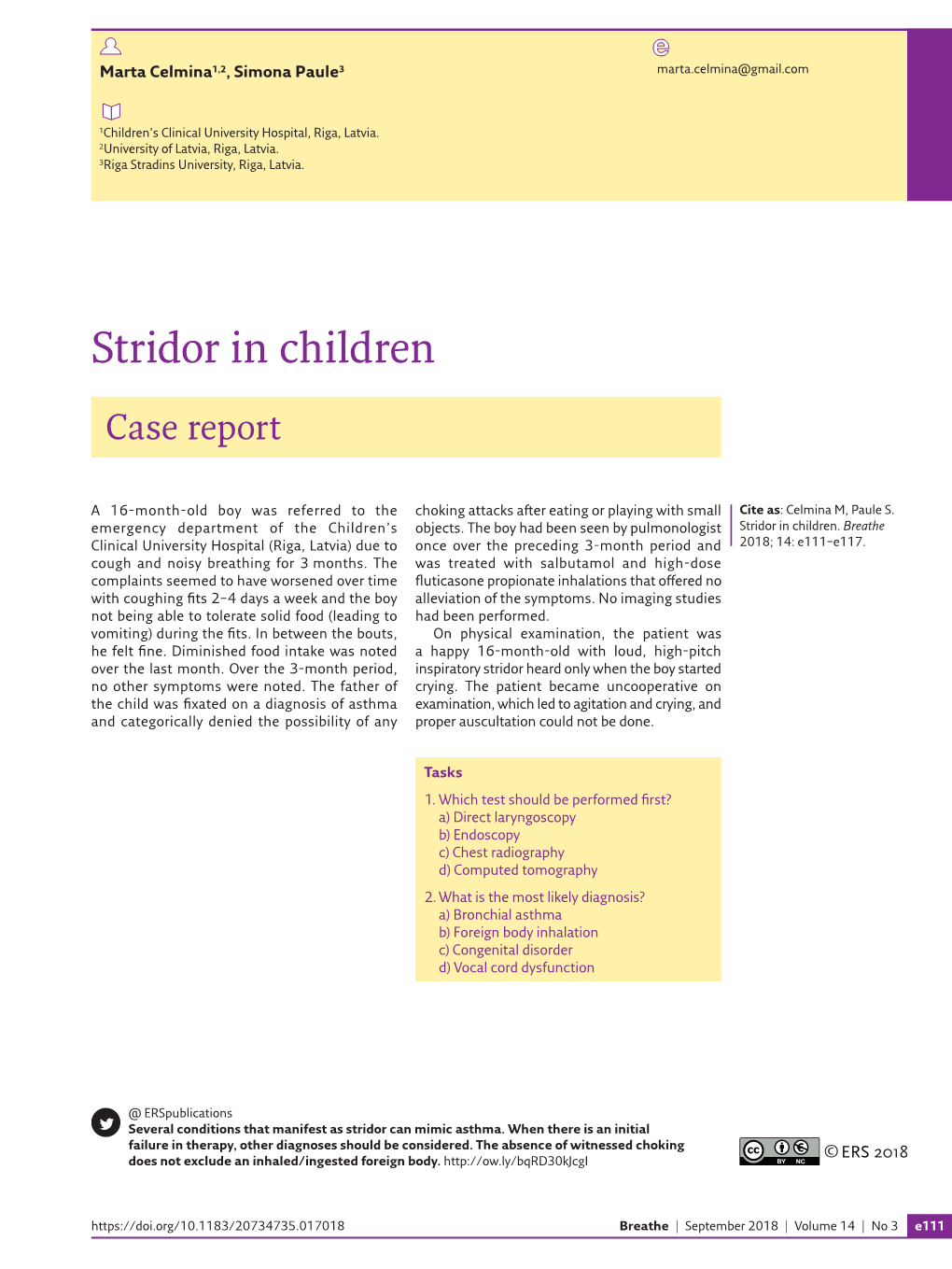
Stridor in Children
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Inhalation of “Borax”
Journal of Paediatrics and Neonatal Disorders Volume 4 | Issue 1 ISSN: 2456-5482 Case Report Open Access Inhalation of “Borax” and Risk of Severe Stridor Obaid O* Department of Pediatrics, MOH, Makkah, Saudi Arabia *Corresponding author: Obaid O, Department of Pediatrics, MOH, Makkah, Saudi Arabia, Tel: 00966500606352, E-mail: [email protected] Citation: Obaid O (2019) Inhalation of “Borax” and Risk of Severe Stridor. J Paedatr Neonatal Dis 4(1): 105 Received Date: March 21, 2019 Accepted Date: June 26, 2019 Published Date: June 28, 2019 Abstract Stridor in children is not uncommon reason to visit emergency department and usually due to croup but inhalation of toxic substance may cause severe stridor which is uncommon. Keywords: Stridor; Pediatric; Sodium Burate Case Report A 9 year old Saudi girl presented to emergency department accompanied by her grandmother with history of dry cough, shortness of breath and audible wheeze for more than12 hours. She has no history of fever, foreign body ingestion and chronic cough. No history of contact with sick person and no history of lip swelling or skin rash. Her vaccination status up to date. She was a Preterm 30 weeks, admitted to Neonatal intensive care for 2 months and discharge well. In emergency room she was ill looking with biphasic stridor, kept on oxygen 10 liter/min and given one dose IM epinephrine 0.3 mg and nebulizer Racemic epinephrine, connected to Cardiorespiratory monitor and 2 IV lines was inserted started on IV Fluids and given one dose of dexamethasone. Urgent consultation to ENT was done and they recommend bronchoscopy to rule out Foreign body ingestion. -

Management of Airway Obstruction and Stridor in Pediatric Patients
November 2017 Management of Airway Volume 14, Number 11 Obstruction and Stridor in Authors Ashley Marchese, MD Department of Pediatrics, Yale-New Haven Hospital, New Haven, CT Pediatric Patients Melissa L. Langhan, MD, MHS Associate Professor of Pediatrics and Emergency Medicine; Fellowship Director, Director of Education, Pediatric Emergency Abstract Medicine, Yale University School of Medicine, New Haven, CT Peer Reviewers Stridor is a result of turbulent air-flow through the trachea from Steven S. Bin, MD upper airway obstruction, and although in children it is often Associate Clinical Professor of Emergency Medicine and Pediatrics; Medical Director, Emergency Department, UCSF School of Medicine, due to croup, it can also be caused by noninfectious and/or con- Benioff Children’s Hospital, San Francisco, CA genital conditions as well as life-threatening etiologies. The his- Alexander Toledo, DO, PharmD, FAAEM, FAAP tory and physical examination guide initial management, which Chief, Section of Pediatric Emergency Medicine; Director, Pediatric Emergency Department, Arizona Children’s Center at Maricopa includes reduction of airway inflammation, treatment of bacterial Medical Center, Phoenix, AZ infection, and, less often, imaging, emergent airway stabilization, Prior to beginning this activity, see “Physician CME Information” or surgical management. This issue discusses the most common on the back page. as well as the life-threatening etiologies of acute and chronic stridor and its management in the emergency department. Editor-in-Chief -

The Diseases of Airway-Tracheal Diverticulum: a Review of the Literature
Review Article The diseases of airway-tracheal diverticulum: a review of the literature Asli Tanrivermis Sayit, Muzaffer Elmali, Dilek Saglam, Cetin Celenk Department of Radiology, Faculty of Medicine, Ondokuz Mayis University, Samsun, Turkey Contributions: (I) Conception and design: A Tanrivermis Sayit; (II) Administrative support: M Elmali, C Celenk; (III) Provision of study materials or patients: A Tanrivermis Sayit; (IV) Collection and assembly of data: A Tanrivermis Sayit, D Saglam; (V) Data analysis and interpretation: A Tanrivermis Sayit, M Elmali, C Celenk; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Asli Tanrivermis Sayit. Department of Radiology, Faculty of Medicine, Ondokuz Mayis University, 55139, Atakum/Samsun, Turkey. Email: [email protected]. Abstract: Tracheal diverticulum (DV) is a type of paratracheal air cyst (PTAC) that is often asymptomatic and usually detected incidentally by imaging methods. Tracheal DV are divided into two subgroups: congenital and acquired. Dysphagia, odynophagia, neck pain, hoarseness, hemoptysis, choking, and recurrent episodes of hiccups and burping can also be seen in symptomatic patients. Thin-section multidetector computed tomography (MDCT) is useful for diagnosis of tracheal diverticulum. The relationship between DV and tracheal lumen can be demonstrated by axial, coronal, and sagittal reformat multiplanar images. Bronchoscopy can also be used in diagnosis for tracheal DV. However, the connection between DV and tracheal lumen can not be shown easily with bronchoscopy. Conservative treatment is the preferred treatment in asymptomatic patients. Surgical or conservative treatment can be performed for symptomatic patients, depending on patient age and physical condition. Keywords: Trachea; diverticulum (DV); thorax; multidetector computed tomography; tracheal diseases; chronic obstructive pulmonary disease (CODP) Submitted Sep 17, 2016. -

PQI 15 Asthma in Younger Adults Admission Rate
AHRQ Quality Indicators™ (AHRQ QI™) ICD-10-CM/PCS Specification v2021 Prevention Quality Indicator 15 (PQI 15) Asthma in Younger Adults Admission Rate July 2021 Area-Level Indicator Type of Score: Rate Prepared by: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services www.qualityindicators.ahrq.gov DESCRIPTION Admissions for a principal diagnosis of asthma per 100,000 population, ages 18 to 39 years. Excludes admissions with an indication of cystic fibrosis or anomalies of the respiratory system, obstetric admissions, and transfers from other institutions. [NOTE: The software provides the rate per population. However, common practice reports the measure as per 100,000 population. The user must multiply the rate obtained from the software by 100,000 to report admissions per 100,000 population.] NUMERATOR Discharges, for patients ages 18 through 39 years, with a principal ICD-10-CM diagnosis code for asthma (ACSASTD*). [NOTE: Obstetric discharges are not included in the PQI rate for PQI 15, though the AHRQ QI™ does not explicitly exclude obstetric cases. By definition, discharges with a principal diagnosis of asthma exclude obstetric discharges, because the principal diagnosis for an obstetric discharge would identify it as obstetric, and no such diagnoses are included in the set of qualifying diagnoses.] July 2021 1 of 5 AHRQ QI™ ICD-10-CM/PCS Specification v2021 PQI 15 Asthma in Younger Adults Admission Rate www.qualityindicators.ahrq.gov NUMERATOR EXCLUSIONS Exclude cases: • with any listed ICD-10-CM -

Supraglottoplasty Home Care Instructions Hospital Stay Most Children Stay Overnight in the Hospital for at Least One Night
10914 Hefner Pointe Drive, Suite 200 Oklahoma City, OK 73120 Phone: 405.608.8833 Fax: 405.608.8818 Supraglottoplasty Home Care Instructions Hospital Stay Most children stay overnight in the hospital for at least one night. Bleeding There is typically very little to no bleeding associated with this procedure. Though very unlikely to happen, if your child were to spit or cough up blood you should contact your physician immediately. Diet After surgery your child will be able to eat the foods or formula that they usually do. It is important after surgery to encourage your child to drink fluids and remain hydrated. Daily fluid needs are listed below: • Age 0-2 years: 16 ounces per day • Age 2-4 years: 24 ounces per day • Age 4 and older: 32 ounces per day It is our experience that most children experience a significant improvement in eating after this procedure. However, we have found about that approximately 4% of otherwise healthy infants may experience a transient onset of coughing or choking with feeding after surgery. In our experience these symptoms resolve over 1-2 months after surgery. We have also found that infants who have other illnesses (such as syndromes, prematurity, heart trouble, or other congenital abnormalities) have a greater risk of experiencing swallowing difficulties after a supraglottoplasty (this number can be as high as 20%). In time the child usually will return to normal swallowing but there is a small risk of feeding difficulties. You will be given a prescription before you leave the hospital for an acid reducing (anti-reflux) medication that must be filled before you are discharged. -

Stridor in the Newborn
Stridor in the Newborn Andrew E. Bluher, MD, David H. Darrow, MD, DDS* KEYWORDS Stridor Newborn Neonate Neonatal Laryngomalacia Larynx Trachea KEY POINTS Stridor originates from laryngeal subsites (supraglottis, glottis, subglottis) or the trachea; a snoring sound originating from the pharynx is more appropriately considered stertor. Stridor is characterized by its volume, pitch, presence on inspiration or expiration, and severity with change in state (awake vs asleep) and position (prone vs supine). Laryngomalacia is the most common cause of neonatal stridor, and most cases can be managed conservatively provided the diagnosis is made with certainty. Premature babies, especially those with a history of intubation, are at risk for subglottic pathologic condition, Changes in voice associated with stridor suggest glottic pathologic condition and a need for otolaryngology referral. INTRODUCTION Families and practitioners alike may understandably be alarmed by stridor occurring in a newborn. An understanding of the presentation and differential diagnosis of neonatal stridor is vital in determining whether to manage the child with further observation in the primary care setting, specialist referral, or urgent inpatient care. In most cases, the management of neonatal stridor is outside the purview of the pediatric primary care provider. The goal of this review is not, therefore, to present an exhaustive review of causes of neonatal stridor, but rather to provide an approach to the stridulous newborn that can be used effectively in the assessment and triage of such patients. Definitions The neonatal period is defined by the World Health Organization as the first 28 days of age. For the purposes of this discussion, the newborn period includes the first 3 months of age. -

Factors Associated with Pleurisy in Pigs: a Case-Control Analysis of Slaughter Pig Data for England and Wales
Aus dem Zentrum für Klinische Tiermedizin der Tierärztlichen Fakultät der Ludwig-Maximilians-Universität München Arbeit angefertigt unter der Leitung von Prof. Dr. Mathias Ritzmann Angefertigt am Cambridge Infectious Diseases Consortium, University of Cambridge, Department of Veterinary Medicine, Cambridge, UK (Dr. A W (Dan) Tucker) Factors associated with pleurisy in pigs: A case-control analysis of slaughter pig data for England and Wales Inaugural-Dissertation zur Erlangung der tiermedizinischen Doktorwürde der Tierärztlichen Fakultät der Ludwig-Maximilians-Universität München Von Henrike Caroline Jäger aus Wiesbaden München 2012 Gedruckt mit der Genehmigung der Tierärztlichen Fakultät der Ludwig-Maximilians-Universität München Dekan: Univ.-Prof. Dr. Joachim Braun Berichterstatter: Univ.-Prof. Dr. Mathias Ritzmann Korreferent: Univ.-Prof. Dr. Dr. habil. Manfred Gareis Tag der Promotion: 9. Februar 2013 Meinem Vater Dr. med Sepp-Dietrich Jäger Table of Contents 4 TABLE OF CONTENTS I. INTRODUCTION ...................................................................................... 7 II. LITERATURE OVERVIEW .................................................................... 8 1. Anatomy and Physiology of the Pleura ....................................................8 2. Pleurisy ........................................................................................................9 2.1. Morphology ..................................................................................................9 2.2. Prevalence ..................................................................................................11 -
Exercise-Induced Laryngeal Obstruction
American Thoracic Society PATIENT EDUCATION | INFORMATION SERIES Exercise-induced Laryngeal Obstruction Exercise-induced laryngeal obstruction (EILO) is a breathing problem that affects people during exercise. EILO is defined by inappropriate narrowing of the upper airway at the level of the vocal cords (glottis) and/or supraglottis (above the vocal cords). This can make it hard to get air into your lungs during exercise and cause a noisy breathing that can be frightening. EILO has also been called vocal cord dysfunction (VCD) or paradoxical vocal fold motion (PVFM). Most people with EILO only have symptoms when they Common signs and symptoms of EILO exercise, those some people may have the problem at During (or immediately after) high-intensity exercise, other times as well. (See ATS Patient Information Series with EILO you may experience: fact sheet ‘Inducible Laryngeal Obstruction/Vocal Cord ■■ Profound shortness of breath or breathlessness Dysfunction’) ■■ Noisy breathing, particularly when breathing in Where are the vocal cords and what do they do? (stridor, gasping, raspy sounds, or “wheezing”) Your vocal cords are located in your upper airway or ■■ A feeling of choking or suffocation that can be scary larynx. Your supraglottic structures (including your ■■ CLIP AND COPY AND CLIP Feeling like there is a lump in the throat arytenoid cartilages and epiglottis) are located above the ■■ Throat or chest tightness vocal cords and are part of your larynx. The larynx is often called the voice box and is deep in your throat. When These symptoms often come on suddenly during you speak, the vocal cords vibrate as you breathe out, exercise, and are typically quite noticeable or concerning to people around you as well. -

What Is Pertussis (Whooping Cough)?
American Thoracic Society PATIENT EDUCATION | INFORMATION SERIES What Is Pertussis (Whooping Cough)? Pertussis is a very contagious respiratory infection commonly known as ‘whooping cough’. It is caused by a bacterium called Bordetella pertussis. The infection became much less common after a successful vaccine was developed and given to children to help prevent infection. However, in recent years, the number of people infected with pertussis has increased and now is at the highest rate seen since the 1950’s. There is concern that this is due mainly to people not taking the pertussis (whooping cough) vaccination and adults who have not had a booster and their immune protection has weakened with age. Whooping cough usually starts as a mild cold-like illness get in the air. If you are close enough, you can breathe in these (upper respiratory infection). The pertussis bacteria enter the droplets or they can land on your mouth, nose, or eye. You lungs and cause swelling and irritation in the airways leading can also get the infection if you kiss the face of a person with to severe coughing fits. At times, people with whooping pertussis or get infected nose or mouth secretions on your cough can have a secondary pneumonia from other bacteria hands and then touch your own face to rub your eyes or nose. while they are ill. Whooping cough can cause very serious A person with pertussis can remain contagious for many weeks illness. It is most dangerous in young babies and can result unless treated with an antibiotic. in death. It spreads very easily and people who have the infection can still spread it to others for weeks after they What are the symptoms of Pertussis infection? become sick. -
Transitioning Newborns from NICU to Home: Family Information Packet
Transitioning Newborns from NICU to Home Family Information Packet Your Health Coach has prepared this information packet for your family to help explain the medical needs of your newborn as you prepare to leave the hospital. A Health Coach helps families/ caregivers adjust to working directly with the health care providers as well as increasing your ability and confidence to care for your infant. When infants are born before their due date or with health problems, families often need help managing their baby’s health care after leaving the hospital. Since they spend the first part of their lives in the hospital, the babies and their families may find it helpful to have extra support. Your Health Coach will work with your family to teach you to care for your infant, connect with the right doctors and specialists for treatment, and find resources in your area. The role of the Health Coach is as an educator, not as a caregiver. Planning must start before hospital discharge and continue through followup with the primary care provider. After discharge from the hospital, your infant’s care must be well coordinated and clearly communicated to avoid medical errors that could harm the baby. After your infant is discharged, your Health Coach should follow up with you by phone within a few days to make sure the transition is going well. Your Health Coach will want to know how your baby is doing, whether you have any questions or concerns, if your infant has been to the scheduled appointments, etc. This information packet contains tips for getting care, understanding signs and symptoms of illness, medicines and immunizations, managing breathing problems, and feeding. -

Laryngotracheitis Caused by COVID-19
Prepublication Release A Curious Case of Croup: Laryngotracheitis Caused by COVID-19 Claire E. Pitstick, DO, Katherine M. Rodriguez, MD, Ashley C. Smith, MD, Haley K. Herman, MD, James F. Hays, MD, Colleen B. Nash, MD, MPH DOI: 10.1542/peds.2020-012179 Journal: Pediatrics Article Type: Case Report Citation: Pitstick CE, Rodriguez KM, Smith AC, Herman HK, Hays JF, Nash CB. A curious case of croup: laryngotracheitis caused by COVID-19. Pediatrics. 2020; doi: 10.1542/peds.2020-012179 This is a prepublication version of an article that has undergone peer review and been accepted for publication but is not the final version of record. This paper may be cited using the DOI and date of access. This paper may contain information that has errors in facts, figures, and statements, and will be corrected in the final published version. The journal is providing an early version of this article to expedite access to this information. The American Academy of Pediatrics, the editors, and authors are not responsible for inaccurate information and data described in this version. Downloaded from©2020 www.aappublications.org/news American Academy by of guest Pediatrics on September 30, 2021 Prepublication Release A Curious Case of Croup: Laryngotracheitis Caused by COVID-19 Claire E. Pitstick, DO, Katherine M. Rodriguez, MD, Ashley C. Smith, MD, Haley K. Herman, MD, James F. Hays, MD, Colleen B. Nash, MD, MPH Affiliations: Rush University Medical Center, Division of Pediatrics, Chicago, Illinois Address Correspondence to: Claire E. Pitstick, Department of Pediatrics, Rush University Medical Center, 1645 W Jackson Blvd Ste 200, Chicago, IL 60612 [[email protected]], 312-942-2200. -

Cough and Acute Bronchitis
Symptoms of Cough / Acute Bronchitis Symptoms of a cough / acute bronchitis may include: Cough which develops over a day or so and may become quite irritating. Fever, headache, aches and pains. Cold symptoms. Symptoms typically peak after 2-3 days, and then gradually clear. However, the cough may persist for up to three weeks after the infection has gone. This is because the inflammation in the airways, caused by the infection, can take a while to clear. Do I need an antibiotic? Most coughs / acute bronchitis are caused by a viral infection. Antibiotics DO NOT kill viruses. So you DO NOT need an antibiotic for most coughs / acute bronchitis. In people who are normally well, your own immune system will usually clear the infection. Most bouts of cough / acute bronchitis clear without complications. Antibiotics may cause side-effects such as thrush, diarrhoea, rash and stomach upsets, so they should not be taken unnecessarily. Unnecessary use of some antibiotics has caused them to become less effective. You may be prescribed antibiotics if you already have ongoing chronic lung disease. This is to prevent you developing a ‘secondary’ bacterial infection, rather than to clear a viral infection. Treatment for Cough / Acute Bronchitis Treatment options to relieve symptoms whilst waiting for your immune system to clear the infection. No treatment Many bouts of cough / acute bronchitis are mild and will usually get better soon without any treatment. Pain & fever relief Take paracetamol or ibuprofen regularly. Do not take any more than the recommended dose. Fluids Drink plenty of fluids such as water and fruit-juices to avoid dehydration.