Obstructive Sleep Apnea Diagnosis and Treatment
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Diseases of Airway-Tracheal Diverticulum: a Review of the Literature
Review Article The diseases of airway-tracheal diverticulum: a review of the literature Asli Tanrivermis Sayit, Muzaffer Elmali, Dilek Saglam, Cetin Celenk Department of Radiology, Faculty of Medicine, Ondokuz Mayis University, Samsun, Turkey Contributions: (I) Conception and design: A Tanrivermis Sayit; (II) Administrative support: M Elmali, C Celenk; (III) Provision of study materials or patients: A Tanrivermis Sayit; (IV) Collection and assembly of data: A Tanrivermis Sayit, D Saglam; (V) Data analysis and interpretation: A Tanrivermis Sayit, M Elmali, C Celenk; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Asli Tanrivermis Sayit. Department of Radiology, Faculty of Medicine, Ondokuz Mayis University, 55139, Atakum/Samsun, Turkey. Email: [email protected]. Abstract: Tracheal diverticulum (DV) is a type of paratracheal air cyst (PTAC) that is often asymptomatic and usually detected incidentally by imaging methods. Tracheal DV are divided into two subgroups: congenital and acquired. Dysphagia, odynophagia, neck pain, hoarseness, hemoptysis, choking, and recurrent episodes of hiccups and burping can also be seen in symptomatic patients. Thin-section multidetector computed tomography (MDCT) is useful for diagnosis of tracheal diverticulum. The relationship between DV and tracheal lumen can be demonstrated by axial, coronal, and sagittal reformat multiplanar images. Bronchoscopy can also be used in diagnosis for tracheal DV. However, the connection between DV and tracheal lumen can not be shown easily with bronchoscopy. Conservative treatment is the preferred treatment in asymptomatic patients. Surgical or conservative treatment can be performed for symptomatic patients, depending on patient age and physical condition. Keywords: Trachea; diverticulum (DV); thorax; multidetector computed tomography; tracheal diseases; chronic obstructive pulmonary disease (CODP) Submitted Sep 17, 2016. -

PQI 15 Asthma in Younger Adults Admission Rate
AHRQ Quality Indicators™ (AHRQ QI™) ICD-10-CM/PCS Specification v2021 Prevention Quality Indicator 15 (PQI 15) Asthma in Younger Adults Admission Rate July 2021 Area-Level Indicator Type of Score: Rate Prepared by: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services www.qualityindicators.ahrq.gov DESCRIPTION Admissions for a principal diagnosis of asthma per 100,000 population, ages 18 to 39 years. Excludes admissions with an indication of cystic fibrosis or anomalies of the respiratory system, obstetric admissions, and transfers from other institutions. [NOTE: The software provides the rate per population. However, common practice reports the measure as per 100,000 population. The user must multiply the rate obtained from the software by 100,000 to report admissions per 100,000 population.] NUMERATOR Discharges, for patients ages 18 through 39 years, with a principal ICD-10-CM diagnosis code for asthma (ACSASTD*). [NOTE: Obstetric discharges are not included in the PQI rate for PQI 15, though the AHRQ QI™ does not explicitly exclude obstetric cases. By definition, discharges with a principal diagnosis of asthma exclude obstetric discharges, because the principal diagnosis for an obstetric discharge would identify it as obstetric, and no such diagnoses are included in the set of qualifying diagnoses.] July 2021 1 of 5 AHRQ QI™ ICD-10-CM/PCS Specification v2021 PQI 15 Asthma in Younger Adults Admission Rate www.qualityindicators.ahrq.gov NUMERATOR EXCLUSIONS Exclude cases: • with any listed ICD-10-CM -

XI. COMPLICATIONS of PREGNANCY, Childbffith and the PUERPERIUM 630 Hydatidiform Mole Trophoblastic Disease NOS Vesicular Mole Ex
XI. COMPLICATIONS OF PREGNANCY, CHILDBffiTH AND THE PUERPERIUM PREGNANCY WITH ABORTIVE OUTCOME (630-639) 630 Hydatidiform mole Trophoblastic disease NOS Vesicular mole Excludes: chorionepithelioma (181) 631 Other abnormal product of conception Blighted ovum Mole: NOS carneous fleshy Excludes: with mention of conditions in 630 (630) 632 Missed abortion Early fetal death with retention of dead fetus Retained products of conception, not following spontaneous or induced abortion or delivery Excludes: failed induced abortion (638) missed delivery (656.4) with abnormal product of conception (630, 631) 633 Ectopic pregnancy Includes: ruptured ectopic pregnancy 633.0 Abdominal pregnancy 633.1 Tubalpregnancy Fallopian pregnancy Rupture of (fallopian) tube due to pregnancy Tubal abortion 633.2 Ovarian pregnancy 633.8 Other ectopic pregnancy Pregnancy: Pregnancy: cervical intraligamentous combined mesometric cornual mural - 355- 356 TABULAR LIST 633.9 Unspecified The following fourth-digit subdivisions are for use with categories 634-638: .0 Complicated by genital tract and pelvic infection [any condition listed in 639.0] .1 Complicated by delayed or excessive haemorrhage [any condition listed in 639.1] .2 Complicated by damage to pelvic organs and tissues [any condi- tion listed in 639.2] .3 Complicated by renal failure [any condition listed in 639.3] .4 Complicated by metabolic disorder [any condition listed in 639.4] .5 Complicated by shock [any condition listed in 639.5] .6 Complicated by embolism [any condition listed in 639.6] .7 With other -

Paratracheal Air Cysts: Prevalence and Relevance to Pulmonary Emphysema and Bronchiectasis Using Thoracic Multidetector CT
Diagn Interv Radiol 2015; 21:42–46 CHEST IMAGING © Turkish Society of Radiology 2015 ORIGINAL ARTICLE Paratracheal air cysts: prevalence and relevance to pulmonary emphysema and bronchiectasis using thoracic multidetector CT Nurefsan Boyaci, Dilek Sen Dokumaci, Ekrem Karakas, Funda Yalcin, Ayse Gul Oney Kurnaz PURPOSE aratracheal air cysts (PTACs) are small collections of air adjacent to We aimed to determine the prevalence of paratracheal air the trachea at the level of the thoracic inlet (1). Pathological diag- cysts (PTACs) and the relationship of PTACs with emphysema nosis of PTACs in surgically confirmed cases includes tracheal di- and bronchiectasis through retrospective analysis of multide- P tector computed tomography (MDCT) findings. verticulum, lymphoepithelial cyst, and bronchogenic cyst (1–3). These cysts are covered with ciliary columnar epithelium and connected with METHODS MDCT findings of 1027 consecutive patients who underwent the trachea (4). The majority of PTACs are reported as tracheal divertic- routine thorax examination between January 2012 and Janu- ula in the literature, due to their connection with the trachea (2). The ary 2013 were evaluated retrospectively for the presence of thoracic inlet between the cartilage and muscle layers in right postero- PTACs. Localization of the PTACs, as well as their size, shape, and relationship with the trachea were examined. Presence lateral wall of the trachea is the most common location for PTACs. A of emphysema and bronchiectasis was recorded, and bron- relationship may be seen between an isolated PTAC and the trachea l chiectasis severity index was calculated when present. We randomly selected 80 patients who had no visible PTACs as lumen (5). -

The Respiratory System
Embryology18 Dr.Ban The respiratory system Respiratory system development is a highly coordinated and complex process it’s development is tightly associated with the digestive system from the beginning.The respiratory tract is divided anatomically into 2 main parts: A-upper respiratory tract, consisting of the nose, nasal cavity and the pharynx B-lower respiratory tract consisting of the larynx, trachea, bronchi and the lungs. The pharynx is the part of the throat behind the mouth and nasal cavity, and above the esophagus and larynx. In humans, the pharynx is part of the digestive system and the conducting zone of the respiratory system. The conducting zone which also includes the nostrils of the nose, the larynx, trachea, bronchi, and bronchioles filters, warms and moistens air and conducts it into the lungs). The human pharynx is divided into three sections: . nasopharynx . oropharynx . laryngopharynx 1 Embryology18 Dr.Ban The larynx The internal lining of the larynx originates from endoderm, but the cartilages and muscles originate from mesenchyme of the 4th and 6th pharyngeal arches. As a result of rapid proliferation of this mesenchyme, the laryngeal orifice changes in appearance from a sagital slit to a T-shaped opening. When the mesenchyme of the two arches transforms into the thyroid, cricoid and arytenoid cartilages the adult shape of the laryngeal orifice can be recognized. The laryngeal epithelium proliferates rapidly, resulting in a temporary occlusion of the lumen. Subsequently, vacuolization and recanalization produces a pair of lateral recesses, the laryngeal ventricles that are bounded by folds of tissue that differentiate into the false and true vocal cords. -

Tracheal and Bronchial Surgery
Tracheal and Bronchial Surgery 1A031 Honorary Editors: Douglas E. Wood, Douglas J. Mathisen, Erino Angelo Rendina Editors: Xiaofei Li, Federico Venuta, David C. van der Zee Associate Editors: Dirk Van Raemdonck, Federico Rea, Jinbo Zhao Xiaofei Li, Federico Venuta, David C. van der Zee Xiaofei Li, Federico Venuta, Editors: Tracheal and Bronchial Surgery Honorary Editors: Douglas E. Wood, Douglas J. Mathisen, Erino Angelo Rendina Editors: Xiaofei Li, Federico Venuta, David C. van der Zee Associate Editors: Dirk Van Raemdonck, Federico Rea, Jinbo Zhao AME Publishing Company Room C 16F, Kings Wing Plaza 1, NO. 3 on Kwan Street, Shatin, NT, Hong Kong Information on this title: www.amegroups.com For more information, contact [email protected] Copyright © AME Publishing Company. All rights reserved. This publication is in copyright. Subject to statutory exception and to the provisions of relevant collective licensing agreements, no reproduction of any part may take place without the written permission of AME Publishing Company. First published 2017 Printed in China by AME Publishing Company Editors: Xiaofei Li, Federico Venuta, David C. van der Zee Cover Image Illustrator: Zhijing Xu, Shanghai, China Tracheal and Bronchial Surgery Hardcover ISBN: 978-988-77841-8-0 AME Publishing Company, Hong Kong AME Publishing Company has no responsibility for the persistence or accuracy of URLs for external or third-party internet websites referred to in this publication, and does not guarantee that any content on such websites is, or will remain, accurate or appropriate. The advice and opinions expressed in this book are solely those of the author and do not necessarily represent the views or practices of AME Publishing Company. -

Thieme: Directdiagnosis in Radiology -- Pediatric Imaging
Index right, with aberrant left subclavian A artery 60, 68 abdomen, free fluid 165 aortopulmonary collateral arteries, abdominal trauma 162–165, major (MAPCAs) 71, 73 163, 164, 165 Apert syndrome 296 abscess appendicitis 134, 135–137, 136, 144 Brodie 225, 227, 227, 247 apple peel deformity 119 pericecal 135, 136 arachnoid cyst 307 pulmonary 21, 24, 27, 33 arteria lusoria 57–58, 58 retropharyngeal 98–100, 99 arteriovenous malformation subperiosteal 319, 320 (AVM) 280–283 accidental injuries 294 aspiration acetabular index 269 foreign body 44–46, 45, 46 acoustic neurinomas (vestibular pneumonia 118 schwannomas) 322, 324, 325, 326 recurrent 43 acute disseminated encephalo- asthma 43, 45 myelitis 336 astrocytoma 323, 325 acute lymphatic leukemia (ALL) pilocytic see pilocytic astrocytoma 263–265, 264, 294 atrial septal defect (ASD) 80–82, 81 adolescents differential diagnosis 70, 79, 84, 89 acute hematogenous osteo- avascular necrosis of femoral myelitis 225 head 273 transitional fractures 288–289, 290 axonal injuries, intracranial 340 adrenal hemorrhage 195–197, 196, 197, 200 B adrenal hyperplasia, congenital 196 air portogram 105, 106, 107 basal ganglia, dysgenesis of 301 Alagille syndrome 149 battered child syndrome anal atresia 122–125, 123 see child abuse anal stenosis 129 Beckwith–Wiedeman syndrome Andre von Rosen line 269 159, 190 aneurysmal bone cyst 233–236, 234, bell clapper deformity 215 235, 256 benign fibrous histiocytoma 232 anomalous pulmonary venous biliary atresia 148–150, 149, 159 connection 76, 86–89, 88 biloma 154 partial (PAPVC) 86, 87, 89 birth trauma 90, 195, 294 total (TAPVC) 86, 87 bizarre parosteal osteochondromatous antrum 134 proliferation 243 aorta bladder coarctation 62–65, 63 masses 179 pseudo-coarctation 65 neurogenic 182 aortic arch rhabdomyosarcoma 201, 202, discontinuous 65 203, 204 double 57, 59–61, 60, 68 Blalock–Taussig shunts 71, 72, 76 Blount disease 220 Bochdalek hernia 28 bone abscess see Brodie abscess Page numbers in italics refer to bone cysts 261 illustrations. -

Huge Tracheal Diverticulum in a Patient with Mounier-Kuhn Syndrome
European Journal of Case Reports in Internal Medicine Huge Tracheal Diverticulum in a Patient with Mounier-Kuhn Syndrome Michele Mondoni1, Paolo Carlucci1, Elena Maria Parazzini1, Paolo Busatto2, Stefano Centanni1 1Respiratory Unit, San Paolo Hospital, Dept. of Scienze della Salute, Università degli Studi di Milano, Milan, Italy 2UO Pneumologia, San Luca Hospital, USL Nordovest Toscana, Lucca, Italy Doi: 10.12890/2016_000419 - European Journal of Case Reports in Internal Medicine - © EFIM 2016 Received: 01/03/2016 Accepted: 16/03/2016 Published: 15/06/2016 How to cite this article: Mondoni M, Carlucci P, Parazzini EM, Busatto P, Centanni S. Huge tracheal diverticulum in a patient with Mounier-Kuhn syndrome EJCRIM 2016;3:doi:10.12890/2016_000419 Conflicts of Interests: The Authors declare that there are no competing interests. This article is licensed under a Commons Attribution Non-Commercial 4.0 License ABSTRACT Tracheal diverticulum is a rare benign entity. Tracheobronchomegaly (TBM), also known as Mounier-Kuhn syndrome, is a rare disorder characterized by marked dilation of the trachea and main bronchi, associated with thinning or atrophy of the elastic tissue. Because of the weakened trachea and increased intraluminal pressure related to chronic cough, some patients may develop mucosal herniation leading to tracheal diverticulosis. We report the case of a patient with TBM with a huge tracheal diverticulum, diagnosed by bronchoscopy and computed tomography with three-dimensional reconstruction. to our knowledge this is the largest tracheal diameter described in a patient affected by this syndrome. LEARNING POINTS • Tracheal diverticulum is a rare condition that should be considered in the presence of bronchopulmonary disorders characterized by chronic cough and repeated bronchial infection, such as Mounier-Kuhn syndrome. -

Incidental Paratracheal Air Cyst in Papillary Thyroid Cancer Patient: a Case Report
2339 Case Report Incidental paratracheal air cyst in papillary thyroid cancer patient: a case report Min Jhi Kim^, Hera Jung, Cheong Soo Park Department of Surgery, CHA Ilsan Medical Center, Cha University School of Medicine, Goyang-si, Gyeonggi-do, South Korea Correspondence to: Cheong Soo Park, MD, PhD. Department of Surgery, CHA Ilsan Medical Center, Cha University School of Medicine, 1205, Jungang-ro, Ilsandong-gu, Goyang-si, Gyeonggi-do, South Korea. Email: [email protected]. Abstract: Paratracheal air cyst (PTAC) is a collection of air in the right posterior side of the trachea with an uncertain etiology. We report a papillary thyroid cancer patient with a PTAC that was removed during thyroid cancer surgery. A 68-year-old woman was diagnosed with right papillary thyroid cancer with suspicion of central lymph node metastasis. She had a history of hypertension and a rear-end collision car accident 20 years prior. On computed tomography, an ovoid cyst was incidentally found in the paratracheal region at the thoracic inlet level. Emphysematous lung with an obstructive lung defect was noted without any symptoms. Bilateral total thyroidectomy with ipsilateral central compartment neck dissection was indicated for the patient. During surgery, removal of the cyst was inevitable for complete central neck dissection. Histopathologic analysis revealed an etiology of tracheal mucus sprouting through weak trachea points. No postoperative complications occurred. The patient continued on levothyroxine medication without further radioactive iodine therapy. After 6 months, follow-up ultrasound showed no evidence of recurrence. We hypothesized that obstructive lung disease with impaired lung function or trauma history might have contributed to the development of PTAC. -

Series. Indexing and Abstracting Publications Litted Indude" Indexes, Abstracts
DOCUMINT 11111SUNS EDon576 EC 003 1106 BrLunin. Lois F., Ed. Information Sources in Hearing, Speech. and Communication Disorders. Part L Publications. Developmental EcStion. Information Center for Hearing, Speech. and Disorders of Human Communication, Baltimore. Md. Pub Date 68 Note-311p. EDRS Price Mr-S125 HC-S15.65 Descriptors-Abstracts,*AnnotatedBibliographies.*AurauyHanckapped.Betliografhies.Dictionaries. Directories. *Exceptional Chid Services, FAms, Glossaries. Guides, Indexes (Locaters), Information Sources. *Language Hanckapped. Literature Reviews, Periockals, Publications. Research Reviews (Publications). *Speech Handicapped, Textbooks This guide to recent sources of published inforMation in hearincj, speech. and con yntrnication disorders lists 759 references.The items are arranged in nine major sections and are annotated- except when reasons of processing prevent. The section on reviews covers hearing. language. speech. andadditional reviews; the section on special serials contains review journals. annual and irregular review serials. status reports of laboratories, statistical survey series.i translation serials. and publishers' series. Indexing and abstracting publications litted indude" indexes, abstracts. research in progress. and meetings; gt tides and directories cover members and_ individuals, societies and associations: centers and services, professional training. and funding. Additional sections contain core and cognate journals; hearing. language. speech. and cognate Area bibliographies; English language. deaf language. -

General Thoracic Crosswalk ICD-9 to ICD-10
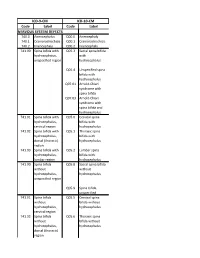
General Thoracic Surgery ICD9 to ICD10 Crosswalks ICD-9 Code ICD-9 Description ICD-10 Code ICD-10 Description 150.3 Malignant neoplasm of upper third of esophagus C15.3 Malignant neoplasm of upper third of esophagus 150.4 Malignant neoplasm of middle third of esophagus C15.4 Malignant neoplasm of middle third of esophagus 150.5 Malignant neoplasm of lower third of esophagus C15.5 Malignant neoplasm of lower third of esophagus 150.9 Malignant neoplasm of esophagus, unspecified C15.9 Malignant neoplasm of esophagus, unspecified site 151.0 Malignant neoplasm of cardia C16.0 Malignant neoplasm of cardia 151.9 Malignant neoplasm of stomach, unspecified site C16.9 Malignant neoplasm of stomach, unspecified 162.0 Malignant neoplasm of trachea C33 Malignant neoplasm of trachea 162.2 Malignant neoplasm of main bronchus C34.00 Malignant neoplasm of unspecified main bronchus 162.2 Malignant neoplasm of main bronchus C34.01 Malignant neoplasm of right main bronchus 162.2 Malignant neoplasm of main bronchus C34.02 Malignant neoplasm of left main bronchus 162.3 Malignant neoplasm of upper lobe, bronchus or C34.10 Malignant neoplasm of upper lobe, unspecified lung bronchus or lung 162.3 Malignant neoplasm of upper lobe, bronchus or C34.11 Malignant neoplasm of upper lobe, right bronchus lung or lung 162.3 Malignant neoplasm of upper lobe, bronchus or C34.12 Malignant neoplasm of upper lobe, left bronchus lung or lung 162.4 Malignant neoplasm of middle lobe, bronchus or C34.2 Malignant neoplasm of middle lobe, bronchus or lung lung 162.5 Malignant neoplasm -
Code Label Code Label NERVOUS SYSTEM DEFECTS ICD-9-CM ICD-10-CM
ICD-9-CM ICD-10-CM Code Label Code Label NERVOUS SYSTEM DEFECTS 740.0 Anencephalus Q00.0 Anencephaly 740.1 Craniorachischisis Q00.1 Craniorachischisis 740.2 Iniencephaly Q00.2 Iniencephaly 741.00 Spina bifida with Q05.3 Sacral spina bifida hydrocephalus, with unspecified region hydrocephalus Q05.4 Unspecified spina bifida with hydrocephalus Q07.01 Arnold-Chiari syndrome with spina bifida Q07.03 Arnold-Chiari syndrome with spina bifida and hydrocephalus 741.01 Spina bifida with Q05.0 Cervical spina hydrocephalus, bifida with cervical region hydrocephalus 741.02 Spina bifida with Q05.1 Thoracic spina hydrocephalus, bifida with dorsal (thoracic) hydrocephalus region 741.03 Spina bifida with Q05.2 Lumbar spina hydrocephalus, bifida with lumbar region hydrocephalus 741.90 Spina bifida Q05.8 Sacral spina bifida without without hydrocephalus, hydrocephalus unspecified region Q05.9 Spina bifida, unspecified 741.91 Spina bifida Q05.5 Cervical spina without bifida without hydrocephalus, hydrocephalus cervical region 741.92 Spina bifida Q05.6 Thoracic spina without bifida without hydrocephalus, hydrocephalus dorsal (thoracic) region 741.93 Spina bifida Q05.7 Lumbar spina without bifida without hydrocephalus, hydrocephalus lumbar region 742.0 Encephalocele Q01.0 Frontal encephalocele Q01.1 Nasofrontal encephalocele Q01.2 Occipital encephalocele Q01.8 Encephalocele of other sites Q01.9 Encephalocele, unspecified 742.1 Microcephalus Q02 Microcephaly 742.2 Reducation Q04.0 Congenital deformities of malformations of brain corpus callosum Q04.1 Arhinencephaly