Findings from the Nord Trøndelag Health
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Kvinnherad Kommune Møteinnkalling
Kvinnherad kommune Møteinnkalling Utvalg: Kontrollutvalet Møtestad: Kommunestyresalen, Kvinnherad Rådhus Dato: 24.08.2016 Tidspunkt: 13:00 NB – tidspunkt for møtestart er kl. 13.00 Dersom nokon av medlemmene ikkje kan møte og må melde forfall, vert dei bedne om å gjere dette så tidleg som råd er ved å ringa til Kari Nygard tlf. 55 23 94 06 / 916 64 183 eller til Hogne Haktorson, tlf. 55 23 94 53 / 911 05 982. Til varamedlemar er denne innkallinga å sjå på som ei orientering. Dersom det vert aktuelt at varamedlemar må møta, vil det bli gjeve nærmare beskjed. Det er planlagt at Kari Nygard møter frå sekretariatet, på dette møtet. Synnøve Solbakken kontrollutvalsleiar Hogne Haktorson Kari Marie Nygard kontrollsjef seniorrådgjevar Dokumentet er elektronisk godkjent og har derfor ikkje underskrift. Kopi: Vararepresentantar til kontrollutvalet Ordførar Revisor Rådmann -1- Saksliste Utvalgs- Innhold Lukket Arkiv- saksnr saksnr PS 28/16 Godkjenning av innkalling og sakliste PS 29/16 Godkjenning av protokoll frå forrige møte PS 30/16 Orienteringssak vedr. rådgjevarstilling for prosjekt 2014/69 Kvinnheradspakken PS 31/16 Vurdering av om Deloitte er uavhengig i høve til 2016/51 Kvinnherad kommune PS 32/16 Revisjonsplan for Kvinnherad kommune 2016 2016/32 PS 33/16 Framlegg til budsjett for kontroll- og tilsynsarbeid 2016/20 for 2017 PS 34/16 Referatsaker RS 8/16 Utdrag frå protokoll kommunestyret 26.05.16 2016/8 RS 9/16 Notat - referatsak som gjeld henvending 2014/69 vedr.kommunedelplan RS 10/16 Referatsak til KUV-møte 24.08.16 vedr. vedtak i 2015/210 Levekårskomiteen 04.04.16 RS 11/16 Revidert nasjonalbudsjett 2016 og 2016/19 kommuneopplegget for 2017 RS 12/16 Budsjettbrev frå Fylkesmannen 2016 2016/32 RS 13/16 Notat til kontrollutvalet vedr. -

THE WESTFIELD LEADER LEADING and MOST WIDELY CIRCULATED WEEKLY NEWSPAPER in UNION COUNTY Published Blnth YUAK—Wo
THE WESTFIELD LEADER LEADING AND MOST WIDELY CIRCULATED WEEKLY NEWSPAPER IN UNION COUNTY Published blNTH YUAK—wo. 3Y Post Otttot, WutliU, N. J. WESTFIELD, NEW JERSEY, THURSDAY, MAY 26, 1949 Every Thursday. to Begin 259 Children to Participate in Local Stores, Offices Borough School Memorial Day To < W Monday Time Schedule Memorial Day • uonn Station Stores and local offices, includ- Census Data 8:30 A.M. Ring-ing of church Elementary School Choir Festival ing the Municipal Building and bells. Post Office, will be closed Monday 8:30 A.M. Parade assembly The elementary school Choir Festival will be held this evening in observation of Memorial Day. Due Next Fall at Ferris PI. end at 7:30 o'clock at Roosevelt Junior High School auditorium. Approx- As a legal holiday, parking meters Prospect St. Parade Monday Resident* Ask imately 250 children will take part in the singing and a group from will not be in operation. Barber- Education Board Lincoln .School will dance the Virginia Rael, accompanied by the choirs shops will be closed Monday but 9:00 A.M. Services at Mon- iK-il to Ponder singing "The Arkansas Traveler," Rhythm instruments will be added will be open on Wednesday. To Study Data ument. C«l. June* H. HoagTo~BeGrand Again* Bugs thth e MexicaMi n song-, "Fit"Fiesta," The Wett/itld Leader will also For Future Plans 9:15 A.M. Procession starts. Marshal at Annual May 30 Event nd will be played by a group from be closed all day Monday. Club Line of march will be from Mon- n the comstruction of a e Franklin School Choir: Sally correspondents and advertisers are A large number of Weetfteld organizations, including tfc Spring Flower illace, Iris Hann, Susan Hait- MOUNTAINSIDE — The boro ument out Broad king- lot on the north urged to co-operate by sending census being taken for the benefit talion from the National Guard Armory here, will maich in a ian, Wendy Holmes, Judy Hes copy in early, tomorrow if possi- St. -

Lasting Legacies
Tre Lag Stevne Clarion Hotel South Saint Paul, MN August 3-6, 2016 .#56+0).')#%+'5 6*'(7674'1(1742#56 Spotlights on Norwegian-Americans who have contributed to architecture, engineering, institutions, art, science or education in the Americas A gathering of descendants and friends of the Trøndelag, Gudbrandsdal and northern Hedmark regions of Norway Program Schedule Velkommen til Stevne 2016! Welcome to the Tre Lag Stevne in South Saint Paul, Minnesota. We were last in the Twin Cities area in 2009 in this same location. In a metropolitan area of this size it is not as easy to see the results of the Norwegian immigration as in smaller towns and rural communities. But the evidence is there if you look for it. This year’s speakers will tell the story of the Norwegians who contributed to the richness of American culture through literature, art, architecture, politics, medicine and science. You may recognize a few of their names, but many are unsung heroes who quietly added strands to the fabric of America and the world. We hope to astonish you with the diversity of their talents. Our tour will take us to the first Norwegian church in America, which was moved from Muskego, Wisconsin to the grounds of Luther Seminary,. We’ll stop at Mindekirken, established in 1922 with the mission of retaining Norwegian heritage. It continues that mission today. We will also visit Norway House, the newest organization to promote Norwegian connectedness. Enjoy the program, make new friends, reconnect with old friends, and continue to learn about our shared heritage. -

Retningsliner for Graving I Offentlig Veg - NKF Nettverksgruppe Veg Og Trafikk Hordaland
1 Retningsliner for graving i offentlig veg - NKF nettverksgruppe Veg og trafikk Hordaland Askøy, Fjell, Sund, Kvam, Voss, Ulvik, Granvin, Lindås, Austrheim, Meland, Os , Radøy, Gulen 2 Retningsliner for graving i offentlig veg - NKF nettverksgruppe Veg og trafikk Hordaland Forord Framføring av kablar, leidningar, samt graving i vegar og gater medfører ofte ulemper for trafikantar og vegnaboar. Etter slikt arbeid viser det seg ofte at det oppstår setningar og sprekkdanningar som følgje av mangelfull istandsetting. Dette medfører ein dårlegare standard på vegar og gater. Nettverksgruppen Veg og trafikk Hordaland har med utgangspunkt i Statens vegvesen – Region vest sine Retningliner for framføring av kablar, leidningar og graving i offentleg veg -2006, tilpassa desse for kommunane i Hordaland. Målet er det same: sikre ei effektiv og omsynsfull gjennomføring og ei fullgod istandsetting etter arbeidet, slik at samfunnet ikkje vert påført unødige ulemper og kostnader. Dette heftet skal gi opplysningar om kva ein søknad skal innehalde og kvar den skal sendast. I tillegg vert det informert om korleis arbeidet skal gjennomførast og kva for krav som vert stilla, samt det ansvar den som gjennomfører arbeidet har. Retningslinene gjeld for alle type arbeid, til dømes boring og graving i veg og gategrunn, samt for luftstrekk over veg m.m. Det vil normalt ikkje bli gitt graveløyve i veger og gater som har nyare dekke enn 3 år. Den einskilte kommune kan fastsetje lengre sperrefrist. Retningslinene gjeld for fylgjande kommunar og søknad om graving i -

Outbreak of Meningococcal Disease in Western Norway Due to a New Serogroup C Variant of the ET-5 Clone: Effect of Vaccination and Selective Carriage Eradication
Epidemiol. Infect. (1999), 123, 373–382. Printed in the United Kingdom # 1999 Cambridge University Press Outbreak of meningococcal disease in western Norway due to a new serogroup C variant of the ET-5 clone: effect of vaccination and selective carriage eradication " " # $ % I.SMITH *, A. K. LEHMANN ,L.LIE, A.DIGRANES , D.A.CAUGANT , % % " E. A. HØIBY ,L.O.FRØHOLM A. HALSTENSEN " Institute of Medicine, Uniersity of Bergen, N-5021 Bergen, Norway # Lindab s Health Authority, N-5050 Lindab s, Norway $ Department of Microbiology and Immunology, The Gade Institute, Haukeland Uniersity Hospital, N-5021 Bergen, Norway % Department of Bacteriology, National Institute of Public Health, N-0403 Oslo, Norway (Accepted 14 August 1999) SUMMARY A new sulphonamide resistant (SR) C:15:P1.7,16 meningococcal strain, a variant of the ET-5 clone, dominated in an outbreak of 22 cases in western Norway commencing in 1995. The first eight patients were 15–21 years old from the Nordhordland area, initiating a carrier study in the local high schools. Carriage of SR serogroup C meningococci was detected by routine methods and treated with a single dose of ofloxacin 400 mg. Of 20 treated carriers, 14 harboured the outbreak strain C:15:P1.7,16. Vaccination of 4000 children, adolescents and close contacts of patients was also performed. After the intervention, 14 additional cases of meningococcal disease occurred, 8 due to the outbreak strain. However, incidence rates dropped from 180 to 30 per 100000 per year in the student population, but increased from 0 to 13 in the rest of the population in Nordhordland. -

Folketal Og Demografi 2 Føreord
HORDALAND I TAL Nr. 1 - 2018 Folketal og demografi 2 Føreord Hordaland i tal nr. 1 2018 presenterer folketalsutviklinga i fylket og på regions- og kommunenivå. I dette nummeret tek vi og eit blikk nordover til Sogn og Fjordane som saman med Hordaland skal inngå i Vestland fylkeskommune frå 1. januar 2020. Frå 2017 til 2018 auka folketalet i Hordaland med 0,5 % som er den lågaste veksten sidan 1998. Hordaland er ikkje ein isolert del av Europa og av verda, men blir påverka av internasjonale konjunkturar, av krigar og sosial uro og nød i andre delar av verda som driv menneske på flukt. Dette påverkar folketalsut- viklinga i Hordaland. Innvandring har bidrege positivt til folketalsutviklinga i alle kommunar i Hordaland og Sogn og Fjordane sidan 2013 og statistikken viser at mange kommunar er heilt avhengig av nye innbyggjarar frå utlandet. For kommunane med befolkningsnedgang har innvandringa bremsa reduksjonen i folketalet. I 2017 fekk vi ein kraftig reduksjon i innvandringa til Hordaland. Samstundes ser vi at det kjem stadig færre innvandrar frå Europa, som har dominert innvandringsstraumen til Hordaland dei seinare åra. Dette heng saman med auken i arbeidsløyse i Noreg og i nokre høve ein betre økonomisk situasjon i dei landa dei har kome frå. Polakkar er likevel framleis den klårt største innvandrargruppa i Noreg. Saman med rekordlåg netto innanlandsk flytting og lågt fødselsoverskot, har dette ført til den låge folkeveksten vi no har hatt siste året i Hordaland. Korleis desse tilhøva slår ut i din kommune og din region, kan du lese meir om i dette nummeret av Hordaland i tal, saman med mykje anna nyttig informasjon om folketalsutviklinga. -

Kommunedelplan for Sambandet Vest Silingsrapport
Kommunedelplan for Sambandet vest Silingsrapport Askøy kommune og kommunane Meland, Radøy og Lindås (Alver kommune i 2020): KOMMUNEDELPLAN FOR SAMBANDET VEST VEDLEGG I: SILINGSRAPPORT, juni 2019 1 Kommunedelplan for Sambandet vest Silingsrapport Oppdragsgjevar: Alver kommune Oppdragsgjevars kontaktperson: John Fredrik Wallace Rådgjevar Norconsult AS, Valkendorfsgate 6, NO-5012 Bergen Oppdragsleiar: Øystein Skofteland Fagansvarleg: Øystein Skofteland Andre nøkkelpersonar: Alv Terje Fotland, Lene Merete Rabben, Kristoffer Åsen Røys, Heidi Handeland, Arne Værnes. Kristina Ebbing Wensaas Oppdragsnummer NO: 5190526 001 2019-05-22 Silingsrapport Versjon 1 OYSKO ATFOT/KRIWEN OYSKO Versjon Dato Beskrivelse Utarbeidet Fagkontrollert Godkjent Dette dokumentet er utarbeidet av Norconsult AS som del av det oppdraget som dokumentet omhandler. Opphavsretten tilhører Norconsult AS. Dokumentet må bare benyttes til det formål som oppdragsavtalen beskriver, og må ikke kopieres eller gjøres tilgjengelig på annen måte eller i større utstrekning enn formålet tilsier. 2 Kommunedelplan for Sambandet vest Silingsrapport INNHALD 1 INNLEIING 5 4.3 FORKASTA LINJER 16 4.4 OPPSUMMERING 19 1.1 BAKGRUNN 5 5 ANALYSAR 21 2 MÅL MED PROSJEKTET 7 5.1 TRANSPORT, BUSETNAD OG ARBEIDSLIV 21 2.1 NASJONALE OG REGIONALE MÅL 7 5.2 TRAFIKK 27 2.2 SAMFUNNSMÅL 7 5.3 KOSTNAD 28 2.3 EFFEKTMÅL 8 5.4 KONFLIKTANALYSE 29 2.4 VEGSTANDARD 9 5.5 AREALPLANAR I OMRÅDET 33 3 METODE 11 6 SILING 35 3.1 SILINGSKRITERIUM OG SILING 11 6.1 KORRIDOR AA 35 3.2 VURDERING AV MÅLOPPNÅING 12 6.2 KORRIDOR -

Kystlynghei I Austrheim, Lindås, Radøy, Meland, Øygarden, Fjell Og Sund Registreringer I 2013 I Forbindelse Med Handlingsplan for Kystlynghei
MVA-rapport 1/2014 Kystlynghei i Austrheim, Lindås, Radøy, Meland, Øygarden, Fjell og Sund Registreringer i 2013 i forbindelse med Handlingsplan for kystlynghei Miljøvern- og klimaavdelinga Fylkesmannen i Hordaland Utgiver: Rapport nr: Fylkesmannen i Hordaland, miljøvern‐ og klimaavdelinga MVA‐rapport 1/2014 Tittel: ISBN: Kystlynghei i Austrheim, Lindås, Radøy, Meland, Øygarden, Fjell og Sund. 978‐82‐8060‐097‐4 Registreringer i 2013 i forbindelse med Handlingsplan for kystlynghei. Forfatter: Dato: Kristine Ekelund 06.02.2014 Sammendrag: Rapporten inneholder supplerende og oppdaterte beskrivelser av ti områder med kystlynghei i kommunene Austrheim, Lindås, Radøy, Meland, Øygarden, Fjell og Sund i Hordaland. Registreringen er initiert og finansiert av Fylkesmannen i Hordaland, og er en del av arbeidet med å dokumentere biologiske kvaliteter og skjøtselstilstand i kystlynghei. Kystlyngheiene er en menneskeskapt naturtype som er i rask endring fordi de ikke lenger er i bruk som tidligere. Mange er i ferd med å gro igjen, og med dette er en bekymret for at mye av kulturhistorien og artssammensetningen som er typisk for slike områder vil forsvinne. Dette er bakgrunnen for at kystlynghei er fremmet som kandidat som utvalgt naturtype etter naturmangfoldloven. I forbindelse med dette er det laget et faggrunnlag for kystlynghei, med forslag til nasjonal handlingsplan der en tar sikte på å ta vare på et utvalg lyngheiområder langs hele norskekysten. Fitjarøyane og Lygra med Lurekalven er foreslått som referanseområder i Hordaland, men en ønsker også å stimulere til drift og skjøtsel av lynghei utenfor de fylkesvise referanseområdene. Kystlynghei i Hordaland er tidligere kartlagt både gjennom nasjonale registreringer og gjennom den kommunevise kartleggingen av viktige naturtyper som har pågått siden 1999. -
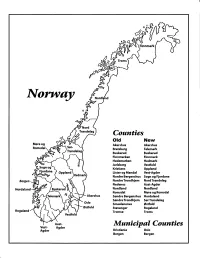
Norway Maps.Pdf
Finnmark lVorwny Trondelag Counties old New Akershus Akershus Bratsberg Telemark Buskerud Buskerud Finnmarken Finnmark Hedemarken Hedmark Jarlsberg Vestfold Kristians Oppland Oppland Lister og Mandal Vest-Agder Nordre Bergenshus Sogn og Fjordane NordreTrondhjem NordTrondelag Nedenes Aust-Agder Nordland Nordland Romsdal Mgre og Romsdal Akershus Sgndre Bergenshus Hordaland SsndreTrondhjem SorTrondelag Oslo Smaalenenes Ostfold Ostfold Stavanger Rogaland Rogaland Tromso Troms Vestfold Aust- Municipal Counties Vest- Agder Agder Kristiania Oslo Bergen Bergen A Feiring ((r Hurdal /\Langset /, \ Alc,ersltus Eidsvoll og Oslo Bjorke \ \\ r- -// Nannestad Heni ,Gi'erdrum Lilliestrom {", {udenes\ ,/\ Aurpkog )Y' ,\ I :' 'lv- '/t:ri \r*r/ t *) I ,I odfltisard l,t Enebakk Nordbv { Frog ) L-[--h il 6- As xrarctaa bak I { ':-\ I Vestby Hvitsten 'ca{a", 'l 4 ,- Holen :\saner Aust-Agder Valle 6rrl-1\ r--- Hylestad l- Austad 7/ Sandes - ,t'r ,'-' aa Gjovdal -.\. '\.-- ! Tovdal ,V-u-/ Vegarshei I *r""i'9^ _t Amli Risor -Ytre ,/ Ssndel Holt vtdestran \ -'ar^/Froland lveland ffi Bergen E- o;l'.t r 'aa*rrra- I t T ]***,,.\ I BYFJORDEN srl ffitt\ --- I 9r Mulen €'r A I t \ t Krohnengen Nordnest Fjellet \ XfC KORSKIRKEN t Nostet "r. I igvono i Leitet I Dokken DOMKIRKEN Dar;sird\ W \ - cyu8npris Lappen LAKSEVAG 'I Uran ,t' \ r-r -,4egry,*T-* \ ilJ]' *.,, Legdene ,rrf\t llruoAs \ o Kirstianborg ,'t? FYLLINGSDALEN {lil};h;h';ltft t)\l/ I t ,a o ff ui Mannasverkl , I t I t /_l-, Fjosanger I ,r-tJ 1r,7" N.fl.nd I r\a ,, , i, I, ,- Buslr,rrud I I N-(f i t\torbo \) l,/ Nes l-t' I J Viker -- l^ -- ---{a - tc')rt"- i Vtre Adal -o-r Uvdal ) Hgnefoss Y':TTS Tryistr-and Sigdal Veggli oJ Rollag ,y Lvnqdal J .--l/Tranbv *\, Frogn6r.tr Flesberg ; \. -

Administrative and Statistical Areas English Version – SOSI Standard 4.0
Administrative and statistical areas English version – SOSI standard 4.0 Administrative and statistical areas Norwegian Mapping Authority [email protected] Norwegian Mapping Authority June 2009 Page 1 of 191 Administrative and statistical areas English version – SOSI standard 4.0 1 Applications schema ......................................................................................................................7 1.1 Administrative units subclassification ....................................................................................7 1.1 Description ...................................................................................................................... 14 1.1.1 CityDistrict ................................................................................................................ 14 1.1.2 CityDistrictBoundary ................................................................................................ 14 1.1.3 SubArea ................................................................................................................... 14 1.1.4 BasicDistrictUnit ....................................................................................................... 15 1.1.5 SchoolDistrict ........................................................................................................... 16 1.1.6 <<DataType>> SchoolDistrictId ............................................................................... 17 1.1.7 SchoolDistrictBoundary ........................................................................................... -

Søknad Om Løyve Til Graving I Offentleg Veg Send Til: [email protected]
Retningsliner for graving i offentlig veg - NKF nettverksgruppe Veg og trafikk Hordaland Søknad om løyve til graving i offentleg veg Send til: [email protected] Etter vedtektene i Veglova §§ 32 og 57 og forskrifter om varsling av arbeid på offentleg veg vert det hermed søkt om løyve til: Legging Utskifting Reparasjon Luftspenn Veg nr.: ______ Hp.: ______ Km: _________-_________ Arbeidsstad: _________________________________________________ Arbeida gjeld: Vassleidning Telekabel Avløpsleidning Anna: ________________ El-kabel Gassleidning TV-kabel Noverande dekke: Asfalt Brostein Grus Anna: ________________ Frå eigedom Gnr.: _________ bnr.:_________ slik det er vist på vedlagde kart / skisse i målestokk 1: 1000 Arbeidsskildring:________________________________________________________________________________________________________________________ ______________________________________________________________________________________________________________________________________ Arbeidet er ønska oppstarta:____________________ og venta avslutta:_______________________ Talet på kryssingar:________ stk. Boring: ja, ved km: _____________ nei Lengde på luftspenn/grøft langs veg: ________ m frå km: ______________ til km: ______________ Som eigar av og oppdragsgjevar/byggherre for anlegget tek eg på meg det ansvaret som ”Retningsliner for graving i offentleg veg – NKF nettverksgruppe Veg og trafikk Hordaland, Oktober 2013” pålegg meg og garanterer for ferdigstilling av anlegget utan kostnad for veghalder. Eg godtek dei vilkår for løyvet som -

Port of Bergen
Cruise Norway The complete natural experience A presentation of Norwegian destinations and cruise ports Cruise Norway Manual 2007/2008 ANGEN R W NNA : GU OTO H Index P Index 2 Presentation of Cruise Norway 2-3 Cruise Cruise Destination Norway 4-5 Norwegian Cruise Ports 6 wonderful Norway Distances in nautical miles 7 The “Norway Cruise Manual” gives a survey of Norwegian harbours Oslo Cruise Port 8 providing excellent services to the cruise market. This presentation is edited in a geographical sequence: It starts in the North - and finishes Drammen 10 in the South. Kristiansand 12 The presentation of each port gives concise information about the most 3 Small City Cruise 14 important attractions, “day” and “halfday” excursions, and useful, practical information about harbour conditions. The amount of information is limited Stavanger 16 due to space. On request, more detailed information may be obtained from Eidfjord 18 Cruise Norway or from the individual ports. The “Norway Cruise Manual” is the only comprehensive overview of Ulvik 20 Norwegian harbours and the cooperating companies that have the Bergen 22 international cruise market as their field of activity. The individual port authorities / companies are responsible for the information which Vik 24 appears in this presentation. Flåm 26 An Early Warning System (EWS) for Norwegian ports was introduced in 2004 Florø 28 - go to: www.cruise-norway.no Olden/Nordfjord 30 T D Geirangerfjord 32 N Y BU Ålesund 34 NANC : Molde/Åndalsnes 36 OTO PH Kristiansund 38 Narvik 40 Møre and Romsdal Lofoten 42 Vesterålen 44 Y WA R NO Harstad 46 ation Tromsø 48 Presenting V INNO Alta 50 .