Alterations in the Epithelial Stem Cell Compartment Could Contribute
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -
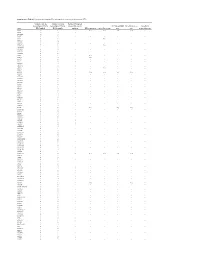
Supplementary Table S1. Prioritization of Candidate FPC Susceptibility Genes by Private Heterozygous Ptvs
Supplementary Table S1. Prioritization of candidate FPC susceptibility genes by private heterozygous PTVs Number of private Number of private Number FPC patient heterozygous PTVs in heterozygous PTVs in tumors with somatic FPC susceptibility Hereditary cancer Hereditary Gene FPC kindred BCCS samples mutation DNA repair gene Cancer driver gene gene gene pancreatitis gene ATM 19 1 - Yes Yes Yes Yes - SSPO 12 8 1 - - - - - DNAH14 10 3 - - - - - - CD36 9 3 - - - - - - TET2 9 1 - - Yes - - - MUC16 8 14 - - - - - - DNHD1 7 4 1 - - - - - DNMT3A 7 1 - - Yes - - - PKHD1L1 7 9 - - - - - - DNAH3 6 5 - - - - - - MYH7B 6 1 - - - - - - PKD1L2 6 6 - - - - - - POLN 6 2 - Yes - - - - POLQ 6 7 - Yes - - - - RP1L1 6 6 - - - - - - TTN 6 5 4 - - - - - WDR87 6 7 - - - - - - ABCA13 5 3 1 - - - - - ASXL1 5 1 - - Yes - - - BBS10 5 0 - - - - - - BRCA2 5 6 1 Yes Yes Yes Yes - CENPJ 5 1 - - - - - - CEP290 5 5 - - - - - - CYP3A5 5 2 - - - - - - DNAH12 5 6 - - - - - - DNAH6 5 1 1 - - - - - EPPK1 5 4 - - - - - - ESYT3 5 1 - - - - - - FRAS1 5 4 - - - - - - HGC6.3 5 0 - - - - - - IGFN1 5 5 - - - - - - KCP 5 4 - - - - - - LRRC43 5 0 - - - - - - MCTP2 5 1 - - - - - - MPO 5 1 - - - - - - MUC4 5 5 - - - - - - OBSCN 5 8 2 - - - - - PALB2 5 0 - Yes - Yes Yes - SLCO1B3 5 2 - - - - - - SYT15 5 3 - - - - - - XIRP2 5 3 1 - - - - - ZNF266 5 2 - - - - - - ZNF530 5 1 - - - - - - ACACB 4 1 1 - - - - - ALS2CL 4 2 - - - - - - AMER3 4 0 2 - - - - - ANKRD35 4 4 - - - - - - ATP10B 4 1 - - - - - - ATP8B3 4 6 - - - - - - C10orf95 4 0 - - - - - - C2orf88 4 0 - - - - - - C5orf42 4 2 - - - - -

Copy Number Variation in Fetal Alcohol Spectrum Disorder
Biochemistry and Cell Biology Copy number variation in fetal alcohol spectrum disorder Journal: Biochemistry and Cell Biology Manuscript ID bcb-2017-0241.R1 Manuscript Type: Article Date Submitted by the Author: 09-Nov-2017 Complete List of Authors: Zarrei, Mehdi; The Centre for Applied Genomics Hicks, Geoffrey G.; University of Manitoba College of Medicine, Regenerative Medicine Reynolds, James N.; Queen's University School of Medicine, Biomedical and Molecular SciencesDraft Thiruvahindrapuram, Bhooma; The Centre for Applied Genomics Engchuan, Worrawat; Hospital for Sick Children SickKids Learning Institute Pind, Molly; University of Manitoba College of Medicine, Regenerative Medicine Lamoureux, Sylvia; The Centre for Applied Genomics Wei, John; The Centre for Applied Genomics Wang, Zhouzhi; The Centre for Applied Genomics Marshall, Christian R.; The Centre for Applied Genomics Wintle, Richard; The Centre for Applied Genomics Chudley, Albert; University of Manitoba Scherer, Stephen W.; The Centre for Applied Genomics Is the invited manuscript for consideration in a Special Fetal Alcohol Spectrum Disorder Issue? : Keyword: Fetal alcohol spectrum disorder, FASD, copy number variations, CNV https://mc06.manuscriptcentral.com/bcb-pubs Page 1 of 354 Biochemistry and Cell Biology 1 Copy number variation in fetal alcohol spectrum disorder 2 Mehdi Zarrei,a Geoffrey G. Hicks,b James N. Reynolds,c,d Bhooma Thiruvahindrapuram,a 3 Worrawat Engchuan,a Molly Pind,b Sylvia Lamoureux,a John Wei,a Zhouzhi Wang,a Christian R. 4 Marshall,a Richard F. Wintle,a Albert E. Chudleye,f and Stephen W. Scherer,a,g 5 aThe Centre for Applied Genomics and Program in Genetics and Genome Biology, The Hospital 6 for Sick Children, Toronto, Ontario, Canada 7 bRegenerative Medicine Program, University of Manitoba, Winnipeg, Canada 8 cCentre for Neuroscience Studies, Queen's University, Kingston, Ontario, Canada. -

Plasma Membrane Ion Channels and Epithelial to Mesenchymal Transition in Cancer Cells
2311 I Azimi and G R Monteith Ion channels and EMT 23:11 R517–R525 Review in cancer Plasma membrane ion channels and epithelial to mesenchymal transition in cancer cells Iman Azimi1,2,3 and Gregory R Monteith1,2,3 Correspondence should be addressed 1 The School of Pharmacy, The University of Queensland, Brisbane, Queensland, Australia to G R Monteith 2 Mater Research Institute, The University of Queensland, Brisbane, Queensland, Australia Email 3 Translational Research Institute, Brisbane, Queensland, Australia [email protected] Abstract A variety of studies have suggested that epithelial to mesenchymal transition (EMT) Key Words may be important in the progression of cancer in patients through metastasis and/or f calcium therapeutic resistance. A number of pathways have been investigated in EMT in cancer f cell signalling cells. Recently, changes in plasma membrane ion channel expression as a consequence f intracellular signalling of EMT have been reported. Other studies have identified specific ion channels able to f metastasis regulate aspects of EMT induction. The utility of plasma membrane ion channels as targets for pharmacological modulation make them attractive for therapeutic approaches to target EMT. In this review, we provide an overview of some of the key plasma membrane ion channel types and highlight some of the studies that are beginning to define changes in plasma membrane ion channels as a consequence of EMT and also their possible roles in Endocrine-Related Cancer Endocrine-Related Cancer Endocrine-Related EMT induction. (2016) 23, R517–R525 Introduction Epithelial to mesenchymal transition (EMT) refers to the treatment of the primary tumour are often feasible process whereby epithelial cells which typically exhibit (e.g. -

Appendix 2. Significantly Differentially Regulated Genes in Term Compared with Second Trimester Amniotic Fluid Supernatant
Appendix 2. Significantly Differentially Regulated Genes in Term Compared With Second Trimester Amniotic Fluid Supernatant Fold Change in term vs second trimester Amniotic Affymetrix Duplicate Fluid Probe ID probes Symbol Entrez Gene Name 1019.9 217059_at D MUC7 mucin 7, secreted 424.5 211735_x_at D SFTPC surfactant protein C 416.2 206835_at STATH statherin 363.4 214387_x_at D SFTPC surfactant protein C 295.5 205982_x_at D SFTPC surfactant protein C 288.7 1553454_at RPTN repetin solute carrier family 34 (sodium 251.3 204124_at SLC34A2 phosphate), member 2 238.9 206786_at HTN3 histatin 3 161.5 220191_at GKN1 gastrokine 1 152.7 223678_s_at D SFTPA2 surfactant protein A2 130.9 207430_s_at D MSMB microseminoprotein, beta- 99.0 214199_at SFTPD surfactant protein D major histocompatibility complex, class II, 96.5 210982_s_at D HLA-DRA DR alpha 96.5 221133_s_at D CLDN18 claudin 18 94.4 238222_at GKN2 gastrokine 2 93.7 1557961_s_at D LOC100127983 uncharacterized LOC100127983 93.1 229584_at LRRK2 leucine-rich repeat kinase 2 HOXD cluster antisense RNA 1 (non- 88.6 242042_s_at D HOXD-AS1 protein coding) 86.0 205569_at LAMP3 lysosomal-associated membrane protein 3 85.4 232698_at BPIFB2 BPI fold containing family B, member 2 84.4 205979_at SCGB2A1 secretoglobin, family 2A, member 1 84.3 230469_at RTKN2 rhotekin 2 82.2 204130_at HSD11B2 hydroxysteroid (11-beta) dehydrogenase 2 81.9 222242_s_at KLK5 kallikrein-related peptidase 5 77.0 237281_at AKAP14 A kinase (PRKA) anchor protein 14 76.7 1553602_at MUCL1 mucin-like 1 76.3 216359_at D MUC7 mucin 7, -
Microarray Analysis Reveals the Inhibition of Intestinal Expression Of
www.nature.com/scientificreports OPEN Microarray analysis reveals the inhibition of intestinal expression of nutrient transporters in piglets infected with porcine epidemic diarrhea virus Junmei Zhang1,3, Di Zhao1,3, Dan Yi1,3, Mengjun Wu1, Hongbo Chen1, Tao Wu1, Jia Zhou1, Peng Li1, Yongqing Hou1* & Guoyao Wu2 Porcine epidemic diarrhea virus (PEDV) infection can induce intestinal dysfunction, resulting in severe diarrhea and even death, but the mode of action underlying these viral efects remains unclear. This study determined the efects of PEDV infection on intestinal absorption and the expression of genes for nutrient transporters via biochemical tests and microarray analysis. Sixteen 7-day-old healthy piglets fed a milk replacer were randomly allocated to one of two groups. After 5-day adaption, piglets (n = 8/ group) were orally administrated with either sterile saline or PEDV (the strain from Yunnan province) 4.5 at 10 TCID50 (50% tissue culture infectious dose) per pig. All pigs were orally infused D-xylose (0.1 g/ kg BW) on day 5 post PEDV or saline administration. One hour later, jugular vein blood samples as well as intestinal samples were collected for further analysis. In comparison with the control group, PEDV infection increased diarrhea incidence, blood diamine oxidase activity, and iFABP level, while reducing growth and plasma D-xylose concentration in piglets. Moreover, PEDV infection altered plasma and jejunal amino acid profles, and decreased the expression of aquaporins and amino acid transporters (L-type amino acid -

CLCA4 Inhibits Bladder Cancer Cell Proliferation, Migration, and Invasion by Suppressing the PI3K/AKT Pathway
www.impactjournals.com/oncotarget/ Oncotarget, 2017, Vol. 8, (No. 54), pp: 93001-93013 Research Paper CLCA4 inhibits bladder cancer cell proliferation, migration, and invasion by suppressing the PI3K/AKT pathway Teng Hou1,*, Lijie Zhou1,*, Longwang Wang1,2, Gallina Kazobinka1, Xiaoping Zhang1 and Zhaohui Chen1 1Department of Urology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan 430022, China 2Department of Urology, The Second Affiliated Hospital of Nanchang University, Nanchang, Jiangxi 330008, China *These authors have contributed equally to this work Correspondence to: Zhaohui Chen, email: [email protected] Keywords: CLCA4, bladder cancer, PI3K/Akt, proliferation, metastasis Received: July 21, 2017 Accepted: August 17, 2017 Published: October 09, 2017 Copyright: Hou et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License 3.0 (CC BY 3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. ABSTRACT Calcium activated chloride channel A4 (CLCA4), a tumor suppressor, was shown to contribute to the progression of several human cancers, while its role in bladder carcinoma remains unclear. In this study, we showed CLCA4 expression was down- regulated in bladder carcinoma tissues and cells compared to adjacent non-tumor tissues and normal urothelial cells. Low CLCA4 expression was correlated with larger tumor size, advanced tumor stage, and poor prognosis in bladder carcinoma patients. Overexpression of CLCA4 profoundly attenuated the proliferation, growth, migratory and invasive capabilities of bladder cancer cells, whereas CLCA4 knockdown had the opposite effect. Mechanistically, CLCA4 is involved in PI3K/AKT signaling and its downstream molecules can promote bladder cancer cell proliferation. -

Clinical, Molecular, and Immune Analysis of Dabrafenib-Trametinib
Supplementary Online Content Chen G, McQuade JL, Panka DJ, et al. Clinical, molecular and immune analysis of dabrafenib-trametinib combination treatment for metastatic melanoma that progressed during BRAF inhibitor monotherapy: a phase 2 clinical trial. JAMA Oncology. Published online April 28, 2016. doi:10.1001/jamaoncol.2016.0509. eMethods. eReferences. eTable 1. Clinical efficacy eTable 2. Adverse events eTable 3. Correlation of baseline patient characteristics with treatment outcomes eTable 4. Patient responses and baseline IHC results eFigure 1. Kaplan-Meier analysis of overall survival eFigure 2. Correlation between IHC and RNAseq results eFigure 3. pPRAS40 expression and PFS eFigure 4. Baseline and treatment-induced changes in immune infiltrates eFigure 5. PD-L1 expression eTable 5. Nonsynonymous mutations detected by WES in baseline tumors This supplementary material has been provided by the authors to give readers additional information about their work. © 2016 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 09/30/2021 eMethods Whole exome sequencing Whole exome capture libraries for both tumor and normal samples were constructed using 100ng genomic DNA input and following the protocol as described by Fisher et al.,3 with the following adapter modification: Illumina paired end adapters were replaced with palindromic forked adapters with unique 8 base index sequences embedded within the adapter. In-solution hybrid selection was performed using the Illumina Rapid Capture Exome enrichment kit with 38Mb target territory (29Mb baited). The targeted region includes 98.3% of the intervals in the Refseq exome database. Dual-indexed libraries were pooled into groups of up to 96 samples prior to hybridization. -

SNX10 and PTGDS Are Associated with the Progression and Prognosis of Cervical Squamous Cell Carcinoma
SNX10 and PTGDS are Associated with the Progression and Prognosis of Cervical Squamous Cell Carcinoma Pinping Jiang Nanjing Medical University Ying Cao Nanjing Medical University Feng Gao Nanjing Medical University Wei Sun Nanjing Medical University Jinhui Liu Nanjing Medical University Ziyan Ma University of New South Wales Manxin Xie Nanjing Medical University Shilong Fu ( [email protected] ) Jiangsu Province Hospital and Nanjing Medical University First Aliated Hospital https://orcid.org/0000-0001-7416-3070 Research article Keywords: Cervical squamous cell carcinoma, methylation, prognosis, risk model, SNX10, PTGDS Posted Date: October 12th, 2020 DOI: https://doi.org/10.21203/rs.3.rs-50778/v2 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/25 Abstract Background: Cervical cancer (CC) is the primary cause of death in women. This study sought to investigate the potential mechanism and prognostic genes of CC. Methods: We downloaded four gene expression proles from GEO. The RRA method was used to integrate and screen differentially expressed genes (DEGs) between CC and normal samples. Functional analysis was performed by clusterproler. We built PPI network by Search Tool for the Retrieval of Interacting Genes Database (STRING) and selected hub modules via Molecular COmplex Detection (MCODE). CMap database was used to nd molecules with therapeutic potential for CC. The hub genes were validated in GEO datasets, Gene Expession Proling Interactive Analysis (GEPIA), immunohistochemistry, Cox regression analysis, TCGA methylation analysis and ONCOMINE were carried out. ROC curve analysis and GSEA were also performed to describe the prognostic signicance of hub genes. -

SNX10 and PTGDS Are Associated with the Progression and Prognosis
Jiang et al. BMC Cancer (2021) 21:694 https://doi.org/10.1186/s12885-021-08212-w RESEARCH ARTICLE Open Access SNX10 and PTGDS are associated with the progression and prognosis of cervical squamous cell carcinoma Pinping Jiang1†, Ying Cao2†, Feng Gao3†, Wei Sun1, Jinhui Liu1, Ziyan Ma4, Manxin Xie1* and Shilong Fu1* Abstract Background: Cervical cancer (CC) is the primary cause of death in women. This study sought to investigate the potential mechanism and prognostic genes of CC. Methods: We downloaded four gene expression profiles from GEO. The RRA method was used to integrate and screen differentially expressed genes (DEGs) between CC and normal samples. Functional analysis was performed by clusterprofiler. We built PPI network by Search Tool for the Retrieval of Interacting Genes Database (STRING) and selected hub modules via Molecular COmplex Detection (MCODE). CMap database was used to find molecules with therapeutic potential for CC. The hub genes were validated in GEO datasets, Gene Expession Profiling Interactive Analysis (GEPIA), immunohistochemistry, Cox regression analysis, TCGA methylation analysis and ONCOMINE were carried out. ROC curve analysis and GSEA were also performed to describe the prognostic significance of hub genes. Results: Functional analysis revealed that 147 DEGs were significantly enriched in binding, cell proliferation, transcriptional activity and cell cycle regulation. PPI network screened 30 hub genes, with CDK1 having the strongest connectivity with CC. Cmap showed that apigenin, thioguanine and trichostatin A might be used to treat CC(P < 0.05). Eight genes (APOD, CXCL8, MMP1, MMP3, PLOD2, PTGDS, SNX10 and SPP1) were screened out through GEPIA. Of them, only PTGDS and SNX10 had not appeared in previous studies about CC. -

Infection Defense Against Bacterial Urinary Tract Pathways and Rapid
Downloaded from http://www.jimmunol.org/ by guest on October 2, 2021 is online at: average * Drive Diverse Biological The Journal of Immunology , 27 of which you can access for free at: 2012; 188:781-792; Prepublished online 19 from submission to initial decision 4 weeks from acceptance to publication Benjamin L. Duell, Alison J. Carey, Chee K. Tan, Xiangqin Cui, Richard I. Webb, Makrina Totsika, Mark A. Schembri, Petra Derrington, Helen Irving-Rodgers, Andrew J. Brooks, Allan W. Cripps, Michael Crowley and Glen C. Ulett December 2011; doi: 10.4049/jimmunol.1101231 http://www.jimmunol.org/content/188/2/781 Innate Transcriptional Networks Activated in Bladder in Response to Uropathogenic Escherichia coli Pathways and Rapid Synthesis of IL-10 for Defense against Bacterial Urinary Tract Infection J Immunol cites 82 articles Submit online. Every submission reviewed by practicing scientists ? is published twice each month by http://jimmunol.org/subscription Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts http://www.jimmunol.org/content/188/2/781.full#ref-list-1 http://www.jimmunol.org/content/suppl/2011/12/19/jimmunol.110123 1.DC1 This article Information about subscribing to The JI No Triage! Fast Publication! Rapid Reviews! 30 days* Why • • • Material References Permissions Email Alerts Subscription Supplementary The Journal of Immunology The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2012 by The American Association of Immunologists, Inc. All rights reserved. -

Calcium-Activated Chloride Channel Regulator 1 As A
Hu et al. BMC Cancer (2018) 18:1096 https://doi.org/10.1186/s12885-018-5013-2 RESEARCH ARTICLE Open Access Calcium-activated chloride channel regulator 1 as a prognostic biomarker in pancreatic ductal adenocarcinoma Dingyuan Hu1,2, Daniel Ansari1, Qimin Zhou1, Agata Sasor3, Katarzyna Said Hilmersson1, Monika Bauden1, Yi Jiang2 and Roland Andersson1* Abstract Background: In a previous study utilizing mass spectrometry-based proteomics, we identified calcium-activated chloride channel regulator 1 (CLCA1) as a potential tumor suppressor in pancreatic cancer and the expression was inversely correlated with patient survival. The aim of the study was to further validate the prognostic significance of CLCA1 in pancreatic cancer. Methods: CLCA1 expression was evaluated with tissue microarrays and immunohistochemistry in 140 patients with pancreatic ductal adenocarcinoma that underwent surgical resection at Skåne University Hospital, Sweden. Kaplan- Meier and Cox proportional hazards modeling were used to explore the association between CLCA1 and clinicopathological factors and survival. Results: CLCA1 expression was denoted as positive in 90 tumors (64.3%), with positive staining being limited to the tumor cells. There were no significant association between CLCA1 expression and established clinicopathological parameters. Low CLCA1 expression correlated significantly with shorter disease-free survival (11.9 vs 17.5 months, P = 0.042). Multivariable Cox regression analysis confirmed the results (HR 0.61, 95% CI-0.40-0.92, P = 0.019). Conclusions: Low CLCA1 expression is an independent factor of poor disease-free survival in pancreatic cancer. Keywords: Pancreatic ductal adenocarcinoma, CLCA1, Calcium-activated chloride channel regulators, Survival Background and a better prediction of prognosis and treatment Pancreatic ductal adenocarcinoma (PDAC) is currently response.