BMI the Runnymede Hospital Newapproachcomprehensive Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Highfield House Woodlands Road East • Virginia Water • Surrey Highfield House Woodlands Road East • Virginia Water • Surrey • GU25 4PH
Highfield House Woodlands Road East • Virginia Water • Surrey Highfield House Woodlands Road East • Virginia Water • Surrey • GU25 4PH Virginia Water 0.4 mile • Ascot 5.1 miles • Windsor 7.3 miles • Heathrow (T5) 7.3 miles • Central London 25.2 miles (All distances are approximate) Exceptional family home with indoor pool, guest house, tennis court and 2.31 acre private plot on the world renowned Wentworth Estate. Main House Entrance Hall • Drawing Room • Study • Dining Room • Kitchen/Breakfast Room • Orangery Family Room • Indoor Swimming Pool • Sauna • Gymnasium • Wine Store • Utility Room Principal Bedroom with Double Dressing Room • Ensuite Bathroom and Balcony 2 Further Ensuite Bedrooms 4 Further Bedrooms • 3 of which Ensuite Detached Annexe Kitchen • Living/Dining Room • Reception Room • 2 Bedrooms • Family Bathrooms • W/C Gardens and Grounds Triple Garage with Games Room Above • Sweeping Driveway • Enclosed Parking Courtyard • Large Entertaining Patio Loggia • Tennis Court • Manicured Lawned Gardens In all about 2.31 acres Savills London Savills Sunningdale Barton Wyatt 33 Margaret Street Mount Lodge 2 Station Approach London W1G 0JD Sunningdale SL5 0EP Virginia Water GU25 4DL Trevor Kearney Charlie Fisher Rupert Wyatt 07807 999872 07870 999 586 07768 410910 [email protected] [email protected] [email protected] Situation Highfield House is superbly situated on Woodlands Road East, a highly prestigious road located between the picturesque shopping parades of Virginia Water and the world renowned Wentworth Golf Club; just 0.7 miles from Virginia Water station - 40 minutes to Waterloo and the excitement of central London. Regarded as the premier countryside location in the UK, the prestigious Wentworth Estate is a quintessentially English oasis within touching distance of London. -

Runnymede Borough Council, Civic Centre, Station Road, Addlestone
The Planning Inspectorate National Infrastructure Planning Temple Quay House 2 The Square Bristol BS1 6PN Emailed to: [email protected] FAO Mr Hefin Jones 25 July 2019 Dear Sir/Madam Location: Southampton to London Pipeline Project Proposal: Notification from Esso of acceptance of their DCO application (by the Planning Inspectorate) and deadline for registering as a Interested Party Following the Planning Inspectorate’s acceptance of an application for a Development Consent Order (DCO) for the Southampton to London Pipeline, Runnymede Borough Council requests to be registered as an Interested Party at the Examination. Runnymede Borough Council (RBC) is a host Borough and also landowner affected by the development. Chertsey Meads, a public open space owned by the Council is a key parcel of land required to be used to enable the pipeline to go under the River Thames. Runnymede Borough Council is not a unitary authority and therefore a number of matters, such as Highways, Transport and Archaeology fall within the remit of Surrey County Council (SCC). Esso’s discussions with SCC have not been shared with RBC and therefore RBC are now making enquiries as to SCC’s position. This letter provides a summary of the main aspects of the proposal which RBC is presently in a position to confirm that it agrees and/or disagrees, together with an appropriate explanation, in accordance with the Planning Inspectorate Advice Note 8.3. The response below is an initial response as the Council is currently reviewing the detailed documentation submitted with the DCO application and therefore the Council reserves the right to make further written representations during the examination should it be required. -

Runnymede Community Engagement Plan
Southampton to London Pipeline Project Community Engagement Plan Revision No. 2.0 June 2021 Runnymede Borough Council Southampton to London Pipeline Project Community Engagement Plan – Runnymede Borough Council Contents 1 Introduction ..................................................................................................................................1 2 Scope ............................................................................................................................................2 3 Overview of the Project................................................................................................................3 4 Community Engagement Team ...................................................................................................4 5 Community Stakeholders ............................................................................................................5 6 Core Engagement Channels ........................................................................................................6 7 Frequency of engagement ...........................................................................................................8 8 Core Engagement Topics ............................................................................................................9 9 Within Runnymede Borough ..................................................................................................... 10 10 Location-Specific Tactical Communication Plans ................................................................... -

White Cottage Ottershaw • Surrey White Cottage Murray Road, Ottershaw, Surrey, Kt16 0Hp
WHITE COTTAGE OTTERSHAW • SURREY WHITE COTTAGE MURRAY ROAD, OTTERSHAW, SURREY, KT16 0HP A stunning contemporary family home, thoughtfully designed for entertaining as well as modern family living. Beautiful views Perfect for entertaining Light and bright accommodation Lateral living Gated driveway DESCRIPTION A fabulous modern family home, built in 2011 by the current owners. The modern design of this house allows light to flood in and provides excellent balanced accommodation for comfortable family living as well as outstanding entertaining space. Approached via electric gates, the property has been thoughtfully designed and features underfloor heating throughout, air ventilation and a control 4 system. The front door leads into the striking entrance hall. To the right is the true hub of this home, the open plan kitchen/breakfast/ dining/living room with corner bi-fold doors that open up to give breath-taking views of the gardens and fields beyond. Clever use of decking joins the indoor living space with the outdoors. The master bedroom suite is unique with its open plan en suite shower room overlooking the rear garden and views beyond and a walk in wardrobe. 2 further bedrooms, both with access out to the rear garden, a study, utility room, generous family bathroom and guest cloakroom complete the accommodation. The property is situated on a generous plot consisting beautifully maintained gardens, a pond and a large decking area ideal for al fresco entertaining. LOCATION Ottershaw is a village in the Runnymede district of Surrey, England about 20 miles to the south-west of London. It is part of the Foxhills ward. -

THE RIVER THAMES a Complete Guide to Boating Holidays on the UK’S Most Famous River the River Thames a COMPLETE GUIDE
THE RIVER THAMES A complete guide to boating holidays on the UK’s most famous river The River Thames A COMPLETE GUIDE And there’s even more! Over 70 pages of inspiration There’s so much to see and do on the Thames, we simply can’t fit everything in to one guide. 6 - 7 Benson or Chertsey? WINING AND DINING So, to discover even more and Which base to choose 56 - 59 Eating out to find further details about the 60 Gastropubs sights and attractions already SO MUCH TO SEE AND DISCOVER 61 - 63 Fine dining featured here, visit us at 8 - 11 Oxford leboat.co.uk/thames 12 - 15 Windsor & Eton THE PRACTICALITIES OF BOATING 16 - 19 Houses & gardens 64 - 65 Our boats 20 - 21 Cliveden 66 - 67 Mooring and marinas 22 - 23 Hampton Court 68 - 69 Locks 24 - 27 Small towns and villages 70 - 71 Our illustrated map – plan your trip 28 - 29 The Runnymede memorials 72 Fuel, water and waste 30 - 33 London 73 Rules and boating etiquette 74 River conditions SOMETHING FOR EVERY INTEREST 34 - 35 Did you know? 36 - 41 Family fun 42 - 43 Birdlife 44 - 45 Parks 46 - 47 Shopping Where memories are made… 48 - 49 Horse racing & horse riding With over 40 years of experience, Le Boat prides itself on the range and 50 - 51 Fishing quality of our boats and the service we provide – it’s what sets us apart The Thames at your fingertips 52 - 53 Golf from the rest and ensures you enjoy a comfortable and hassle free Download our app to explore the 54 - 55 Something for him break. -

Bourne View 2 Keepers Walk • Wentworth Estate • Virginia Water • Surrey
BOURNE VIEW 2 KEEPERS WALK • WENTWORTH ESTATE • VIRGINIA WATER • SURREY BOURNE VIEW 2 KEEPERS WALK • WENTWORTH ESTATE VIRGINIA WATER • SURREY • GU25 4RU Virginia Water 1 mile, Ascot 4 miles, Windsor 6 miles, Heathrow (T5) 9 miles, Central London 21 miles (Distances are approximate) A well-appointed and maintained family home on the world renowned Wentworth Estate Main House Entrance Hall • Kitchen/Breakfast/Family Room • Drawing Room • Dining Room • Study Gymnasium • Utility Room • 2 WCs Principal Bedroom with Ensuite and Dressing Room 4 further Bedroom Suites • Galleried Landing • Front Balcony Media/Games Room • Shower Room • Kitchenette • Plant Room • Store Gardens and Grounds Gated Driveway • Detached Double Garage • Landscaped Gardens • Entertaining Terrace In all about 0.56 acres Savills Sunningdale Savills London Office Mount Lodge, London Road 33 Margaret Street Sunningdale SL5 0EP London W1G 0JD Charlie Fisher Trevor Kearney 07870 999 586 07807 999872 [email protected] [email protected] savills.co.uk Situation Bourne View is ideally situated just 0.6 miles from Virginia Water station - 40 minutes to Waterloo and the excitement of central London. Regarded as the premier countryside location in the UK, the prestigious Wentworth Estate is a quintessentially English oasis within touching distance of London. There are some first class local amenities in Virginia Water village, including a number of delightful restaurants, cafes, delicatessens, sophisticated fashion boutiques and general stores. Within a five minute drive is the Michelin 2 star restaurant at Coworth Park Hotel, which also has impressive spa facilities. On the Wentworth Estate is the world renowned Wentworth Club, with its championship golf course, along with three other outstanding courses, tennis, health club with in and outdoor swimming pools. -

Beaumont the Mount Close • Virginia Water • Surrey Beaumont the Mount Close Virginia Water • Surrey
BEAUMONT THE MOUNT CLOSE • VIRGINIA WATER • SURREY BEAUMONT THE MOUNT CLOSE VIRGINIA WATER • SURREY Well presented detached family home with potential to convert the roof, subject to planning permission Entrance hall • Drawing room • Dining room • Study Kitchen/breakfast/family room • Utility room • Cloakroom Master bedroom with full bathroom and dressing room/bedroom 5 • Guest suite • 2 further bedrooms Family bathroom Attached double garage • Southerly facing rear garden Cul‐de‐sac location • Large roof space for possible conversion ﴾STPP﴿ • EPC: C Virginia Water shops and station 0.7 miles A30 2.3 miles • Egham Station 2.8 miles • Ascot 6.3 miles Windsor 8 miles • Heathrow ﴾T5﴿ 8 miles Central London 26 miles ﴿All distances are approximate﴾ These particulars are intended only as a guide and must not be relied upon as statements of fact. Your attention is drawn to the Important Notice on the last page of the text. Beaumont, The Mount Close, Virginia Water, Surrey An attractive, well presented detached family home built by Burwood Homes approximately 11 years ago, owned by the current vendor since new. The accommodation is arranged over two spacious floors. There is also potential to convert the roof space to create possibly two more bedrooms, although the usual planning consent will be required. Situation Beaumont forms part of a small cul‐de‐sac of only 5 properties, close to the recreation ground, tennis courts and shops. Schools: Educational facilities in the area include Eton College, Papplewick, Christchurch C of E Infant school, Brigidine, Upton House, Bishopsgate, St. George's and St John's Beaumont. -

Runnymede Borough Council
RBC C.S. 150617 Runnymede Borough Council COMMUNITY SERVICES COMMITTEE 15 June 2017 at 7.30 pm Members of the Councillors Miss M N Heath (Chairman), P J Waddell (Vice-Chairman), Committee Present: D E Anderson-Bassey, Mrs D V Clarke, Miss D Khalique, B W Pitt and Mrs G Warner. Members of the Committee absent: Councillors Mrs M T Harnden, N M King and S M Mackay. 56 FIRE PRECAUTIONS The Chairman read out the Fire Precautions. 57 PRESENTATION BY EMMA WARREN, CURATOR, CHERTSEY MUSEUM The Committee received an informative presentation about Chertsey Museum, from its curator, Emma Warren. Emma gave Members a brief history of the museum, covering its earliest days in the 1970s at the Old Town Hall, up to the present day, with illustrations of the new redesigned garden, shortly opening at their current home, ‘The Cedars’, in Chertsey. Members were impressed with the range of activities, exhibitions and innovative marketing ideas which contributed to the success of the museum, all provided within a limited budget and by a small number of dedicated staff and volunteers. The significant support of the Olive Matthews Trust and the Friends of Chertsey Museum was noted with appreciation by the Committee. Notable projects included the continuation of the 1st World War related works, the borough history ‘app’, ‘Fashion and Freedom’ (Women in Society) the River Festival; celebrating the River Thames and a project/exhibition on the creation of Victory Park in Addlestone. The museum’s valued outreach and educational work, as well as its participation in loaning and borrowing important pieces nationwide was commended. -

St Andrews Andrwentworthw E N T W O R T H EESTATES T a T E Computer Generated Artist’S Impression
St Andrews andrWENTWORTHW E N T W O R T H EESTATES T A T E Computer generated artist’s impression. Indicative only. Two pairs of double gates secure the carriage driveway, A magnificently presented home with equally impressive interior space, this imposing beyond which lies the private setting of St Andrews, Runnymede Homes’ latest fine new home. This well-proportioned and perfectly balanced home takes its architectural cue from the Georgian period, warm red brick elevations are complimented new home exudes the impeccably high standard set by Runnymede, as before, on the by mellow stone detailing by way of the sash-window surrounds, gable end friezes and portico entrance. This fabulous new home will surely stand the test of time. Located in Gorse Hill Road on the Wentworth Estate, St Andrews is just a short walk from the picturesque Wentworth Estate. village shops and mainline railway station. making an entrance St Andrews is a beautifully appointed The second floor provides two further five/six bedroom home extending to just under double bedrooms, one of which is large 6,500 sq ft, which includes an au-pair suite over enough to become a leisure room; each share the double garage. a ‘Jack & Jill’ bathroom. Beyond its stunning stone portico entrance lie The mature half an acre tree-lined setting three levels of practical and light filled interiors. includes a generous south-facing lawned and The kitchen/breakfast area/family room is an landscaped garden, with large Indian impressive focal point, with folding glazed Sandstone terrace from which to enjoy this doors to the rear of the property. -

Greenacres Farm Licence
Licence Ref. 2012/GREENACRES Caravan Sites and Control of Development Act 1960 Site Licence Site: Greenacres Farm, Hardwick Lane, Chertsey, Surrey, KT16 0AD Granted to: Mrs Lena Draper-Smith Whereas you have made an application received by Runnymede Borough Council (hereinafter called “the Council”) on the 6 March 2012 for the issue under Section 3 of the Caravan Sites and Control of Development Act 1960 (hereinafter called “the Act” of a site licence in respect of land at Greenacres Farm, Hardwick Lane, Chertsey, Surrey, KT16 0AD. And whereas the Council, as local planning authority, has granted permission under the Town and Country Planning Act 1990. Now the Council hereby issue this licence under Part 1 of the Act authorising the use as a caravan site of the land described in the First Schedule hereto upon and subject to the conditions set out in the Schedule of conditions attached to the licence hereto. First Schedule The caravan site known as Greenacres Farm, Hardwick Lane, Chertsey, Surrey, KT16 0AD as shown on the plan attached to this licence. Signature: __________________________ Date: 1 May 2012 Peter Sims Director of Technical Services Our primary aim: to enhance the quality of life for Runnymede residents Caravan Sites and Control of Development Act 1960 (as amended) Schedule of conditions attached to Licence Ref: 2012/GREENACRES Site: Greenacres Farm, Hardwick Lane, Chertsey, Surrey, KT16 0AD Licence granted to: Mrs Lena Draper-Smith At: Greenacres Farm, Hardwick Lane, Chertsey, Surrey, KT16 0AD. (Signature) ............................................... (Date) 1 May 2012 Peter Sims Director of Technical Services. Authorised by Runnymede Borough Council ______________________________________________________________________________________ This Licence is specifically tailored to meet the needs of this site as a Gypsy/Travellers Site, regard has been given to the DCLG Good Practice Guide for Designing Gypsy and Traveller Sites. -
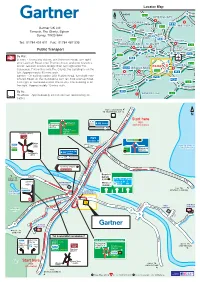
Gartner Group -Egham
Chertsey Thorpe B388 Windsor A308 Staines M25(M3) Chertsey (A320) Thorpe Park Locator Map 21 A4010 A413 N AMERSHAM HIGH WYCOMBE A404 M25 A413 WATFORD Gartner UK Ltd A355 A40 Tamesis, The Glanty, Egham 4 3 A40 Surrey, TW20 9AH 2 A4155 A4155 A404 M40 UXBRIDGE Tel: 01784 431 611 Fax: 01784 487 595 16 MAIDENHEAD SLOUGH A40 HEATHROW Public Transport 7 AIRPORT 8/9 6 15 4 A4 5 M4 By Rail. A308 Staines - On exiting station, join Gresham Road, turn right M4 14 onto Laleham Road, onto Thames Street and onto Clarence A316 Street. Go over Staines Bridge then turn right onto The 10 EGHAM 13 STAINES A329(M) Causeway. Follow this onto The Glanty, the building is on the BRACKNELL A30 left. Approximately 30 mins walk. 12 M3 WOKINGHAM A322 Egham - On exiting station, join Station Road, turn right onto M3 Church Road. At the roundabout turn left onto Avenue Road. A327 3 M25 Turn right at roundabout onto The Glanty. The building is on A3 the right. Approximately 10 mins walk. 4 10 By Air. M3 FARNBOROUGH A3 Heathrow - Approximately 20 mins by taxi (depending on ( traffic). M25 CLOCKWISE TO HEATHROW JCT 14 5 2 N ( M Start here 13 1 3m M25 Kingston A30 Staines Wraysbury (A308) (Anti-Clockwise) (B376) Bagshot A30 Egham Chertsey (A320) Windsor (A308) Thorpe Park M25 Junction 13 Egham A30 Egham (M25) town B 3 KING GEORGE VI Staines centre 7 6 Staines Wraysbury RESERVOIR A30 A30 (B376) London (W) Sunningdale A30 Staines (A30) S T 13 1 2m A I N E S B Y - Chertsey (A320) PA S S Thorpe Park R I V E R Bagshot T H A308 A M Egham A308 TO E S (M3, M23, M20) A WINDSOR -

The 27Th British Rowing Tour the Middle Thames Maidenhead to Putney 27Th - 30Th August 2020 Provisional Programme
The 27th British Rowing Tour The Middle Thames Maidenhead to Putney 27th - 30th August 2020 Provisional Programme Thursday Boats and trailers to Maidenhead Rowing Club, unload and rig 27th Aug Transfer trailers to the Lensbury Hotel (p.m.) Check in Lensbury Hotel, Teddington Buffet dinner Lensbury Hotel Friday Coach from hotel to Maidenhead 28th Aug Row Maidenhead to Eton Picnic lunch at Eton Masters Boathouse Row to Staines Boat Club Dinner, Lensbury Hotel Saturday Coach to Staines 29th Aug Row Staines to Walton Lunch at Walton Rowing Club Row to Lensbury Hotel Dinner, Lensbury Hotel Sunday Row Teddington to Putney 30th Aug Lunch at Thames RC or Vesta RC, load trailers, depart For Walkers: The Thames Path follows the whole river, so walkers can easily accompany the rowers. There’s a description, divided into sections, on this website, though it goes upstream rather than downstream. Our Hotel The Lensbury Resort and Club British Rowing Tour 2020 Day 1 a.m. Maidenhead-Eton 10 km LUNCH Eton Masters Boathouse 1.2 km Romney Lock 3.7 km Boveney Lock 5.1 km Bray Lock 2.0 km Maidenhead RC START MAIDENHEAD Day 1 a.m. Maidenhead to Eton Maidenhead Info Bray Info Dorney Info Eton Info British Rowing Tour 2020 Day 1 p.m. Eton—Staines 10.4 km FINISH Staines BC 2.1 km Bell Weir Lock 4.7 km Old WindsorLock 3.6 km Eton Masters Boathouse LUNCH Day 1 p.m. Eton to Staines WindsorInfo Runnymede Info Staines Info British Rowing Tour 2020 Day 2 a.m. Staines-Walton 12.5 km Day 2 a.m.