Gene Networks Constructed Through Simulated Treatment Learning Can Predict Proteasome Inhibitor Benefit in Multiple Myeloma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Application of a Characterized Pre-Clinical
THE APPLICATION OF A CHARACTERIZED PRE-CLINICAL GLIOBLASTOMA ONCOSPHERE MODEL TO IN VITRO AND IN VIVO THERAPEUTIC TESTING by Kelli M. Wilson A dissertation submitted to Johns Hopkins University in conformity with the requirements for the degree of Doctor of Philosophy Baltimore, Maryland March, 2014 ABSTRACT Glioblastoma multiforme (GBM) is a lethal brain cancer with a median survival time (MST) of approximately 15 months following treatment. A serious challenge facing the development of new drugs for the treatment of GBM is that preclinical models fail to replicate the human GBM phenotype. Here we report the Johns Hopkins Oncosphere Panel (JHOP), a panel of GBM oncosphere cell lines. These cell lines were validated by their ability to form tumors intracranially with histological features of human GBM and GBM variant tumors. We then completed whole exome sequencing on JHOP and found that they contain genetic alterations in GBM driver genes such as PTEN, TP53 and CDKN2A. Two JHOP cell lines were utilized in a high throughput drug screen of 466 compounds that were selected to represent late stage clinical development and a wide range of mechanisms. Drugs that were inhibitory in both cell lines were EGFR inhibitors, NF-kB inhibitors and apoptosis activators. We also examined drugs that were inhibitory in a single cell line. Effective drugs in the PTEN null and NF1 wild type cell line showed a limited number of drug targets with EGFR inhibitors being the largest group of cytotoxic compounds. However, in the PTEN mutant, NF1 null cell line, VEGFR/PDGFR inhibitors and dual PIK3/mTOR inhibitors were the most common effective compounds. -

Options for the Treatment of Gemcitabine-Resistant Advanced Pancreatic Cancer
JOP. J Pancreas (Online) 2010 Mar 5; 11(2):113-123. REVIEW Options for the Treatment of Gemcitabine-Resistant Advanced Pancreatic Cancer Ioannis Gounaris, Kamarul Zaki, Pippa Corrie Oncology Centre, Cambridge University Hospitals NHS Trust. Cambridge, United Kingdom Summary Context Pancreatic cancer is noteworthy in that the number of patients dying from the disease is roughly equal to the number diagnosed. For more than a decade, gemcitabine has constituted the standard of care for the palliative treatment of the majority of patients who present with metastatic or relapsed disease, although the survival gains are limited. Despite a median survival of less than 6 months, there is a significant proportion of advanced pancreatic cancer patients who progress on gemcitabine that remains fit and these patients are candidates for second-line treatment. Methods The OVID MEDLINE database was searched from 1950 to present using the MeSH terms “pancreatic neoplasms”, “drug treatment” and “gemcitabine”. After excluding non-relevant results, 31 published studies were identified. These results were supplemented by searching the last three (2007-2009) American Society of Clinical Oncology (ASCO) Proceedings of Annual Meetings for studies published only in abstract form and reviewing reference lists of published articles. Results and discussion The evidence for second line treatments of metastatic pancreatic cancer consists mostly of single arm, small phase II studies. Oxaliplatin-fluoropyrimidine combinations appear promising and have shown increased survival compared to best supportive care. As the molecular pathways governing pancreatic cancer are unravelled, novel targeted therapies may offer the greatest promise for this disease either given alone, combined with one another, or with cytotoxic agents. -

Age-Dependent Myocardial Transcriptomic Changes in the Rat
Revista Română de Medicină de Laborator Vol. 22, Nr. 1, Martie, 2014 9 Research article DOI: 10.2478/rrlm-2014-0001 Age-dependent myocardial transcriptomic changes in the rat. Novel insights into atrial and ventricular arrhythmias pathogenesis Modificări transcriptomice dependente de vârstă în miocardul de șobolan. Noi aspecte referitoare la patogeneza aritmiilor atriale și ventriculare Alina Scridon1,2, Emmanuelle Fouilloux-Meugnier3, Emmanuelle Loizon3, Marcel Perian1, Sophie Rome3, Claude Julien2, Christian Barrès2, Philippe Chevalier2,4 1.Physiology Department, University of Medicine and Pharmacy of Tîrgu Mureș, 540139, Tîrgu Mureș, Romania 2. Unité de Neurocardiologie, EA4612, Université Lyon 1, F-69008, Lyon, France 3. Unité 1060 INSERM CarMen, Université Lyon 1, F-69008, Lyon, France 4. Hospices Civils de Lyon, Hôpital Louis Pradel, Service de Rythmologie, 69500, Bron, France Abstract Background: Aging is associated with significantly increased prevalence of cardiac arrhythmias, but tran- scriptional events that underlie this process remain to be established. To gain deeper insight into molecular mech- anisms of aging-related cardiac arrhythmias, we performed mRNA expression analysis comparing atrial and ven- tricular myocardium from Wistar-Kyoto (WKY) rats of different ages. Methods: Atrial and ventricular sampling was performed in 3 groups (n=4 each) of young (14-week-old), adult (25-week-old), and aging (47-week-old) WKY rats. mRNA expressions of 89 genes involved in cardiac arrhythmogenicity were investigated using TaqMan Low Density Array analysis. Results: Of the 89 studied genes, 40 and 64 genes presented steady atrial and ventricu- lar expressions, respectively. All genes differentially expressed within the atria of WKY rats were up-regulated with advancing age, mainly the genes encoding for various K+, Ca2+, Na+ channels, and type 6 collagen. -

Regulation of Cdc42 and Its Effectors in Epithelial Morphogenesis Franck Pichaud1,2,*, Rhian F
© 2019. Published by The Company of Biologists Ltd | Journal of Cell Science (2019) 132, jcs217869. doi:10.1242/jcs.217869 REVIEW SUBJECT COLLECTION: ADHESION Regulation of Cdc42 and its effectors in epithelial morphogenesis Franck Pichaud1,2,*, Rhian F. Walther1 and Francisca Nunes de Almeida1 ABSTRACT An overview of Cdc42 Cdc42 – a member of the small Rho GTPase family – regulates cell Cdc42 was discovered in yeast and belongs to a large family of small – polarity across organisms from yeast to humans. It is an essential (20 30 kDa) GTP-binding proteins (Adams et al., 1990; Johnson regulator of polarized morphogenesis in epithelial cells, through and Pringle, 1990). It is part of the Ras-homologous Rho subfamily coordination of apical membrane morphogenesis, lumen formation and of GTPases, of which there are 20 members in humans, including junction maturation. In parallel, work in yeast and Caenorhabditis elegans the RhoA and Rac GTPases, (Hall, 2012). Rho, Rac and Cdc42 has provided important clues as to how this molecular switch can homologues are found in all eukaryotes, except for plants, which do generate and regulate polarity through localized activation or inhibition, not have a clear homologue for Cdc42. Together, the function of and cytoskeleton regulation. Recent studies have revealed how Rho GTPases influences most, if not all, cellular processes. important and complex these regulations can be during epithelial In the early 1990s, seminal work from Alan Hall and his morphogenesis. This complexity is mirrored by the fact that Cdc42 can collaborators identified Rho, Rac and Cdc42 as main regulators of exert its function through many effector proteins. -

The Mineralocorticoid Receptor Leads to Increased Expression of EGFR
www.nature.com/scientificreports OPEN The mineralocorticoid receptor leads to increased expression of EGFR and T‑type calcium channels that support HL‑1 cell hypertrophy Katharina Stroedecke1,2, Sandra Meinel1,2, Fritz Markwardt1, Udo Kloeckner1, Nicole Straetz1, Katja Quarch1, Barbara Schreier1, Michael Kopf1, Michael Gekle1 & Claudia Grossmann1* The EGF receptor (EGFR) has been extensively studied in tumor biology and recently a role in cardiovascular pathophysiology was suggested. The mineralocorticoid receptor (MR) is an important efector of the renin–angiotensin–aldosterone‑system and elicits pathophysiological efects in the cardiovascular system; however, the underlying molecular mechanisms are unclear. Our aim was to investigate the importance of EGFR for MR‑mediated cardiovascular pathophysiology because MR is known to induce EGFR expression. We identifed a SNP within the EGFR promoter that modulates MR‑induced EGFR expression. In RNA‑sequencing and qPCR experiments in heart tissue of EGFR KO and WT mice, changes in EGFR abundance led to diferential expression of cardiac ion channels, especially of the T‑type calcium channel CACNA1H. Accordingly, CACNA1H expression was increased in WT mice after in vivo MR activation by aldosterone but not in respective EGFR KO mice. Aldosterone‑ and EGF‑responsiveness of CACNA1H expression was confrmed in HL‑1 cells by Western blot and by measuring peak current density of T‑type calcium channels. Aldosterone‑induced CACNA1H protein expression could be abrogated by the EGFR inhibitor AG1478. Furthermore, inhibition of T‑type calcium channels with mibefradil or ML218 reduced diameter, volume and BNP levels in HL‑1 cells. In conclusion the MR regulates EGFR and CACNA1H expression, which has an efect on HL‑1 cell diameter, and the extent of this regulation seems to depend on the SNP‑216 (G/T) genotype. -

Merlin Is a Potent Inhibitor of Glioma Growth
Research Article Merlin Is a Potent Inhibitor of Glioma Growth Ying-Ka Ingar Lau,1 Lucas B. Murray,1 Sean S. Houshmandi,2 Yin Xu,1 David H. Gutmann,2 and Qin Yu1 1Department of Oncological Sciences, Mount Sinai School of Medicine, New York, New York and 2Department of Neurology, Washington University School of Medicine, St. Louis, Missouri Abstract The NF2 gene shares sequence similarity with the members of Neurofibromatosis 2 (NF2) is an inherited cancer syndrome in Band 4.1 superfamily (4, 5). In particular, the NF2 protein, merlin (or schwannomin), most closely resembles proteins of the ezrin- which affected individuals develop nervous system tumors, including schwannomas, meningiomas, and ependymomas. radixin-moesin (ERM) subfamily. Similar to the ERM proteins, The NF2 protein merlin (or schwannomin) is a member of the merlin serves as a linker between transmembrane proteins and the Band 4.1superfamily of proteins, which serve as linkers actin cytoskeleton and regulates cytoskeleton remodeling and cell between transmembrane proteins and the actin cytoskeleton. motility (6–8). Unlike ERM proteins, merlin functions as a negative In addition to mutational inactivation of the NF2 gene in NF2- growth regulator or tumor suppressor. In this regard, mutational associated tumors, mutations and loss of merlin expression inactivation of the NF2 gene is sufficient to result in the have also been reported in other types of cancers. In the development of NF2-associated nervous system tumors. Moreover, present study, we show that merlin expression is dramatically NF2 mutations have also been reported in other tumor types, reduced in human malignant gliomas and that reexpression of including melanoma and mesothelioma (9), suggesting that merlin plays an important role, not only in NF2-associated tumors but also functional merlin dramatically inhibits both subcutaneous and intracranial growth of human glioma cells in mice. -

ARHGEF7 (B-PIX) Is Required for the Maintenance of Podocyte Architecture and Glomerular Function
BASIC RESEARCH www.jasn.org ARHGEF7 (b-PIX) Is Required for the Maintenance of Podocyte Architecture and Glomerular Function Jun Matsuda, Mirela Maier, Lamine Aoudjit, Cindy Baldwin, and Tomoko Takano Division of Nephrology, McGill University Health Centre, Montreal, Quebec, Canada ABSTRACT Background Previous studies showed that Cdc42, a member of the prototypical Rho family of small GTPases and a regulator of the actin cytoskeleton, is critical for the normal development and health of podocytes. However, upstream regulatory mechanisms for Cdc42 activity in podocytes are largely unknown. Methods We used a proximity-based ligation assay, BioID, to identify guanine nucleotide exchange fac- tors that activate Cdc42 in immortalized human podocytes. We generated podocyte-specificARHGEF7 (commonly known as b-PIX) knockout mice by crossing b-PIX floxed mice with Podocin-Cre mice. Using shRNA, we established cultured mouse podocytes with b-PIX knockdown and their controls. Results We identified b-PIX as a predominant guanine nucleotide exchange factor that interacts with Cdc42 in human podocytes. Podocyte-specific b-PIX knockout mice developed progressive proteinuria and kidney failure with global or segmental glomerulosclerosis in adulthood. Glomerular podocyte density gradually decreased in podocyte-specific b-PIX knockout mice, indicating podocyte loss. Compared with controls, glomeruli from podocyte-specific b-PIX knockout mice and cultured mouse podocytes with b-PIX knockdown exhibited significant reduction in Cdc42 activity. Loss of b-PIX promoted podocyte apoptosis, which was mediated by the reduced activity of the prosurvival transcriptional regulator Yes-associated protein. Conclusions These findings indicate that b-PIX is required for the maintenance of podocyte architecture and glomerular function via Cdc42 and its downstream Yes-associated protein activities. -

Genetic and Epigenetic Variation in the Human Genome
Digital Comprehensive Summaries of Uppsala Dissertations from the Faculty of Medicine 122 Genetic and Epigenetic Variation in the Human Genome Analysis of Phenotypically Normal Individuals and Patients Affected with Brain Tumors CECILIA DE BUSTOS ACTA UNIVERSITATIS UPSALIENSIS ISSN 1651-6206 UPPSALA ISBN 91-554-6490-4 2006 urn:nbn:se:uu:diva-6629 !" #$ % &' !""( ")*&+ , $ , , -$ $ ./ , 0 12 #$ 3 4 $2 5 62 !""(2 7 4 8 $ 7 2 % , -$ 9 : - %,, 3 $ 5 # 2 % 2 &!!2 (; 2 2 :<59 )&=++>=(>)"=>2 7 , $ $ 2 < $ .<9-1 $ .69-1 $ , , 2 #$ $ $ , = $ 2 6 , , $ 3 $ 2 : : 3 ,, $ , -7/? ,, 3 $ $ @ $ $ $ 2 % , = , $ .!A1 3 , , $ B9/&>;C-7/? $3 $ $ 2 : :: +" 3 @ , 9% 3 $ $ !! 2 D$ !"E , !! ,, , $ !! 3 , &>E , 2 #$ $ , !!F2 - ::: $ , , 'G $ 2 D +&2+E , $ 2 : 3 , 3 , !2! 0 '!" . $ 4 69-12 : 3$ $ 4 69- 3 $ $ $ 3 $ 3 $$= -6 = $ . :812 / $ 3 ! 3$$ $ , 2 #$ $ 3 , 3 $ , 2 H $ 3 @ !)" 2 #$, :=:8 $ <9- 69- = $2 / 8 , 9% $ , ,, I)E , $ $ 2 0 $ $ $ 3 , 3 9% $ , 2 "# $ =67 $ % & & -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

A Multistep Bioinformatic Approach Detects Putative Regulatory
BMC Bioinformatics BioMed Central Research article Open Access A multistep bioinformatic approach detects putative regulatory elements in gene promoters Stefania Bortoluzzi1, Alessandro Coppe1, Andrea Bisognin1, Cinzia Pizzi2 and Gian Antonio Danieli*1 Address: 1Department of Biology, University of Padova – Via Bassi 58/B, 35131, Padova, Italy and 2Department of Information Engineering, University of Padova – Via Gradenigo 6/B, 35131, Padova, Italy Email: Stefania Bortoluzzi - [email protected]; Alessandro Coppe - [email protected]; Andrea Bisognin - [email protected]; Cinzia Pizzi - [email protected]; Gian Antonio Danieli* - [email protected] * Corresponding author Published: 18 May 2005 Received: 12 November 2004 Accepted: 18 May 2005 BMC Bioinformatics 2005, 6:121 doi:10.1186/1471-2105-6-121 This article is available from: http://www.biomedcentral.com/1471-2105/6/121 © 2005 Bortoluzzi et al; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Abstract Background: Searching for approximate patterns in large promoter sequences frequently produces an exceedingly high numbers of results. Our aim was to exploit biological knowledge for definition of a sheltered search space and of appropriate search parameters, in order to develop a method for identification of a tractable number of sequence motifs. Results: Novel software (COOP) was developed for extraction of sequence motifs, based on clustering of exact or approximate patterns according to the frequency of their overlapping occurrences. -
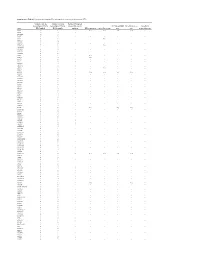
Supplementary Table S1. Prioritization of Candidate FPC Susceptibility Genes by Private Heterozygous Ptvs
Supplementary Table S1. Prioritization of candidate FPC susceptibility genes by private heterozygous PTVs Number of private Number of private Number FPC patient heterozygous PTVs in heterozygous PTVs in tumors with somatic FPC susceptibility Hereditary cancer Hereditary Gene FPC kindred BCCS samples mutation DNA repair gene Cancer driver gene gene gene pancreatitis gene ATM 19 1 - Yes Yes Yes Yes - SSPO 12 8 1 - - - - - DNAH14 10 3 - - - - - - CD36 9 3 - - - - - - TET2 9 1 - - Yes - - - MUC16 8 14 - - - - - - DNHD1 7 4 1 - - - - - DNMT3A 7 1 - - Yes - - - PKHD1L1 7 9 - - - - - - DNAH3 6 5 - - - - - - MYH7B 6 1 - - - - - - PKD1L2 6 6 - - - - - - POLN 6 2 - Yes - - - - POLQ 6 7 - Yes - - - - RP1L1 6 6 - - - - - - TTN 6 5 4 - - - - - WDR87 6 7 - - - - - - ABCA13 5 3 1 - - - - - ASXL1 5 1 - - Yes - - - BBS10 5 0 - - - - - - BRCA2 5 6 1 Yes Yes Yes Yes - CENPJ 5 1 - - - - - - CEP290 5 5 - - - - - - CYP3A5 5 2 - - - - - - DNAH12 5 6 - - - - - - DNAH6 5 1 1 - - - - - EPPK1 5 4 - - - - - - ESYT3 5 1 - - - - - - FRAS1 5 4 - - - - - - HGC6.3 5 0 - - - - - - IGFN1 5 5 - - - - - - KCP 5 4 - - - - - - LRRC43 5 0 - - - - - - MCTP2 5 1 - - - - - - MPO 5 1 - - - - - - MUC4 5 5 - - - - - - OBSCN 5 8 2 - - - - - PALB2 5 0 - Yes - Yes Yes - SLCO1B3 5 2 - - - - - - SYT15 5 3 - - - - - - XIRP2 5 3 1 - - - - - ZNF266 5 2 - - - - - - ZNF530 5 1 - - - - - - ACACB 4 1 1 - - - - - ALS2CL 4 2 - - - - - - AMER3 4 0 2 - - - - - ANKRD35 4 4 - - - - - - ATP10B 4 1 - - - - - - ATP8B3 4 6 - - - - - - C10orf95 4 0 - - - - - - C2orf88 4 0 - - - - - - C5orf42 4 2 - - - - -

Copy Number Variation in Fetal Alcohol Spectrum Disorder
Biochemistry and Cell Biology Copy number variation in fetal alcohol spectrum disorder Journal: Biochemistry and Cell Biology Manuscript ID bcb-2017-0241.R1 Manuscript Type: Article Date Submitted by the Author: 09-Nov-2017 Complete List of Authors: Zarrei, Mehdi; The Centre for Applied Genomics Hicks, Geoffrey G.; University of Manitoba College of Medicine, Regenerative Medicine Reynolds, James N.; Queen's University School of Medicine, Biomedical and Molecular SciencesDraft Thiruvahindrapuram, Bhooma; The Centre for Applied Genomics Engchuan, Worrawat; Hospital for Sick Children SickKids Learning Institute Pind, Molly; University of Manitoba College of Medicine, Regenerative Medicine Lamoureux, Sylvia; The Centre for Applied Genomics Wei, John; The Centre for Applied Genomics Wang, Zhouzhi; The Centre for Applied Genomics Marshall, Christian R.; The Centre for Applied Genomics Wintle, Richard; The Centre for Applied Genomics Chudley, Albert; University of Manitoba Scherer, Stephen W.; The Centre for Applied Genomics Is the invited manuscript for consideration in a Special Fetal Alcohol Spectrum Disorder Issue? : Keyword: Fetal alcohol spectrum disorder, FASD, copy number variations, CNV https://mc06.manuscriptcentral.com/bcb-pubs Page 1 of 354 Biochemistry and Cell Biology 1 Copy number variation in fetal alcohol spectrum disorder 2 Mehdi Zarrei,a Geoffrey G. Hicks,b James N. Reynolds,c,d Bhooma Thiruvahindrapuram,a 3 Worrawat Engchuan,a Molly Pind,b Sylvia Lamoureux,a John Wei,a Zhouzhi Wang,a Christian R. 4 Marshall,a Richard F. Wintle,a Albert E. Chudleye,f and Stephen W. Scherer,a,g 5 aThe Centre for Applied Genomics and Program in Genetics and Genome Biology, The Hospital 6 for Sick Children, Toronto, Ontario, Canada 7 bRegenerative Medicine Program, University of Manitoba, Winnipeg, Canada 8 cCentre for Neuroscience Studies, Queen's University, Kingston, Ontario, Canada.