metamemory: general preference for external over internal information storage Joachim StoÈ ber *, Klaus B. Esser Free University of Berlin, Habelschwerdter Allee 45, D-14195 Berlin, Germany Received 27 October 1999; received in revised form 22 February 2000 Abstract Substantial evidence suggests that test anxiety is associated with poor memory performance. The rela- tionship between test anxiety and metamemory, however, has remained largely unexplored. The present study examines test anxiety and metamemory from the perspective of storage selection in extended memory systems. A sample of 56 university students with scores in the upper or lower thirds of the distribution for the Test Anxiety Inventory were presented with sentences describing everyday tasks under conditions where low and high importance was attached to future remembering. For each sentence, participants indicated whether they would choose internal memory storage (neurophysiological memory) or external storage (external memory aids) to remember the information. Results showed that test-anxious partici- pants displayed a general preference for external over internal storage, independent of the importance attached to remembering. Low estimated success of internal storage emerged as a potential reason for this preference. Implications of these ®ndings for research on test anxiety, metamemory, and storage selection in extended memory systems are discussed. # 2001 Elsevier Science Ltd. All rights reserved. Keywords: Test anxiety; Memory; Memory aids; Metacognition 1. Introduction Substantial evidence accumulated over the last 25 years suggests that test anxiety is associated with poor memory performance (for reviews, see Eysenck, 1979; Mueller, 1992; Zeidner, 1998). -

Episodic Memory, Semantic Memory and the Epistemic Asymmetry
1 Remembering past experiences: episodic memory, semantic memory and the epistemic asymmetry Christoph Hoerl forthcoming in K. Michaelian, D. Debus & D. Perrin (eds.): New Directions in the Philosophy of Memory. Routledge. There seems to be a distinctive way in which we can remember events we have experienced ourselves, which differs from the capacity to retain information about events that we can also have when we have not experienced those events ourselves but just learned about them in some other way. Psychologists and increasingly also philosophers have tried to capture this difference in terms of the idea of two different types of memory: episodic memory and semantic memory. Yet, the demarcation between episodic memory and semantic memory remains a contested topic in both disciplines, to the point of there being researchers in each of them who question the usefulness of the distinction between the two concepts.1 In this paper, I outline a new characterization of the difference between episodic memory and semantic memory, which connects that difference to what is sometimes called the ‘epistemic asymmetry’ between the past and the future, or the ‘epistemic arrow’ of time. My proposal will be that episodic memory and semantic memory exemplify the epistemic asymmetry in two different ways, and for somewhat different reasons, and that the way in which 1 The episodic/semantic distinction originates with Tulving (1972), and has been refined by Tulving in a number of other works (Tulving, 1985, 2002; Wheeler, Stuss, & Tulving, 1997). Rival ways of carving up the domain of memories are suggested, for instance, in Bernecker (2010) and Rubin and Umanath (2015). -
How Can I Remember That the Memory Workshop
Tips and Strategies to Help Improve Your Short- and Long-Term Memory Karen L. Wold, M.S.Ed. Learning Disabilities Specialist [email protected], 217-333-8705 Topics Covered Memory 101 – Different Types of Memory Defined The memory process Short-term memory (STM) Working memory Long-term memory (LTM) Memory Strategies Rote memory (Repetition) Mnemonics Associative memory (Making associations) Memory Compensations (Alternatives, “Work Arounds”) Using reasoning skills to compensate Keep in mind learning styles/strengths (visual, auditory, kinesthetic, tactile) and effects of disability on memory Resources for More Information Memory 101: Different Types of Memory Memory process = encoding+ storage (sensory, STM, LTM) + retrieval Encoding – taking information from our environment (very short term, not retained over the long term) Sensory storage – information we receive from our senses is interpreted by our brains, then only the information that we really pay attention to is transferred to STM Learning allows us to transfer information from our STM to our LTM Retrieval is the ability to recall information we have learned and memoriZed Short-term Memory Information that comes to us through our senses Can only “hold” or retain for a few seconds Can only “hold” or retain a limited amount of information (before other information “kicks it out”) Can only hold 5-9 bits of info (avg. of 7) at one time Example: phone number or name. Usually have to write it down to remember later. Reflection Question: Why is it so hard to remember the name of someone you just met? Working Memory Working memory involves manipulating or changing information that is in your memory For example, “mental math”, adding 123 + 45 in your head. -

Interactions Between Attention and Memory Marvin M Chun and Nicholas B Turk-Browne
Interactions between attention and memory Marvin M Chun and Nicholas B Turk-Browne Attention and memory cannot operate without each other. In form of selective attention to internal representations this review, we discuss two lines of recent evidence that [1,2]. support this interdependence. First, memory has a limited capacity, and thus attention determines what will be Classic psychologists such as William James stated long encoded. Division of attention during encoding prevents the ago that ‘we cannot deny that an object once attended to formation of conscious memories, although the role of attention will remain in the memory, while one inattentively in formation of unconscious memories is more complex. Such allowed to pass will leave no traces behind’ [3]. More memories can be encoded even when there is another recently, leading neuroscientists such as Eric Kandel have concurrent task, but the stimuli that are to be encoded must be stated that one of the most important problems for 21st selected from among other competing stimuli. Second, century neuroscience is to understand how attention memory from past experience guides what should be attended. regulates the processes that stabilize experiential mem- Brain areas that are important for memory, such as the ories [4]. Here, we review studies from the past two years hippocampus and medial temporal lobe structures, are that reveal progress towards understanding the inter- recruited in attention tasks, and memory directly affects frontal- actions between attention and memory in neural systems. parietal networks involved in spatial orienting. Thus, exploring the interactions between attention and memory can provide Attention at encoding new insights into these fundamental topics of cognitive A major question in many people’s minds is how to neuroscience. -

Korsakoff's Syndrome
NEUROPSYCHOLOGY AND NEUROIMAGING OF ALCOHOL USE DISORDER WITH AND WITHOUT KORSAKOFF’S SYNDROME: A BETTER UNDERSTANDING FOR A BETTER TREATMENT Anne Lise PITEL CONFLICT OF INTEREST No conflict of interest to declare. ALCOHOL USE DISORDER (AUD): EPIDEMIOLOGY 10% of French population with disastrous health, psychological, social and professional consequences (Rehm et al. 2011). Alcohol is the cause of 49 000 deaths per year and 18% of the premature deaths in the 35-64 year-old people in France (Guerin et al. 2013). 17% of the admissions in the emergency department in France. Worldwide, alcohol is the third risk factor for morbidity after high blood pressure and tobacco (Moller 2013). Alcohol is the cause of more than 60 diseases (dependence, cirrhosis, psychosis, fetal alcohol syndrome, …) (World Health Organization 2014). Alcohol contributes to the development of more than 200 diseases (cancer, heart disease, pancreatitis, liver disease, …) (Moller 2013). The life expectancy is reduced of 20 years in a man with alcohol dependence (John et al. 2013). The cost related to alcohol or tobacco use disorders is 349 billion euros for Europe, knowing that it is 105 for dementia and 64 for strokes (Effertz et Mann 2013). Tremendous social cost: first cause of hospital admission, sick leave and premature death. ALCOHOL USE DISORDER (AUD): DSM-5 CRITERIA Changes in the concepts: Alcoholism Alcohol dependence (DSM IV) Alcohol Use Disorder (DSM V) A problem pattern of alcohol use, leading to clinically significant impairment or distress, manifested by 2 or more of the following in a 12-month period: . Alcohol drunk in larger amounts or for longer time .