Gene Networks Constructed Through Simulated Treatment Learning Can
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ncomms2254.Pdf
ARTICLE Received 3 May 2012 | Accepted 5 Nov 2012 | Published 4 Dec 2012 DOI: 10.1038/ncomms2254 The RB family is required for the self-renewal and survival of human embryonic stem cells Jamie F. Conklin1,2,3, Julie Baker2,3 & Julien Sage1,2,3 The mechanisms ensuring the long-term self-renewal of human embryonic stem cells are still only partly understood, limiting their use in cellular therapies. Here we found that increased activity of the RB cell cycle inhibitor in human embryonic stem cells induces cell cycle arrest, differentiation and cell death. Conversely, inactivation of the entire RB family (RB, p107 and p130) in human embryonic stem cells triggers G2/M arrest and cell death through functional activation of the p53 pathway and the cell cycle inhibitor p21. Differences in E2F target gene activation upon loss of RB family function between human embryonic stem cells, mouse embryonic stem cells and human fibroblasts underscore key differences in the cell cycle regulatory networks of human embryonic stem cells. Finally, loss of RB family function pro- motes genomic instability in both human and mouse embryonic stem cells, uncoupling cell cycle defects from chromosomal instability. These experiments indicate that a homeostatic level of RB activity is essential for the self-renewal and the survival of human embryonic stem cells. 1 Department of Pediatrics, Stanford Medical School, Stanford, California 94305, USA. 2 Department of Genetics, Stanford Medical School, Stanford, California 94305, USA. 3 Institute for Stem Cell Biology and Regenerative Medicine, Stanford Medical School, Stanford, California 94305, USA. Correspondence and requests for materials should be addressed to J.S. -

Author Manuscript Faculty of Biology and Medicine Publication
Serveur Académique Lausannois SERVAL serval.unil.ch Author Manuscript Faculty of Biology and Medicine Publication This paper has been peer-reviewed but does not include the final publisher proof-corrections or journal pagination. Published in final edited form as: Title: Sexual dimorphism in cancer. Authors: Clocchiatti A, Cora E, Zhang Y, Dotto GP Journal: Nature reviews. Cancer Year: 2016 May Volume: 16 Issue: 5 Pages: 330-9 DOI: 10.1038/nrc.2016.30 In the absence of a copyright statement, users should assume that standard copyright protection applies, unless the article contains an explicit statement to the contrary. In case of doubt, contact the journal publisher to verify the copyright status of an article. Sexual dimorphism in cancer Andrea Clocchiatti1+, Elisa Cora2+, Yosra Zhang1,2 and G. Paolo Dotto1,2* 1Cutaneous Biology Research Center, Massachusetts General Hospital, Charlestown, MA 02129, USA; 2Department of Biochemistry, University of Lausanne, Epalinges, CH-1066, Switzerland + These authors contributed equally to the work * Corresponding author: G. Paolo Dotto email: [email protected] 1 Abstract The incidence of many cancer types is significantly higher in the male than female populations, with associated differences in survival. Occupational and/or behavioral factors are well known underlying determinants. However, cellular/molecular differences between the two sexes are also likely to be important. We are focusing here on the complex interplay that sexual hormones and sex chromosomes can have in intrinsic control of cancer initiating cell populations, tumor microenvironment and systemic determinants of cancer development like the immune system and metabolism. A better appreciation of these differences between the two sexes could be of substantial value for cancer prevention as well as treatment. -

Age-Dependent Myocardial Transcriptomic Changes in the Rat
Revista Română de Medicină de Laborator Vol. 22, Nr. 1, Martie, 2014 9 Research article DOI: 10.2478/rrlm-2014-0001 Age-dependent myocardial transcriptomic changes in the rat. Novel insights into atrial and ventricular arrhythmias pathogenesis Modificări transcriptomice dependente de vârstă în miocardul de șobolan. Noi aspecte referitoare la patogeneza aritmiilor atriale și ventriculare Alina Scridon1,2, Emmanuelle Fouilloux-Meugnier3, Emmanuelle Loizon3, Marcel Perian1, Sophie Rome3, Claude Julien2, Christian Barrès2, Philippe Chevalier2,4 1.Physiology Department, University of Medicine and Pharmacy of Tîrgu Mureș, 540139, Tîrgu Mureș, Romania 2. Unité de Neurocardiologie, EA4612, Université Lyon 1, F-69008, Lyon, France 3. Unité 1060 INSERM CarMen, Université Lyon 1, F-69008, Lyon, France 4. Hospices Civils de Lyon, Hôpital Louis Pradel, Service de Rythmologie, 69500, Bron, France Abstract Background: Aging is associated with significantly increased prevalence of cardiac arrhythmias, but tran- scriptional events that underlie this process remain to be established. To gain deeper insight into molecular mech- anisms of aging-related cardiac arrhythmias, we performed mRNA expression analysis comparing atrial and ven- tricular myocardium from Wistar-Kyoto (WKY) rats of different ages. Methods: Atrial and ventricular sampling was performed in 3 groups (n=4 each) of young (14-week-old), adult (25-week-old), and aging (47-week-old) WKY rats. mRNA expressions of 89 genes involved in cardiac arrhythmogenicity were investigated using TaqMan Low Density Array analysis. Results: Of the 89 studied genes, 40 and 64 genes presented steady atrial and ventricu- lar expressions, respectively. All genes differentially expressed within the atria of WKY rats were up-regulated with advancing age, mainly the genes encoding for various K+, Ca2+, Na+ channels, and type 6 collagen. -

Non-Canonical Notch Signaling During Early Heart Development
Non-Canonical Notch Signaling During Early Heart Development By Matthew Miyamoto A thesis submitted to Johns Hopkins University in conformity with the requirements for the degree of Master of Science Baltimore, Maryland May 2017 ©2017 Matthew Miyamoto All Rights Reserved Abstract: The canonical Notch signaling pathway has been studied extensively and plays a key role during embryonic development. Recent evidence points to the existence of a non-canonical function of the Notch protein. Elucidation of a non-canonical Notch signaling pathway would significantly alter how the Notch protein is viewed in biological systems. Perhaps more importantly, the identification of downstream effectors could lead to discovery of novel gene networks functioning throughout development. One potential downstream effector of non-canonical Notch is Numb, which interacts with Notch during development. We provide evidence of the existence of a non-canonical pathway in both the embryonic stem cell and during early heart development. By developing two models that alter either the Notch protein or the canonical Notch signaling pathway, we studied non-canonical Notch signaling in vitro and in vivo. Upon overexpression of a tethered form of Notch, which cannot initiate canonical Notch signaling, we observed remarkable apoptosis in embryonic stem cells. Furthermore, Notch overexpression during early heart development led to decreased heart size due to decreased myocyte proliferation when the essential transcription factor to canonical Notch signaling, RBP-j, was knocked out. Similar phenotypes observed in a Numb knockout setting led us to hypothesize that an interaction between Numb and Notch is involved in heart development. Elucidation of a non-canonical Notch signaling pathway may lead to not only a better understanding of congenital heart disease, but also development of other organ systems, as well. -

The Mineralocorticoid Receptor Leads to Increased Expression of EGFR
www.nature.com/scientificreports OPEN The mineralocorticoid receptor leads to increased expression of EGFR and T‑type calcium channels that support HL‑1 cell hypertrophy Katharina Stroedecke1,2, Sandra Meinel1,2, Fritz Markwardt1, Udo Kloeckner1, Nicole Straetz1, Katja Quarch1, Barbara Schreier1, Michael Kopf1, Michael Gekle1 & Claudia Grossmann1* The EGF receptor (EGFR) has been extensively studied in tumor biology and recently a role in cardiovascular pathophysiology was suggested. The mineralocorticoid receptor (MR) is an important efector of the renin–angiotensin–aldosterone‑system and elicits pathophysiological efects in the cardiovascular system; however, the underlying molecular mechanisms are unclear. Our aim was to investigate the importance of EGFR for MR‑mediated cardiovascular pathophysiology because MR is known to induce EGFR expression. We identifed a SNP within the EGFR promoter that modulates MR‑induced EGFR expression. In RNA‑sequencing and qPCR experiments in heart tissue of EGFR KO and WT mice, changes in EGFR abundance led to diferential expression of cardiac ion channels, especially of the T‑type calcium channel CACNA1H. Accordingly, CACNA1H expression was increased in WT mice after in vivo MR activation by aldosterone but not in respective EGFR KO mice. Aldosterone‑ and EGF‑responsiveness of CACNA1H expression was confrmed in HL‑1 cells by Western blot and by measuring peak current density of T‑type calcium channels. Aldosterone‑induced CACNA1H protein expression could be abrogated by the EGFR inhibitor AG1478. Furthermore, inhibition of T‑type calcium channels with mibefradil or ML218 reduced diameter, volume and BNP levels in HL‑1 cells. In conclusion the MR regulates EGFR and CACNA1H expression, which has an efect on HL‑1 cell diameter, and the extent of this regulation seems to depend on the SNP‑216 (G/T) genotype. -
Expression Gene Network Analyses Reveal Molecular Mechanisms And
www.nature.com/scientificreports OPEN Diferential expression and co- expression gene network analyses reveal molecular mechanisms and candidate biomarkers involved in breast muscle myopathies in chicken Eva Pampouille1,2, Christelle Hennequet-Antier1, Christophe Praud1, Amélie Juanchich1, Aurélien Brionne1, Estelle Godet1, Thierry Bordeau1, Fréderic Fagnoul2, Elisabeth Le Bihan-Duval1 & Cécile Berri1* The broiler industry is facing an increasing prevalence of breast myopathies, such as white striping (WS) and wooden breast (WB), and the precise aetiology of these occurrences remains poorly understood. To progress our understanding of the structural changes and molecular pathways involved in these myopathies, a transcriptomic analysis was performed using an 8 × 60 K Agilent chicken microarray and histological study. The study used pectoralis major muscles from three groups: slow-growing animals (n = 8), fast-growing animals visually free from defects (n = 8), or severely afected by both WS and WB (n = 8). In addition, a weighted correlation network analysis was performed to investigate the relationship between modules of co-expressed genes and histological traits. Functional analysis suggested that selection for fast growing and breast meat yield has progressively led to conditions favouring metabolic shifts towards alternative catabolic pathways to produce energy, leading to an adaptive response to oxidative stress and the frst signs of infammatory, regeneration and fbrosis processes. All these processes are intensifed in muscles afected by severe myopathies, in which new mechanisms related to cellular defences and remodelling seem also activated. Furthermore, our study opens new perspectives for myopathy diagnosis by highlighting fne histological phenotypes and genes whose expression was strongly correlated with defects. Te poultry industry relies on the production of fast-growing chickens, which are slaughtered at high weights and intended for cutting and processing. -

Genetic and Epigenetic Variation in the Human Genome
Digital Comprehensive Summaries of Uppsala Dissertations from the Faculty of Medicine 122 Genetic and Epigenetic Variation in the Human Genome Analysis of Phenotypically Normal Individuals and Patients Affected with Brain Tumors CECILIA DE BUSTOS ACTA UNIVERSITATIS UPSALIENSIS ISSN 1651-6206 UPPSALA ISBN 91-554-6490-4 2006 urn:nbn:se:uu:diva-6629 !" #$ % &' !""( ")*&+ , $ , , -$ $ ./ , 0 12 #$ 3 4 $2 5 62 !""(2 7 4 8 $ 7 2 % , -$ 9 : - %,, 3 $ 5 # 2 % 2 &!!2 (; 2 2 :<59 )&=++>=(>)"=>2 7 , $ $ 2 < $ .<9-1 $ .69-1 $ , , 2 #$ $ $ , = $ 2 6 , , $ 3 $ 2 : : 3 ,, $ , -7/? ,, 3 $ $ @ $ $ $ 2 % , = , $ .!A1 3 , , $ B9/&>;C-7/? $3 $ $ 2 : :: +" 3 @ , 9% 3 $ $ !! 2 D$ !"E , !! ,, , $ !! 3 , &>E , 2 #$ $ , !!F2 - ::: $ , , 'G $ 2 D +&2+E , $ 2 : 3 , 3 , !2! 0 '!" . $ 4 69-12 : 3$ $ 4 69- 3 $ $ $ 3 $ 3 $$= -6 = $ . :812 / $ 3 ! 3$$ $ , 2 #$ $ 3 , 3 $ , 2 H $ 3 @ !)" 2 #$, :=:8 $ <9- 69- = $2 / 8 , 9% $ , ,, I)E , $ $ 2 0 $ $ $ 3 , 3 9% $ , 2 "# $ =67 $ % & & -

Product Data Sheet
Product Data Sheet ExProfileTM Human AMPK Signaling Related Gene qPCR Array For focused group profiling of human AMPK signaling genes expression Cat. No. QG004-A (4 x 96-well plate, Format A) Cat. No. QG004-B (4 x 96-well plate, Format B) Cat. No. QG004-C (4 x 96-well plate, Format C) Cat. No. QG004-D (4 x 96-well plate, Format D) Cat. No. QG004-E (4 x 96-well plate, Format E) Plates available individually or as a set of 6. Each set contains 336 unique gene primer pairs deposited in one 96-well plate. Introduction The ExProfile human AMPK signaling related gene qPCR array profiles the expression of 336 human genes related to AMPK-mediated signal transduction. These genes are carefully chosen for their close pathway correlation based on a thorough literature search of peer-reviewed publications, mainly including genes that encode AMP-activated protein kinase complex,its regulators and targets involved in many important biological processes, such as glucose uptake, β-oxidation of fatty acids and modulation of insulin secretion. This array allows researchers to study the pathway-related genes to gain understanding of their roles in the different biological processes. QG004 plate 01: 84 unique gene PCR primer pairs QG004 plate 02: 84 unique gene PCR primer pairs QG004 plate 03: 84 unique gene PCR primer pairs QG004 plate 04: 84 unique gene PCR primer pairs Shipping and storage condition Shipped at room temperate Stable for at least 6 months when stored at -20°C Array format GeneCopoeia provides five qPCR array formats (A, B, C, D, and E) suitable for use with the following real- time cyclers. -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -
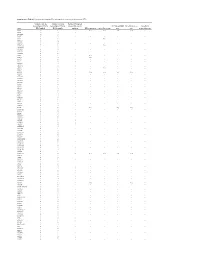
Supplementary Table S1. Prioritization of Candidate FPC Susceptibility Genes by Private Heterozygous Ptvs
Supplementary Table S1. Prioritization of candidate FPC susceptibility genes by private heterozygous PTVs Number of private Number of private Number FPC patient heterozygous PTVs in heterozygous PTVs in tumors with somatic FPC susceptibility Hereditary cancer Hereditary Gene FPC kindred BCCS samples mutation DNA repair gene Cancer driver gene gene gene pancreatitis gene ATM 19 1 - Yes Yes Yes Yes - SSPO 12 8 1 - - - - - DNAH14 10 3 - - - - - - CD36 9 3 - - - - - - TET2 9 1 - - Yes - - - MUC16 8 14 - - - - - - DNHD1 7 4 1 - - - - - DNMT3A 7 1 - - Yes - - - PKHD1L1 7 9 - - - - - - DNAH3 6 5 - - - - - - MYH7B 6 1 - - - - - - PKD1L2 6 6 - - - - - - POLN 6 2 - Yes - - - - POLQ 6 7 - Yes - - - - RP1L1 6 6 - - - - - - TTN 6 5 4 - - - - - WDR87 6 7 - - - - - - ABCA13 5 3 1 - - - - - ASXL1 5 1 - - Yes - - - BBS10 5 0 - - - - - - BRCA2 5 6 1 Yes Yes Yes Yes - CENPJ 5 1 - - - - - - CEP290 5 5 - - - - - - CYP3A5 5 2 - - - - - - DNAH12 5 6 - - - - - - DNAH6 5 1 1 - - - - - EPPK1 5 4 - - - - - - ESYT3 5 1 - - - - - - FRAS1 5 4 - - - - - - HGC6.3 5 0 - - - - - - IGFN1 5 5 - - - - - - KCP 5 4 - - - - - - LRRC43 5 0 - - - - - - MCTP2 5 1 - - - - - - MPO 5 1 - - - - - - MUC4 5 5 - - - - - - OBSCN 5 8 2 - - - - - PALB2 5 0 - Yes - Yes Yes - SLCO1B3 5 2 - - - - - - SYT15 5 3 - - - - - - XIRP2 5 3 1 - - - - - ZNF266 5 2 - - - - - - ZNF530 5 1 - - - - - - ACACB 4 1 1 - - - - - ALS2CL 4 2 - - - - - - AMER3 4 0 2 - - - - - ANKRD35 4 4 - - - - - - ATP10B 4 1 - - - - - - ATP8B3 4 6 - - - - - - C10orf95 4 0 - - - - - - C2orf88 4 0 - - - - - - C5orf42 4 2 - - - - -

Copy Number Variation in Fetal Alcohol Spectrum Disorder
Biochemistry and Cell Biology Copy number variation in fetal alcohol spectrum disorder Journal: Biochemistry and Cell Biology Manuscript ID bcb-2017-0241.R1 Manuscript Type: Article Date Submitted by the Author: 09-Nov-2017 Complete List of Authors: Zarrei, Mehdi; The Centre for Applied Genomics Hicks, Geoffrey G.; University of Manitoba College of Medicine, Regenerative Medicine Reynolds, James N.; Queen's University School of Medicine, Biomedical and Molecular SciencesDraft Thiruvahindrapuram, Bhooma; The Centre for Applied Genomics Engchuan, Worrawat; Hospital for Sick Children SickKids Learning Institute Pind, Molly; University of Manitoba College of Medicine, Regenerative Medicine Lamoureux, Sylvia; The Centre for Applied Genomics Wei, John; The Centre for Applied Genomics Wang, Zhouzhi; The Centre for Applied Genomics Marshall, Christian R.; The Centre for Applied Genomics Wintle, Richard; The Centre for Applied Genomics Chudley, Albert; University of Manitoba Scherer, Stephen W.; The Centre for Applied Genomics Is the invited manuscript for consideration in a Special Fetal Alcohol Spectrum Disorder Issue? : Keyword: Fetal alcohol spectrum disorder, FASD, copy number variations, CNV https://mc06.manuscriptcentral.com/bcb-pubs Page 1 of 354 Biochemistry and Cell Biology 1 Copy number variation in fetal alcohol spectrum disorder 2 Mehdi Zarrei,a Geoffrey G. Hicks,b James N. Reynolds,c,d Bhooma Thiruvahindrapuram,a 3 Worrawat Engchuan,a Molly Pind,b Sylvia Lamoureux,a John Wei,a Zhouzhi Wang,a Christian R. 4 Marshall,a Richard F. Wintle,a Albert E. Chudleye,f and Stephen W. Scherer,a,g 5 aThe Centre for Applied Genomics and Program in Genetics and Genome Biology, The Hospital 6 for Sick Children, Toronto, Ontario, Canada 7 bRegenerative Medicine Program, University of Manitoba, Winnipeg, Canada 8 cCentre for Neuroscience Studies, Queen's University, Kingston, Ontario, Canada. -
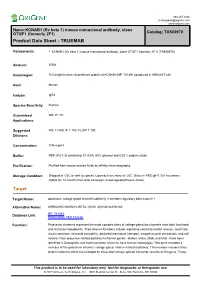
New PDF Document
888.267.4436 [email protected] www.origene.com Name:KCNAB1 (Kv beta 1) mouse monoclonal antibody, clone OTI2F1 (formerly 2F1) Catalog: TA503970 Product Data Sheet - TRUEMAB Components: • KCNAB1 (Kv beta 1) mouse monoclonal antibody, clone OTI2F1 (formerly 2F1) (TA503970) Amount: 100ul Immunogen: Full length human recombinant protein of KCNAB1(NP_751891) produced in HEK293T cell. Host: Mouse Isotype: IgG1 Species Reactivity: Human Guaranteed WB, IF, FC Applications: Suggested WB 1:1000, IF 1:100, FLOW 1:100, Dilutions: Concentration: 0.96 mg/ml Buffer: PBS (PH 7.3) containing 1% BSA, 50% glycerol and 0.02% sodium azide. Purification: Purified from mouse ascites fluids by affinity chromatography Storage Condition: Shipped at -20C or with ice packs. Upon delivery store at -20C. Dilute in PBS (pH7.3) if necessary. Stable for 12 months from date of receipt. Avoid repeated freeze-thaws. Target Target Name: potassium voltage-gated channel subfamily A member regulatory beta subunit 1 Alternative Name: AKR6A3|KCNA1B|KV-BETA-1|Kvb1.3|hKvBeta3|hKvb3 Database Link: NP_751891 Entrez Gene 7881 Human Function: Potassium channels represent the most complex class of voltage-gated ion channels from both functional and structural standpoints. Their diverse functions include regulating neurotransmitter release, heart rate, insulin secretion, neuronal excitability, epithelial electrolyte transport, smooth muscle contraction, and cell volume. Four sequence-related potassium channel genes - shaker, shaw, shab, and shal - have been identified in Drosophila, and each has been shown to have human homolog(s). This gene encodes a member of the potassium channel, voltage-gated, shaker-related subfamily. This member includes three distinct isoforms which are encoded by three alternatively spliced transcript variants of this gene.