BMJ Open Is Committed to Open Peer Review. As Part of This Commitment We Make the Peer Review History of Every Article We Publish Publicly Available
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

2016-17 Department: UCL Medical School Faculty: Medical Sciences CONNECTED CURRICULUM
UCL QUALITY REVIEW FRAMEWORK - ANNEX 6.1.3: ASER DEVELOPMENT & ENHANCEMENT PLAN Academic Session: 2016-17 Department: UCL Medical School Faculty: Medical Sciences CONNECTED CURRICULUM Last session, Departments were invited to discuss how they intended to begin their preliminary assessment of their taught provision by benchmarking each programme against the grid in the Connected Curriculum Enhancement Guide. Programmes were asked to evaluate and clearly state where the programme or cluster of similar programmes was benchmarked in relation to each dimension of the Connected Curriculum. In this section, Departments are asked to indicate the extent to which their programme(s) reflect each of the six dimensions, to highlight notable examples of good practice, and (in the Development and Enhancement plan below) to list up to six actions that the department/programme team will now take to enhance the programme(s) over the next two to three years. Departments will then be asked to review progress in relation to these actions in the Autumn 2019 ASER. The broad evaluation of the programme(s) as ‘Beginning’, ‘Developing’, ‘Developed’ or ‘Outstanding’ for each dimension will enable the Department/Programme Leader to track progress in relation to all six dimensions over time. It is intended to be a broadly agreed description of current practice in the programme(s) as a whole. General guidance on interpreting these terms is found on p6-7 of the Connected Curriculum online guide: https://www.ucl.ac.uk/teaching-learning/sites/teaching-learning/files/connected_curriculum_brochure_21_june_2017.pdf Departments may also find the ‘Twenty Questions’ on p10 helpful. If you have a large number of UG programmes in your department, a suggested approach is to use this form to provide a departmental summary of your programmes and then to identify those particular programmes which are excelling or which need more development by completing a form with a summary for each programme (or cluster of very similar programmes). -

Projects Nominated in 2020 UCL Provosts Public Engagement
Projects Nominated in 2020 UCL Provost's Public Engagement Awards Lead UCL Lead external Project Name UCL Department External Organisation Contact Contact A strengths-based approach to autism and employment: Insights, experiences, and Psychology and Human Development, UCL Anna Melissa best practice strategies from the Deutsche Bank UK autistic graduate internship Institute of Education – Centre for Research in Alex Wilson Deutsche Bank Romualdez programme Autism and Education Addressing Infrastructural Vulnerabilities: a participatory spatial intervention in the Andrea Rigon Development Planning Unit Joana Dabaj CatalyticAction refugee-hosting town of Bar Elias, Lebanon Evangelos Beatboxing After Laryngectomy UCL Institute of Education, Department of CCM Thomas Moors Shout at Cancer Himonides Education, Practice and Society, Institute of Building the evidence base for effective policy: the role of education in international Moses Oketch Education, Centre for Education and International Jess Atkinson Department for International Development (DFID) development Development (CEID) Ameenat Lola Childhood rare eyes disease: patient and public involvement and engagement UCL GOS Institute of Child Health Deirdre Leyden GOSH Patient and Public Involvement in Research Lead Solebo Civic Design CPD and Knowledge Exchange: Co-designing Neighbourhoods with Pablo Sendra The Bartlett School of Planning Leslie Barson Granville Community Kitchen Communities Collaborative City Planning Strategies Masters Module BPLN0033 Elena Besussi Bartlett School of -

Review of UCL Medical School
London regional review 2012–13 Review of UCL Medical School This visit is part of a regional review and uses a risk-based approach. For more information on this approach see http://www.gmc- uk.org/education/13707.asp. Review at a glance About the School Programme MBBS University UCL Medical School Years of course 6 Programme structure Year 1 – Fundamentals of clinical science 1 Year 2 – Fundamentals of clinical science 2 Year 3 – Scientific method in depth (iBSc) Year 4 – Integrated clinical care Year 5 – Life cycle Year 6 – Preparation for practice Number of students 1,969 (2011 MSAR) Number of LEPs UCL reported 196 clinical placements across 28 trusts or other providers, excluding GP placements. Local deanery London Deanery Last GMC visit 2004-5 QABME Outstanding actions None from last visit 1 About the visit Visit dates 22-23 November 2012 Sites visited UCL Medical School Areas of exploration MBBS Were any patient No safety concerns identified during the visit? Were any significant No educational concerns identified? Has further regulatory No action been requested via the responses to concerns element of the QIF? Summary 1 London has been chosen as the region for review in 2012-13 and all five London medical schools have been visited as part of this review. The north central regional visit team visited UCL Medical School (the School), a Division in the Faculty of Medical Sciences, University College London, in November 2012. 2 UCL is the third largest medical school in London with 1,969 students. The School has three main clinical campuses: Bloomsbury, the Royal Free and the Whittington. -

Review 2011 1 Research
LONDON’S GLOBAL UNIVERSITY ReviewHighlights 2011 2011 Walking on Mars © Angeliki Kapoglou Over summer 2011, UCL Communications held a The winning entry was by Angeliki Kapoglou (UCL Space photography competition, open to all students, calling for & Climate Physics), who was selected to serve as a member images that demonstrated how UCL students contribute of an international crew on the Mars Desert Research Station, to society as global citizens. The term ‘education for global which simulates the Mars environment in the Utah desert. citizenship’ encapsulates all that UCL does to enable Researchers at the station work to develop key knowledge students to respond to the intellectual, social and personal needed to prepare for the human exploration of Mars. challenges that they will encounter throughout their future careers and lives. The runners-up and other images of UCL life can be seen at: www.flickr.com/uclnews Contents Research 2 Follow UCL news www.ucl.ac.uk Health 5 Insights: a fortnightly email summary Global 8 of news, comment and events: www.ucl.ac.uk/news/insights Teaching & Learning 11 Events calendar: Enterprise 14 www.events.ucl.ac.uk Highlights 2011 17 Twitter: @uclnews UCL Council White Paper 2011–2021 YouTube: UCLTV Community 21 In images: www.flickr.com/uclnews Finance & Investment 25 SoundCloud: Awards & Appointments 30 www.soundcloud.com/uclsound iTunes U: People 36 http://itunes.ucl.ac.uk Leadership 37 UCL – London’s Global University Our vision Our values • An outstanding institution, recognised as one of the world’s -

Ucl Medical School Internal Quality Review
UCL MEDICAL SCHOOL INTERNAL QUALITY REVIEW Contents INTRODUCTION .....................................................................................................................................................4 Regulatory Framework.........................................................................................................................................4 Overview of Educational Organisational Structures ............................................................................................4 Overview of Educational Programmes.................................................................................................................5 SECTION 1. KEY DEVELOPMENTS......................................................................................................................7 1.1 Findings from previous review .......................................................................................................................7 1.2 Progress on implementation of the recommendations ................................................................................10 1.2.1 MBBS ....................................................................................................................................................10 1.2.2 Postgraduate Education ........................................................................................................................13 SECTION 2. STUDENTS, STAFF AND LEARNING RESOURCES.....................................................................15 2.1 Student Profile..............................................................................................................................................15 -

Teaching and Learning in Higher Education Ed
Teaching and Learning in Higher Education Teaching ‘… an admirable testament to UCL’s ambition to foster innovative, evidence-based and thoughtful approaches to teaching and learning. There is much to learn from here.’— Professor Karen O’Brien, Head of the Humanities Division, University of Oxford ‘Research and teaching’ is a typical response to the question, ‘What are universities for?’ For most people, one comes to mind more quickly than the other. Most undergraduate students will think of teaching, while PhD students will think of research. University staff will have similarly varied reactions depending on their roles. Emphasis on one or the other has also changed over time according to governmental incentives and pressure. Davies and Norbert Pachler ed. Jason P. For some decades, higher education has been bringing the two closer together, to the point of them overlapping, by treating students as partners and nding ways of having them learn through undertaking research. Drawing on a range of examples from across the disciplines, this collection demonstrates how one research-rich university, University College London (UCL), has set up initiatives to raise the pro le of teaching and give it parity with research. It explains what staff and students have done to create an environment in which students can learn by discovery, through research- based education. ‘… an exemplary text of its kind, offering much to dwell on to all interested in advancing university education.’— Ronald Barnett, Emeritus Professor of Higher Education, University College London Institute of Education Dr Jason P. Davies is a Senior Teaching Fellow at the UCL Arena Centre. -

UCL MEDICAL SCHOOL Clinical and Professional Practice, Medical Student Administration University College London JOB DESCRIPTION
UCL MEDICAL SCHOOL Clinical and Professional Practice, Medical Student Administration University College London JOB DESCRIPTION Job Title: Clinical and Professional Practice Tutor x 6 Division: UCL Medical School Sub Department: Clinical and Professional Practice, Medical Student Administration Location: Bloomsbury, Royal Free or Whittington Campus Grade: 7 Hours: Part-time and Sessional, mainly on Thursdays and Fridays with some scope for flexibility The MBBS Clinical and Professional Practice Modules The Clinical and Professional Practice (CPP) modules make up almost 20% of the overall MBBS programme. Learning in CPP is central to understanding medicine as an integrated whole. There are 15 CPP modules, each organised over six years: Student centred learning, patient centred learning: 1. Portfolio a. Y1 online submission at end of year b. Y2 online submission at end of year c. Y4 E-portfolio d. Y5 E-portfolio and Case of the Month e. Y6 E-portfolio and Case of the Month Patient Pathways: 2. Integrated and Community Care (Y1) 3. Cardio-metabolic Medicine (Y2) 4. Cancer Medicine (Y4) 5. Person-centred (Y5) Integrated Vertical Strands: 6. Anatomy and Imaging 7. Clinical Skills and Practical Procedures 8. Pathological Sciences 9. Use of Evidence 10. Use of Medicines Overarching Themes: 11. Mental Health Page 1 of 5 12. Social Determinants of Health a. Epidemiology b. Global Health c. Medical Sociology d. Public Health 13. Ethics and Law 14. Clinical Communication 15. Professional Practice a. Professionalism b. E-health The organisation of the CPP is complex, from both an administrative and academic perspective. CPP teaching takes place both as centrally organised and ‘peel off’ activities in dedicated teaching sessions and activities fully integrated into the horizontal modules. -

For Peer Review Only
BMJ Open BMJ Open: first published as 10.1136/bmjopen-2016-013897 on 2 December 2016. Downloaded from “You can’t be a person and a doctor”. The work-life balance of doctors in training: a national qualitative study ForJournal: peerBMJ Open review only Manuscript ID bmjopen-2016-013897 Article Type: Research Date Submitted by the Author: 15-Aug-2016 Complete List of Authors: Rich, Antonia; University College London Medical School, Research Department of Medical Education Viney, Rowena; University College London Medical School, Research Department of Medical Education Needleman, Sarah; University College London Medical School, Research Department of Medical Education Griffin, Ann; University College London, Medical School Woolf, Katherine; University College London, Academic Centre for Medical Education <b>Primary Subject Medical education and training Heading</b>: Secondary Subject Heading: Qualitative research QUALITATIVE RESEARCH, work-life balance, MEDICAL EDUCATION & http://bmjopen.bmj.com/ Keywords: TRAINING, women, gender, medical training on September 24, 2021 by guest. Protected copyright. For peer review only - http://bmjopen.bmj.com/site/about/guidelines.xhtml Page 1 of 86 BMJ Open BMJ Open: first published as 10.1136/bmjopen-2016-013897 on 2 December 2016. Downloaded from 1 2 3 4 “You can’t be a person and a doctor”. The work-life balance of 5 6 doctors in training: a national qualitative study 7 8 9 Dr Antonia Rich, Research Associate1 10 Dr Rowena Viney, Research Associate1 11 Dr Sarah Needleman, Clinical Teaching Fellow1 -

Translational Research Office, UK
Impact Objectives • Use the Therapeutic Innovation Networks (TINs) to harness the translational experience and infrastructure of UCL and its NIHR Biomedical Research Centres to provide education, support and encouragement to early career scientists to translate their novel science • Maximise University College London’s ability to quickly and efficiently translate disease-related discoveries into high-quality therapeutic interventions and tangible treatments for patients • Ensure all TINs have an industry network with the aim of using their know-how and resource to aid the development of the portfolio The innovation game Professor David Lomas discusses the Therapeutic Innovation Networks (TINs), which are facilitating and accelerating enterprise at University College London (UCL), UK Can you begin by commercialising biomedical therapies. These of our national and international standing. introducing yourself? forums are also used to discuss barriers and For example, we have used the TINs to hurdles, and approaches to overcome them. assess our strengths and weaknesses in cell, I am Vice-Provost The Cell, Gene & Regenerative Medicine gene and regenerative therapies, and work (Health) at UCL, Head TIN has been very effective in pulling out how we can collaborate effectively with of the School of Life & the community together and articulating industry and our London partners: King’s Medical Sciences and our strengths in this area. UCL has more College London, Imperial College London Head of the UCL Medical School. I also serve research and clinical activity in the area of cell and Queen Mary University of London. This as the Academic Director of UCL Partners’ and gene therapy than any other university allows for economy of scale, more rapid Academic Health Science Centre and as a in the UK and, indeed, has a clinical portfolio translation and more effective competition Director of The Francis Crick Institute, Africa of comparable size to that of the whole of for research and enterprise income, Health Research Institute, MedCity, Non- Spain or Italy. -

Clinical Lecturer in Paediatrics Job Description
UCL SCHOOL OF LIFE AND MEDICAL SCIENCES UCL FACUTY OF POULATION HEALTH SCIENCES INSTITUTE OF CHILD HEALTH CLINICAL LECTURER IN PAEDIATRICS JOB DESCRIPTION INTRODUCTION The UCL Institute of Child Health (ICH) The mission of the UCL Institute of Child Health is to improve the health and well-being of children, and the adults they will become, through world-class research, education and public engagement. This strategy has been informed by the insights gained from visits to six other internationally excellent children’s academic medical centres and by detailed discussions internally and with our external partners, including GODH, GOSH Children’s Charity, the wider UCL community, UCL Partners and funding bodies. The UCL Institute of Child Health, together with its clinical partner Great Ormond Street Hospital for Children, forms the largest concentration of children’s health research outside North America. In 2013 ICH developed a new academic strategy which focuses on five scientific programmes: • Genetics and Genomic Medicine • Population, Policy and Practice • Developmental Biology and Cancer • Developmental Neurosciences • Infection, Immunity and Inflammation Four key principles underpin these programmes and the academic strategy: Interdisciplinarity. ICH will facilitate the best scientists, from all relevant academic and clinical disciplines, to work together to address fundamental questions to improve the health of children. Accelerating translation. ICH will support the rapid translation of findings from basic discoveries relevant to understanding of health and disease, to clinical studies, more directly aimed at improving the clinical care of children. We will also support “reverse translation” from observations in clinical and population studies to basic studies which address mechanisms of health and disease. -

Business Plan 2017-18
BUSINESS PLAN 2017‐18 1 Contents MedCity Vision and 3-5 year long range view ................................................................................................................................................................ 3 Themes ............................................................................................................................................................................................................................. 6 Organisational Values ...................................................................................................................................................................................................... 6 Action Plan ....................................................................................................................................................................................................................... 7 Key Performance Indicators .......................................................................................................................................................................................... 14 Assumptions................................................................................................................................................................................................................... 25 Risk Plan ....................................................................................................................................................................................................................... -
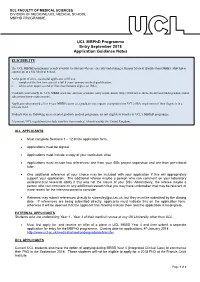
UCL Mbphd Programme Entry September 2018 Application Guidance Notes
UCL FACULTY OF MEDICAL SCIENCES DIVISION OF MEDICINE/UCL MEDICAL SCHOOL MBPHD PROGRAMME UCL MBPhD Programme Entry September 2018 Application Guidance Notes ELIGIBILITY The UCL MBPHD programme is only available to students who are currently undertaking a Primary Medical Qualification (MBBS, MBChB or equivalent) at a UK Medical School. At the point of entry, successful applicants will have: i. completed the first two years of a full 5 years’ primary medical qualification; ii. achieved an upper second or first class honours degree (or iBSc). Candidate must satisfy the UCL MBBS academic and non-academic entry requirements (http://www.ucl.ac.uk/medicalschool/undergraduate/mbbs- admissions/entry-requirements). Applicants who entered a 5 or 6-year MBBS course as a graduate may request exemption from UCL's iBSc requirement if their degree is in a relevant field. Students who are following an accelerated graduate medical programme are not eligible to transfer to UCL’s MBPhD programme. At present, UCL regulations preclude transfers from medical schools outside the United Kingdom. ALL APPLICANTS Must complete Sections 1 – 12 of the application form. Applications must be signed. Applications must include a copy of your curriculum vitae Applications must include two references: one from your iBSc project supervisor and one from pre-clinical tutor. One additional reference of your choice may be included with your application if this will appropriately support your application. The additional referee maybe a person who can comment on your laboratory skills/practical research ability if this was not the nature of your BSc. Alternatively, the referee maybe a person who can comment on any additional research that you may have undertaken that may be relevant or more recent for the interview panel to consider.