THE DIFFERENTIAL DIAGNOSIS of HEMOPTYSIS. by W
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hemoptysis in Children
R E V I E W A R T I C L E Hemoptysis in Children G S GAUDE From Department of Pulmonary Medicine, JN Medical College, Belgaum, Karnataka, India. Correspondence to: Dr G S Gaude, Professor and Head, Department of Pulmonary Medicine, J N Medical College, Belgaum 590 010, Karnataka, India. [email protected] Received: November, 11, 2008; Initial review: May, 8, 2009; Accepted: July 27, 2009. Context: Pulmonary hemorrhage and hemoptysis are uncommon in childhood, and the frequency with which they are encountered by the pediatrician depends largely on the special interests of the center to which the child is referred. Diagnosis and management of hemoptysis in this age group requires knowledge and skill in the causes and management of this infrequently occurring potentially life-threatening condition. Evidence acquisition: We reviewed the causes and treatment options for hemoptysis in the pediatric patient using Medline and Pubmed. Results: A focused physical examination can lead to the diagnosis of hemoptysis in most of the cases. In children, lower respiratory tract infection and foreign body aspiration are common causes. Chest radiographs often aid in diagnosis and assist in using two complementary diagnostic procedures, fiberoptic bronchoscopy and high-resolution computed tomography. The goals of management are threefold: bleeding cessation, aspiration prevention, and treatment of the underlying cause. Mild hemoptysis often is caused by an infection that can be managed on an outpatient basis with close monitoring. Massive hemoptysis may require additional therapeutic options such as therapeutic bronchoscopy, angiography with embolization, and surgical intervention such as resection or revascularization. Conclusions: Hemoptysis in the pediatric patient requires prompt and thorough evaluation and treatment. -
Problems in Family Practice
problems in Family Practice Coughing in Childhood Hyman Sh ran d , M D Cambridge, M assachusetts Coughing in childhood is a common complaint involving a wide spectrum of underlying causes which require a thorough and rational approach by the physician. Most children who cough have relatively simple self-limiting viral infections, but some may have serious disease. A dry environment, allergic factors, cystic fibrosis, and other major illnesses must always be excluded. A simple clinical approach, and the sensible use of appropriate investigations, is most likely to succeed in finding the cause, which can allow precise management. The cough reflex as part of the defense mechanism of the respiratory tract is initiated by mucosal changes, secretions or foreign material in the pharynx, larynx, tracheobronchial Table 1. Persistent Cough — Causes in Childhood* tree, pleura, or ear. Acting as the “watchdog of the lungs,” the “good” cough prevents harmful agents from Common Uncommon Rare entering the respiratory tract; it also helps bring up irritant material from Environmental Overheating with low humidity the airway. The “bad” cough, on the Allergens other hand, serves no useful purpose Pollution Tobacco smoke and, if persistent, causes fatigue, keeps Upper Respiratory Tract the child (and parents) awake, inter Recurrent viral URI Pertussis Laryngeal stridor feres with feeding, and induces vomit Rhinitis, Pharyngitis Echo 12 Vocal cord palsy Allergic rhinitis Nasal polyp Vascular ring ing. It is best suppressed. Coughs and Prolonged use of nose drops Wax in ear colds constitute almost three quarters Sinusitis of all illness in young children. The Lower Respiratory Tract Asthma Cystic fibrosis Rt. -
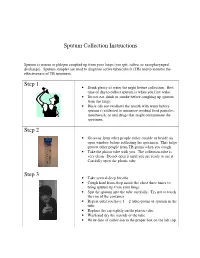
Sputum Collection Instructions Step 1 Step 2 Step 3
Sputum Collection Instructions Sputum is mucus or phlegm coughed up from your lungs (not spit, saliva, or nasopharyngeal discharge). Sputum samples are used to diagnose active tuberculosis (TB) and to monitor the effectiveness of TB treatment. Step 1 • Drink plenty of water the night before collection. Best time of day to collect sputum is when you first wake. • Do not eat, drink or smoke before coughing up sputum from the lungs. • Rinse (do not swallow) the mouth with water before sputum is collected to minimize residual food particles, mouthwash, or oral drugs that might contaminate the specimen. Step 2 • Go away from other people either outside or beside an open window before collecting the specimen. This helps protect other people from TB germs when you cough. • Take the plastic tube with you. The collection tube is very clean. Do not open it until you are ready to use it. Carefully open the plastic tube. Step 3 • Take several deep breaths. • Cough hard from deep inside the chest three times to bring sputum up from your lungs. • Spit the sputum into the tube carefully. Try not to touch the rim of the container. • Repeat until you have 1 – 2 tablespoons of sputum in the tube. • Replace the cap tightly on the plastic tube. • Wash and dry the outside of the tube. • Write date of collection in the proper box on the lab slip. Step 4 • Place the primary specimen container (usually a conical centrifuge tube) in the clear plastic baggie that has the biohazard symbol imprint. • Place the white absorbent sheet in the plastic baggie. -

Perinatal/Neonatal Case Presentation
Perinatal/Neonatal Case Presentation &&&&&&&&&&&&&& Urinary Tract Infection With Trichomonas vaginalis in a Premature Newborn Infant and the Development of Chronic Lung Disease David J. Hoffman, MD vaginal bleeding with suspected abruption resulted in delivery of Gerard D. Brown, DO the infant by Cesarean section. The Apgar scores were 1, 5, and 9 Frederick H. Wirth, MD at 1, 5, and 10 minutes of life, respectively. Betsy S. Gebert, CRNP After delivery, the infant was managed with mechanical Cathy L. Bailey, MS, CRNP ventilation with pressure support and volume guarantee for Endla K. Anday, MD respiratory distress syndrome. She received exogenous surfactant We report a case of a low-birth-weight infant with an infection of the urinary tract with Trichomonas vaginalis, who later developed cystic chronic lung disease suggestive of Wilson-Mikity syndrome. Although she had mild respiratory distress syndrome at birth, the extent of the chronic lung disease was out of proportion to the initial illness. We speculate that maternal infection with this organism may have resulted in an inflammatory response that led to its development. Journal of Perinatology (2003) 23, 59 – 61 doi:10.1038/sj.jp.7210819 CASE PRESENTATION A 956-g, appropriate-for-gestational-age, African–American female was delivered by Cesarean section following 27 5/7 weeks of gestation in breech presentation after a period of advanced cervical dilatation and uterine contractions. Her mother was a 20-year-old gravida 5, para 2022 woman whose prenatal laboratory data were significant for vaginal colonization with Streptococcus agalactiae, treatment for Chlamydia trachomatis, and a history of cocaine and marijuana usage confirmed by urine toxicology. -

Factors Associated with Pleurisy in Pigs: a Case-Control Analysis of Slaughter Pig Data for England and Wales
Aus dem Zentrum für Klinische Tiermedizin der Tierärztlichen Fakultät der Ludwig-Maximilians-Universität München Arbeit angefertigt unter der Leitung von Prof. Dr. Mathias Ritzmann Angefertigt am Cambridge Infectious Diseases Consortium, University of Cambridge, Department of Veterinary Medicine, Cambridge, UK (Dr. A W (Dan) Tucker) Factors associated with pleurisy in pigs: A case-control analysis of slaughter pig data for England and Wales Inaugural-Dissertation zur Erlangung der tiermedizinischen Doktorwürde der Tierärztlichen Fakultät der Ludwig-Maximilians-Universität München Von Henrike Caroline Jäger aus Wiesbaden München 2012 Gedruckt mit der Genehmigung der Tierärztlichen Fakultät der Ludwig-Maximilians-Universität München Dekan: Univ.-Prof. Dr. Joachim Braun Berichterstatter: Univ.-Prof. Dr. Mathias Ritzmann Korreferent: Univ.-Prof. Dr. Dr. habil. Manfred Gareis Tag der Promotion: 9. Februar 2013 Meinem Vater Dr. med Sepp-Dietrich Jäger Table of Contents 4 TABLE OF CONTENTS I. INTRODUCTION ...................................................................................... 7 II. LITERATURE OVERVIEW .................................................................... 8 1. Anatomy and Physiology of the Pleura ....................................................8 2. Pleurisy ........................................................................................................9 2.1. Morphology ..................................................................................................9 2.2. Prevalence ..................................................................................................11 -

Chest Pain in Pediatrics
PEDIATRIC CARDIOLOGY 0031-3955/99 $8.00 + .OO CHEST PAIN IN PEDIATRICS Keith C. Kocis, MD, MS Chest pain is an alarming complaint in children, leading an often frightened and concerned family to a pediatrician or emergency room and commonly to a subsequent referral to a pediatric cardiologist. Because of the well-known associ- ation of chest pain with significant cardiovascular disease and sudden death in adult patients, medical personnel commonly share heightened concerns over pediatric patients presenting with chest pain. Although the differential diagnosis of chest pain is exhaustive, chest pain in children is least likely to be cardiac in origin. Organ systems responsible for causing chest pain in children include*: Idiopathic (12%-85%) Musculoskeletal (15%-31%) Pulmonary (12%-21%) Other (4%-21%) Psychiatric (5%-17%) Gastrointestinal (4'/0-7%) Cardiac (4%4%) Furthermore, chest pain in the pediatric population is rareZy associated with life-threatening disease; however, when present, prompt recognition, diagnostic evaluation, and intervention are necessary to prevent an adverse outcome. This article presents a comprehensive list of differential diagnostic possibilities of chest pain in pediatric patients, discusses the common causes in further detail, and outlines a rational diagnostic evaluation and treatment plan. Chest pain, a common complaint of pediatric patients, is often idiopathic in etiology and commonly chronic in nature. In one study,67 chest pain accounted for 6 in 1000 visits to an urban pediatric emergency room. In addition, chest pain is the second most common reason for referral to pediatric cardiologist^.^, 23, 78 Chest pain is found equally in male and female patients, with an average *References 13, 17, 23, 27, 32, 35, 44, 48, 49, 63-67, 74, and 78. -

What Is Pertussis (Whooping Cough)?
American Thoracic Society PATIENT EDUCATION | INFORMATION SERIES What Is Pertussis (Whooping Cough)? Pertussis is a very contagious respiratory infection commonly known as ‘whooping cough’. It is caused by a bacterium called Bordetella pertussis. The infection became much less common after a successful vaccine was developed and given to children to help prevent infection. However, in recent years, the number of people infected with pertussis has increased and now is at the highest rate seen since the 1950’s. There is concern that this is due mainly to people not taking the pertussis (whooping cough) vaccination and adults who have not had a booster and their immune protection has weakened with age. Whooping cough usually starts as a mild cold-like illness get in the air. If you are close enough, you can breathe in these (upper respiratory infection). The pertussis bacteria enter the droplets or they can land on your mouth, nose, or eye. You lungs and cause swelling and irritation in the airways leading can also get the infection if you kiss the face of a person with to severe coughing fits. At times, people with whooping pertussis or get infected nose or mouth secretions on your cough can have a secondary pneumonia from other bacteria hands and then touch your own face to rub your eyes or nose. while they are ill. Whooping cough can cause very serious A person with pertussis can remain contagious for many weeks illness. It is most dangerous in young babies and can result unless treated with an antibiotic. in death. It spreads very easily and people who have the infection can still spread it to others for weeks after they What are the symptoms of Pertussis infection? become sick. -
Gas Exchange and Respiratory Function
LWBK330-4183G-c21_p484-516.qxd 23/07/2009 02:09 PM Page 484 Aptara Gas Exchange and 5 Respiratory Function Applying Concepts From NANDA, NIC, • Case Study and NOC A Patient With Impaired Cough Reflex Mrs. Lewis, age 77 years, is admitted to the hospital for left lower lobe pneumonia. Her vital signs are: Temp 100.6°F; HR 90 and regular; B/P: 142/74; Resp. 28. She has a weak cough, diminished breath sounds over the lower left lung field, and coarse rhonchi over the midtracheal area. She can expectorate some sputum, which is thick and grayish green. She has a history of stroke. Secondary to the stroke she has impaired gag and cough reflexes and mild weakness of her left side. She is allowed food and fluids because she can swallow safely if she uses the chin-tuck maneuver. Visit thePoint to view a concept map that illustrates the relationships that exist between the nursing diagnoses, interventions, and outcomes for the patient’s clinical problems. LWBK330-4183G-c21_p484-516.qxd 23/07/2009 02:09 PM Page 485 Aptara Nursing Classifications and Languages NANDA NIC NOC NURSING DIAGNOSES NURSING INTERVENTIONS NURSING OUTCOMES INEFFECTIVE AIRWAY CLEARANCE— RESPIRATORY MONITORING— Return to functional baseline sta- Inability to clear secretions or ob- Collection and analysis of patient tus, stabilization of, or structions from the respiratory data to ensure airway patency improvement in: tract to maintain a clear airway and adequate gas exchange RESPIRATORY STATUS: AIRWAY PATENCY—Extent to which the tracheobronchial passages remain open IMPAIRED GAS -

Subset of Alphabetical Index to Diseases and Nature of Injury for Use with Perinatal Conditions (P00-P96)
Subset of alphabetical index to diseases and nature of injury for use with perinatal conditions (P00-P96) SUBSET OF ALPHABETICAL INDEX TO DISEASES AND NATURE OF INJURY FOR USE WITH PERINATAL CONDITIONS (P00-P96) Conditions arising in the perinatal period Conditions arising—continued - abnormal, abnormality—continued Note - Conditions arising in the perinatal - - fetus, fetal period, even though death or morbidity - - - causing disproportion occurs later, should, as far as possible, be - - - - affecting fetus or newborn P03.1 coded to chapter XVI, which takes - - forces of labor precedence over chapters containing codes - - - affecting fetus or newborn P03.6 for diseases by their anatomical site. - - labor NEC - - - affecting fetus or newborn P03.6 These exclude: - - membranes (fetal) Congenital malformations, deformations - - - affecting fetus or newborn P02.9 and chromosomal abnormalities - - - specified type NEC, affecting fetus or (Q00-Q99) newborn P02.8 Endocrine, nutritional and metabolic - - organs or tissues of maternal pelvis diseases (E00-E99) - - - in pregnancy or childbirth Injury, poisoning and certain other - - - - affecting fetus or newborn P03.8 consequences of external causes (S00-T99) - - - - causing obstructed labor Neoplasms (C00-D48) - - - - - affecting fetus or newborn P03.1 Tetanus neonatorum (A33) - - parturition - - - affecting fetus or newborn P03.9 - ablatio, ablation - - presentation (fetus) (see also Presentation, - - placentae (see also Abruptio placentae) fetal, abnormal) - - - affecting fetus or newborn -

Chest Auscultation: Presence/Absence and Equality of Normal/Abnormal and Adventitious Breath Sounds and Heart Sounds A
Northwest Community EMS System Continuing Education: January 2012 RESPIRATORY ASSESSMENT Independent Study Materials Connie J. Mattera, M.S., R.N., EMT-P COGNITIVE OBJECTIVES Upon completion of the class, independent study materials and post-test question bank, each participant will independently do the following with a degree of accuracy that meets or exceeds the standards established for their scope of practice: 1. Integrate complex knowledge of pulmonary anatomy, physiology, & pathophysiology to sequence the steps of an organized physical exam using four maneuvers of assessment (inspection, palpation, percussion, and auscultation) and appropriate technique for patients of all ages. (National EMS Education Standards) 2. Integrate assessment findings in pts who present w/ respiratory distress to form an accurate field impression. This includes developing a list of differential diagnoses using higher order thinking and critical reasoning. (National EMS Education Standards) 3. Describe the signs and symptoms of compromised ventilations/inadequate gas exchange. 4. Recognize the three immediate life-threatening thoracic injuries that must be detected and resuscitated during the “B” portion of the primary assessment. 5. Explain the difference between pulse oximetry and capnography monitoring and the type of information that can be obtained from each of them. 6. Compare and contrast those patients who need supplemental oxygen and those that would be harmed by hyperoxia, giving an explanation of the risks associated with each. 7. Select the correct oxygen delivery device and liter flow to support ventilations and oxygenation in a patient with ventilatory distress, impaired gas exchange or ineffective breathing patterns including those patients who benefit from CPAP. 8. Explain the components to obtain when assessing a patient history using SAMPLE and OPQRST. -

Evaluation of Upper Airway Changes Following Surgical Removal of the Adenoids Using 3-D Cone Beam CT
University of Nebraska Medical Center DigitalCommons@UNMC Theses & Dissertations Graduate Studies Fall 12-18-2015 Evaluation of Upper Airway Changes Following Surgical Removal of the Adenoids Using 3-D Cone Beam CT Christopher C. Schultz University of Nebraska Medical Center Follow this and additional works at: https://digitalcommons.unmc.edu/etd Part of the Other Medical Specialties Commons Recommended Citation Schultz, Christopher C., "Evaluation of Upper Airway Changes Following Surgical Removal of the Adenoids Using 3-D Cone Beam CT" (2015). Theses & Dissertations. 54. https://digitalcommons.unmc.edu/etd/54 This Thesis is brought to you for free and open access by the Graduate Studies at DigitalCommons@UNMC. It has been accepted for inclusion in Theses & Dissertations by an authorized administrator of DigitalCommons@UNMC. For more information, please contact [email protected]. EVALUATION OF UPPER AIRWAY CHANGES FOLLOWING SURGICAL REMOVAL OF THE ADENOIDS USING 3-D CONE BEAM CT By Christopher C. Schultz, D.D.S A THESIS Presented to the Faculty of The Graduate College in the University of Nebraska In Partial Fulfillment of Requirements For the Degree of Master of Science Medical Sciences Interdepartmental Area Oral Biology University of Nebraska Medical Center Omaha, Nebraska December, 2015 Advisory Committee: Sundaralingam Premaraj, BDS, MS, PhD, FRCD(C) Sheela Premaraj, BDS, PhD Peter J. Giannini, DDS, MS Stanton D. Harn, PhD i ACKNOWLEDGEMENTS I would like to express my thanks and gratitude to the members of my thesis committee: Dr. Sundaralingam Premaraj, Dr. Sheela Premaraj, Dr. Peter Giannini, and Dr. Stanton Harn. Your advice and assistance has been vital for the completion of the project. -

Community-Acquired Pneumonia in Adults: Diagnostic Reliability of Physical Examination Techniques and Their Teaching in Academia
James Madison University JMU Scholarly Commons Physician Assistant Capstones The Graduate School Fall 12-14-2018 Community-acquired pneumonia in adults: Diagnostic reliability of physical examination techniques and their teaching in academia Amber Tordoff James Madison University Lauren A. Williams James Madison University Follow this and additional works at: https://commons.lib.jmu.edu/pacapstones Part of the Bacteria Commons, Bacterial Infections and Mycoses Commons, Diagnosis Commons, Investigative Techniques Commons, Medical Pathology Commons, Respiratory Tract Diseases Commons, Virus Diseases Commons, and the Viruses Commons Recommended Citation Tordoff AL, Williams LA. Community-Acquired Pneumonia in Adults: Diagnostic Reliability of Physical Examination Techniques and their Teaching in Academia. JMU Scholarly Commons Physician Assistant Capstones. https://commons.lib.jmu.edu/pacapstones/44/. Published December 12, 2018. This Presentation is brought to you for free and open access by the The Graduate School at JMU Scholarly Commons. It has been accepted for inclusion in Physician Assistant Capstones by an authorized administrator of JMU Scholarly Commons. For more information, please contact [email protected]. Community-Acquired Pneumonia in Adults: Diagnostic Reliability of Physical Examination Techniques and their Teaching in Academia Amber Tordoff, PA-S and Lauren Williams, PA-S, James Madison University, Harrisonburg, Virginia _____________________________________________________________________________________ ABSTRACT Background: