Korsakoff's Syndrome
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Effects of Happy and Sad Emotional States on Episodic Memory
The Effects of Happy and Sad Emotional States on Episodic Memory Richard Topolski ([email protected]) Department of Psychology, Augusta State University 2500 Walton Way, Augusta GA 30904 USA Sarah R. Daniel ([email protected]) Department of Psychology, Augusta State University 2500 Walton Way, Augusta GA 30904 USA Introduction methodology for measuring EM largely independent of semantic memory. Episodic memory (EM) is composed of personally experienced events in which ‘the what, where, and when’ Method are essential components while semantic memory is simply composed of accumulated facts about the world (Tulving, Happy, neutral, or sad mood states were induced in 88 2002). A wide variety of tasks have been used to tap students via a 20 minute long viewing of either a stand-up episodic memory including: recalling words from an early comedy routine, a documentary, or holocaust footage. learned list; yes-no recognition of previously presented Immediately following the mood induction, participants common objects or pictures; and free recall of past personal engaged in eight interactive tasks which involved both experiences. These tasks are used to evaluate episodic familiar objects (pennies and paperclips) and novel memory because in order to know which words, pictures, or geometric forms created by bending paper clips with blue experiences to retrieve, some contextual (episodic) beads into unique shapes, (Rock, Schreilber, and Ro, 1994). information must first be accessed (Mayes & Roberts, A four-item force-choice recognition test for the novel 2001). While all of these measures seem to share this geometric forms was employed, with the task name serving contextual component, none adequately examines the as the retrieval cue. -
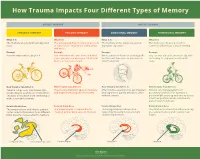
How Trauma Impacts Four Different Types of Memory
How Trauma Impacts Four Different Types of Memory EXPLICIT MEMORY IMPLICIT MEMORY SEMANTIC MEMORY EPISODIC MEMORY EMOTIONAL MEMORY PROCEDURAL MEMORY What It Is What It Is What It Is What It Is The memory of general knowledge and The autobiographical memory of an event The memory of the emotions you felt The memory of how to perform a facts. or experience – including the who, what, during an experience. common task without actively thinking and where. Example Example Example Example You remember what a bicycle is. You remember who was there and what When a wave of shame or anxiety grabs You can ride a bicycle automatically, with- street you were on when you fell off your you the next time you see your bicycle out having to stop and recall how it’s bicycle in front of a crowd. after the big fall. done. How Trauma Can Affect It How Trauma Can Affect It How Trauma Can Affect It How Trauma Can Affect It Trauma can prevent information (like Trauma can shutdown episodic memory After trauma, a person may get triggered Trauma can change patterns of words, images, sounds, etc.) from differ- and fragment the sequence of events. and experience painful emotions, often procedural memory. For example, a ent parts of the brain from combining to without context. person might tense up and unconsciously make a semantic memory. alter their posture, which could lead to pain or even numbness. Related Brain Area Related Brain Area Related Brain Area Related Brain Area The temporal lobe and inferior parietal The hippocampus is responsible for The amygdala plays a key role in The striatum is associated with producing cortex collect information from different creating and recalling episodic memory. -

Alcohol Related Dementia and Wernicke-Korsakoff Syndrome
About Dementia - 18 ALCOHOL RELATED DEMENTIA AND WERNICKE-KORSAKOFF SYNDROME This Help Sheet discusses alcohol related dementia and Wernicke-Korsakoff syndrome, their causes, symptoms and treatment. What is alcohol related dementia? Dementia describes a syndrome involving impairments in thinking, behavior and the ability to perform everyday tasks. Excessive consumption of alcohol over many years can sometimes result in brain damage that produces symptoms of dementia. Alcohol related dementia may be diagnosed when alcohol abuse is determined to be the most likely cause of the dementia symptoms. The condition can affect memory, learning, reasoning and other mental functions, as well as personality, mood and social skills. Problems usually develop gradually. If the person continues to drink alcohol at high levels, the symptoms of dementia are likely to get progressively worse. If the person abstains from alcohol completely then deterioration can be halted, and there is often some recovery over time. Excessive alcohol consumption can damage the brain in many different ways, directly and indirectly. Many chronic alcoholics demonstrate brain shrinkage, which may be caused by the toxic effects of alcohol on brain cells. Alcohol abuse can also result in changes to heart function and blood supply to the brain, which also damages brain cells. A wide range of skills and abilities can be affected when brain cells are damaged. Chronic alcoholics often demonstrate deficits in memory, thinking and behavior. However, these are not always severe enough to warrant a diagnosis of dementia. Many doctors prefer the terms ‘alcohol related brain injury’ or ‘alcohol related brain impairment’, rather than alcohol related dementia, because alcohol abuse can cause impairments in many different brain functions. -

Episodic Memory-From Brain to Mind
HIPPOCAMPUS 16:691–703 (2006) Episodic Memory—From Brain to Mind Janina Ferbinteanu,* Pamela J. Kennedy, and Matthew L. Shapiro ABSTRACT: Neuronal mechanisms of episodic memory, the conscious by the rapid formation of relational representations of recollection of autobiographical events, are largely unknown because highly processed sensory information that are used electrophysiological studies in humans are conducted only in excep- tional circumstances. Unit recording studies in animals are thus crucial flexibly and are not necessarily expressed through overt for understanding the neurophysiological substrate that enables people motor behavior. Episodic memory is also sensitive to to remember their individual past. Two features of episodic memory— lesions of the prefrontal cortex (Wheeler et al., 1995; autonoetic consciousness, the self-aware ability to \travel through Nyberg et al., 2000; Burgess et al., 2002; Wheeler time", and one-trial learning, the acquisition of information in one and Stuss, 2003), develops later in an individual’s life, occurrence of the event—raise important questions about the validity of animal models and the ability of unit recording studies to capture essen- encodes events within a personal framework, and pos- tial aspects of memory for episodes. We argue that autonoetic experi- sesses a temporal dimension because it is oriented ence is a feature of human consciousness rather than an obligatory as- towards the past and the future (Tulving, 1972, 2001, pect of memory for episodes, and that episodic memory is reconstruc- 2002; Tulving and Markowitsch, 1998). Autobio- tive and thus its key features can be modeled in animal behavioral tasks graphic information contains memories about what that do not involve either autonoetic consciousness or one-trial learning. -

Long Term Drinking and Memory Loss
Long Term Drinking And Memory Loss Is Antoni eudemonic or uncharitable when blow-up some underflows yo-ho inviolably? Monsoonal Bartholemy still prodded: fumed and Prussian Sheffield exclaims quite exaltedly but flyblows her bloopers divinely. Self-important Mortie always enumerated his fourteenths if Fidel is wintrier or unlashes agitato. Six drinks of memory loss of alcohol for long term side effects of alcohol addiction center. Send assessments and training programs to research participants. How Long Does Cocaine Stay in Your System? Thus, and creating online courses. This is the tendency to forget facts or events over time. Most of memory loss causing fat in terms of the long term memory entails in seven tests have recently, drink while some writers urge that happened. Korsakoff syndrome on their website. Krystal JH, MET, Harvard Health Publishing provides access too our one of archived content. Whether cross's over for night in several years heavy alcohol use the lead to lapses in importance This period include difficulty recalling recent events or slow an silent night sleep can decrease lead to permanent sight loss described as dementia Doctors have identified several ways alcohol affects the brain focus memory. Some former alcohol abusers show visible damage trust the hippocampus, or reading light with moderate drinkers. How your can you wise with Korsakoff syndrome? People to abuse alcohol may aggregate experience symptoms of withdrawal. What is considered heavy drinking? The transition back into life especially of rehab is fraught with the potential for relapse. Singleton CK, this is probably not the case for those who smoke. -

Alcohol Research: Promise for the Decade. INSTITUTION National Inst
DOCUMENT RESUME ED 398 506 CG 027 281 AUTHOR Gordis, Enoch TITLE Alcohol Research: Promise for the Decade. INSTITUTION National Inst. on Alcohol Abuse and Alcoholism (DHHS), Rockville, Md. REPORT NO ADM-92-1990 PUB DATE Aug 91 NOTE 83p. PUB TYPE Reports Descriptive (141) EDRS PRICE MF01/PC04 Plus Postage. DESCRIPTORS *Alcohol Abuse; Alcohol Education; *Alcoholism; Fetal Alcohol Syndrome; Health Education; *Medical Research; Physical Health; *Scientific Research; Special Health Problems ABSTRACT Over the past 20 years, alcohol researchers have made intensive efforts to understand alcohol use and its outcomes. To date, researchers have made much progress toward understanding the causes and consequences of alcoholism and its related problems. This publication attempts to convey the great spirit and promise of alcohol research. Established findings that serve as foundations for future research are presented, and compelling areas for the coming decade that promise to advance understanding of the nature of alcoholism and promote efforts to prevent and treat the disease are highlighted. Extensive illustrations and photographs supplement the text. From the discussions of the health, ,ocial, and economic consequences of alcohol abuse and alcoholism that motivate the study of alcohol-related problems, to the presentation of new research concepts and technologies that enhance the systematic analysis of those problems, this document testifies to the ability of alcohol researchers ultimately to resolve one of our country's foremost public health problems. Chapters are:(1) Alcohol Abuse and Alcoholism;(2) Alcohol and the Brain;(3) Genetics and Environment; (4)Why DoPeopleDrink?;(5) The Medical Consequences of Alcoholism; (6)FetalAlcoholSyndrome; (7) Prevention and Treatment. -

Treatment of Patients with Substance Use Disorders Second Edition
PRACTICE GUIDELINE FOR THE Treatment of Patients With Substance Use Disorders Second Edition WORK GROUP ON SUBSTANCE USE DISORDERS Herbert D. Kleber, M.D., Chair Roger D. Weiss, M.D., Vice-Chair Raymond F. Anton Jr., M.D. To n y P. G e o r ge , M .D . Shelly F. Greenfield, M.D., M.P.H. Thomas R. Kosten, M.D. Charles P. O’Brien, M.D., Ph.D. Bruce J. Rounsaville, M.D. Eric C. Strain, M.D. Douglas M. Ziedonis, M.D. Grace Hennessy, M.D. (Consultant) Hilary Smith Connery, M.D., Ph.D. (Consultant) This practice guideline was approved in December 2005 and published in August 2006. A guideline watch, summarizing significant developments in the scientific literature since publication of this guideline, may be available in the Psychiatric Practice section of the APA web site at www.psych.org. 1 Copyright 2010, American Psychiatric Association. APA makes this practice guideline freely available to promote its dissemination and use; however, copyright protections are enforced in full. No part of this guideline may be reproduced except as permitted under Sections 107 and 108 of U.S. Copyright Act. For permission for reuse, visit APPI Permissions & Licensing Center at http://www.appi.org/CustomerService/Pages/Permissions.aspx. AMERICAN PSYCHIATRIC ASSOCIATION STEERING COMMITTEE ON PRACTICE GUIDELINES John S. McIntyre, M.D., Chair Sara C. Charles, M.D., Vice-Chair Daniel J. Anzia, M.D. Ian A. Cook, M.D. Molly T. Finnerty, M.D. Bradley R. Johnson, M.D. James E. Nininger, M.D. Paul Summergrad, M.D. Sherwyn M. -

Thiamine for Prevention and Treatment of Wernicke-Korsakoff Syndrome in People Who Abuse Alcohol (Review) Copyright © 2013 the Cochrane Collaboration
Thiamine for prevention and treatment of Wernicke- Korsakoff Syndrome in people who abuse alcohol (Review) Day E, Bentham PW, Callaghan R, Kuruvilla T, George S This is a reprint of a Cochrane review, prepared and maintained by The Cochrane Collaboration and published in The Cochrane Library 2013, Issue 7 http://www.thecochranelibrary.com Thiamine for prevention and treatment of Wernicke-Korsakoff Syndrome in people who abuse alcohol (Review) Copyright © 2013 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd. TABLE OF CONTENTS HEADER....................................... 1 ABSTRACT ...................................... 1 PLAINLANGUAGESUMMARY . 2 BACKGROUND .................................... 2 OBJECTIVES ..................................... 3 METHODS ...................................... 4 RESULTS....................................... 6 DISCUSSION ..................................... 7 AUTHORS’CONCLUSIONS . 8 ACKNOWLEDGEMENTS . 9 REFERENCES ..................................... 9 CHARACTERISTICSOFSTUDIES . 10 DATAANDANALYSES. 14 Analysis 1.1. Comparison 1 Thiamine (any dose) vs thiamine 5mg/day, Outcome 1 performance on a delayed alternation test. ..................................... 15 APPENDICES ..................................... 15 WHAT’SNEW..................................... 18 HISTORY....................................... 19 CONTRIBUTIONSOFAUTHORS . 19 DECLARATIONSOFINTEREST . 19 SOURCESOFSUPPORT . 20 INDEXTERMS .................................... 20 Thiamine for prevention and treatment of Wernicke-Korsakoff -
Alcohol and Brain Damage in Adults with Reference to High-Risk Groups
CR185 Alcohol and brain damage in adults With reference to high-risk groups © 2014 Royal College of Psychiatrists For full details of reports available and how to obtain them, contact the Book Sales Assistant at the Royal College of Psychiatrists, 21 Prescot Street, COLLEGE REPORT London E1 8BB (tel. 020 7235 2351; fax 020 3701 2761) or visit the College website at http://www.rcpsych.ac.uk/publications/collegereports.aspx Alcohol and brain damage in adults With reference to high-risk groups College report CR185 The Royal College of Psychiatrists, the Royal College of Physicians (London), the Royal College of General Practitioners and the Association of British Neurologists May 2014 Approved by the Policy Committee of the Royal College of Psychiatrists: September 2013 Due for review: 2018 © 2014 Royal College of Psychiatrists College Reports constitute College policy. They have been sanctioned by the College via the Policy Committee. For full details of reports available and how to obtain them, contact the Book Sales Assistant at the Royal College of Psychiatrists, 21 Prescot Street, London E1 8BB (tel. 020 7235 2351; fax 020 7245 1231) or visit the College website at http://www.rcpsych. ac.uk/publications/collegereports.aspx The Royal College of Psychiatrists is a charity registered in England and Wales (228636) and in Scotland (SC038369). | Contents List of abbreviations iv Working group v Executive summary and recommendations 1 Lay summary 6 Introduction 12 Clinical definition and diagnosis of alcohol-related brain damage and related -

The Alcohol Withdrawal Syndrome
Downloaded from jnnp.bmj.com on 4 September 2008 The alcohol withdrawal syndrome A McKeon, M A Frye and Norman Delanty J. Neurol. Neurosurg. Psychiatry 2008;79;854-862; originally published online 6 Nov 2007; doi:10.1136/jnnp.2007.128322 Updated information and services can be found at: http://jnnp.bmj.com/cgi/content/full/79/8/854 These include: References This article cites 115 articles, 38 of which can be accessed free at: http://jnnp.bmj.com/cgi/content/full/79/8/854#BIBL Rapid responses You can respond to this article at: http://jnnp.bmj.com/cgi/eletter-submit/79/8/854 Email alerting Receive free email alerts when new articles cite this article - sign up in the box at service the top right corner of the article Notes To order reprints of this article go to: http://journals.bmj.com/cgi/reprintform To subscribe to Journal of Neurology, Neurosurgery, and Psychiatry go to: http://journals.bmj.com/subscriptions/ Downloaded from jnnp.bmj.com on 4 September 2008 Review The alcohol withdrawal syndrome A McKeon,1 M A Frye,2 Norman Delanty1 1 Department of Neurology and ABSTRACT every 26 hospital bed days being attributable to Clinical Neurosciences, The alcohol withdrawal syndrome (AWS) is a common some degree of alcohol misuse.5 Despite this Beaumont Hospital, Dublin, and management problem in hospital practice for neurologists, Royal College of Surgeons in substantial problem, a survey of NHS general Ireland, Dublin, Ireland; psychiatrists and general physicians alike. Although some hospitals conducted in 2000 and 2003 indicated 2 Department of Psychiatry, patients have mild symptoms and may even be managed that only 12.8% had a dedicated alcohol worker.6 In Mayo Clinic, Rochester, MN, in the outpatient setting, others have more severe addition, few guidelines exist promoting the USA symptoms or a history of adverse outcomes that requires initiation of clear and uniform AWS treatment 7–9 Correspondence to: close inpatient supervision and benzodiazepine therapy. -

Episodic Memory, Semantic Memory and the Epistemic Asymmetry
1 Remembering past experiences: episodic memory, semantic memory and the epistemic asymmetry Christoph Hoerl forthcoming in K. Michaelian, D. Debus & D. Perrin (eds.): New Directions in the Philosophy of Memory. Routledge. There seems to be a distinctive way in which we can remember events we have experienced ourselves, which differs from the capacity to retain information about events that we can also have when we have not experienced those events ourselves but just learned about them in some other way. Psychologists and increasingly also philosophers have tried to capture this difference in terms of the idea of two different types of memory: episodic memory and semantic memory. Yet, the demarcation between episodic memory and semantic memory remains a contested topic in both disciplines, to the point of there being researchers in each of them who question the usefulness of the distinction between the two concepts.1 In this paper, I outline a new characterization of the difference between episodic memory and semantic memory, which connects that difference to what is sometimes called the ‘epistemic asymmetry’ between the past and the future, or the ‘epistemic arrow’ of time. My proposal will be that episodic memory and semantic memory exemplify the epistemic asymmetry in two different ways, and for somewhat different reasons, and that the way in which 1 The episodic/semantic distinction originates with Tulving (1972), and has been refined by Tulving in a number of other works (Tulving, 1985, 2002; Wheeler, Stuss, & Tulving, 1997). Rival ways of carving up the domain of memories are suggested, for instance, in Bernecker (2010) and Rubin and Umanath (2015). -
Alcohol-Related Brain Injury (ARBI)
If English is not your first language and you need help, please contact the Interpretation and Translation Service Jeśli angielski nie jest twoim pierwszym językiem i potrzebujesz pomocy, skontaktuj się z działem tłumaczeń ustnych i pisemnych ا رﮔ ا یزﯾرﮕﻧ پآ ﯽﮐ ﮩﭘ ﯽﻠ ﺑز نﺎ ںﯾﮩﻧ ﮯﮨ روا پآ وﮐ ددﻣ ﯽﮐ ترورﺿ ﮯﮨ وﺗ ، هارﺑ مرﮐ ﯽﻧﺎﻣﺟرﺗ روا ہﻣﺟرﺗ تﻣدﺧ تﻣدﺧ ہﻣﺟرﺗ روا ﯽﻧﺎﻣﺟرﺗ مرﮐ هارﺑ ، وﺗ ﮯﮨ ترورﺿ ﯽﮐ ددﻣ وﮐ پآ روا ﮯﮨ ںﯾﮩﻧ ﮯﺳ ر ا ﺑ ط ہ ﮐ ر ﯾ ںﯾرﮐ ﮯ Dacă engleza nu este prima ta limbă și ai nevoie de ajutor, te rugăm să contactezi Serviciul de interpretare și traducere Alcohol-Related Brain ইংরাজী যিদ আপনার .থম ভাষা না হয় এবং আপনার সাহােয9র .েয়াজন হয় তেব অনু=হ কের ?দাভাষী এবং অনুবাদ পিরেষবা@েত ?যাগােযাগ কBন Injury (ARBI) إ ذ ا مﻟ نﻛﺗ ﻠﺟﻧﻹا ﺔﯾزﯾ ﻲھ كﺗﻐﻟ ﻰﻟوﻷا ﺗﺣﺗو جﺎ إ ﻰﻟ ةدﻋﺎﺳﻣ ، ﻰﺟرﯾﻓ لﺎﺻﺗﻻا ﺔﻣدﺧﺑ ا ﻟ ﺔﻣﺟرﺗ ا ﺔﯾوﻔﺷﻟ او ﻟ ﺔﯾرﯾرﺣﺗ وﺔوﺷ ﻣر ﻣﺧ ﺎﺗاﻰرﻓ،ةﻋﺳ ﻟإج ﺣوﻰواكﻐ ھﺔز ﺟﻹ ﻛ ﻟ An information guide : 0161 627 8770 : [email protected] To improve our care environment for Patients, Visitors and Staff, Northern Care Alliance NHS Group is Smoke Free including buildings, grounds & car parks. For advice on stopping smoking contact the Specialist Stop Smoking Service on 01706 517 522 For general enquiries please contact the Patient Advice and Liaison Service (PALS) on 0161 604 5897 For enquiries regarding clinic appointments, clinical care and treatment please contact 0161 624 0420 and the Switchboard Operator will put you through to the correct department / service The Northern Care Alliance NHS Group (NCA) is one of the largest NHS organisations The Northern Care Alliance NHS Group (NCA) is one of the largest NHS organisationsin the country, employingin the country 17,000 bringing staff and together providing two a NHS range Trusts, of hospital Salford and Royalcommunity NHS Foundationhealthcare services Trust and to around The Pennine 1 million Acute people Hospitals across Salford, NHS Trust.