Chronic Lymphocytic Leukemia Early Detection, Diagnosis, and Staging Detection and Diagnosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Synchronous Diagnosis of Multiple Myeloma, Breast Cancer, and Monoclonal B-Cell Lymphocytosis on Initial Presentation
Hindawi Publishing Corporation Case Reports in Oncological Medicine Volume 2016, Article ID 7953745, 4 pages http://dx.doi.org/10.1155/2016/7953745 Case Report Synchronous Diagnosis of Multiple Myeloma, Breast Cancer, and Monoclonal B-Cell Lymphocytosis on Initial Presentation A. Vennepureddy,1 V. Motilal Nehru,1 Y. Liu,2 F. Mohammad,3 andJ.P.Atallah3 1 Department of Internal Medicine, Staten Island University Hospital, 475 Seaview Avenue, Staten Island, NY 10305, USA 2Department of Pathology, Staten Island University Hospital, 475 Seaview Avenue, Staten Island, NY 10305, USA 3Division of Hematology and Oncology, Staten Island University Hospital, 475 Seaview Avenue, Staten Island, NY 10305, USA Correspondence should be addressed to A. Vennepureddy; [email protected] Received 20 December 2015; Accepted 24 April 2016 Academic Editor: Su Ming Tan Copyright © 2016 A. Vennepureddy et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. The cooccurrence of more than one oncologic illness in a patient can present a diagnostic challenge. Here we report an unusual case of concomitant existence of multiple myeloma, breast cancer, and monoclonal B-cell lymphocytosis on initial presentation. The challenge was to accurately diagnose each disease and stage in order to maximize the therapeutic regimen to achieve cure/remission. Successful management of the patient and increased life expectancy can be achieved by multidisciplinary management and patient- oriented approach in multiple primary malignant synchronous tumors. 1. Introduction different patterns of MPMs should be considered. Thera- peutically, a multidisciplinary and patient-oriented approach Multiple primary malignant tumors (MPMTs) are rarely should be considered. -

Follicular Lymphoma
Follicular Lymphoma What is follicular lymphoma? Let us explain it to you. www.anticancerfund.org www.esmo.org ESMO/ACF Patient Guide Series based on the ESMO Clinical Practice Guidelines FOLLICULAR LYMPHOMA: A GUIDE FOR PATIENTS PATIENT INFORMATION BASED ON ESMO CLINICAL PRACTICE GUIDELINES This guide for patients has been prepared by the Anticancer Fund as a service to patients, to help patients and their relatives better understand the nature of follicular lymphoma and appreciate the best treatment choices available according to the subtype of follicular lymphoma. We recommend that patients ask their doctors about what tests or types of treatments are needed for their type and stage of disease. The medical information described in this document is based on the clinical practice guidelines of the European Society for Medical Oncology (ESMO) for the management of newly diagnosed and relapsed follicular lymphoma. This guide for patients has been produced in collaboration with ESMO and is disseminated with the permission of ESMO. It has been written by a medical doctor and reviewed by two oncologists from ESMO including the lead author of the clinical practice guidelines for professionals, as well as two oncology nurses from the European Oncology Nursing Society (EONS). It has also been reviewed by patient representatives from ESMO’s Cancer Patient Working Group. More information about the Anticancer Fund: www.anticancerfund.org More information about the European Society for Medical Oncology: www.esmo.org For words marked with an asterisk, a definition is provided at the end of the document. Follicular Lymphoma: a guide for patients - Information based on ESMO Clinical Practice Guidelines – v.2014.1 Page 1 This document is provided by the Anticancer Fund with the permission of ESMO. -

Monoclonal B-Cell Lymphocytosis Is Characterized by Mutations in CLL Putative Driver Genes and Clonal Heterogeneity Many Years Before Disease Progression
Leukemia (2014) 28, 2395–2424 © 2014 Macmillan Publishers Limited All rights reserved 0887-6924/14 www.nature.com/leu LETTERS TO THE EDITOR Monoclonal B-cell lymphocytosis is characterized by mutations in CLL putative driver genes and clonal heterogeneity many years before disease progression Leukemia (2014) 28, 2395–2398; doi:10.1038/leu.2014.226 (Beckton Dickinson) and data analyzed using Cell Quest software. On the basis of FACS (fluorescence-activated cell sorting) analysis, we observed after enrichment an average of 91% of CD19+ cells Monoclonal B-cell lymphocytosis (MBL) is defined as an asympto- (range 76–99%) and 91% of the CD19+ fraction were CD19+/CD5+ matic expansion of clonal B cells with less than 5 × 109/L cells in the cells (range 66–99%). We used the values of the CD19+/CD5+ peripheral blood and without other manifestations of chronic fraction to calculate the leukemic B-cell fraction and reduce any lymphocytic leukemia (CLL; for example, lymphadenopathy, cyto- significant contamination of non-clonal B cells in each biopsy. DNA penias, constitutional symptoms).1 Approximately 1% of the MBL was extracted from the clonal B cells and non-clonal (that is, T cells) cohort develops CLL per year. Evidence suggests that nearly all CLL cells using the Gentra Puregene Cell Kit (Qiagen, Hilden, Germany). 2 fi fi cases are preceded by an MBL state. Our understanding of the Extracted DNAs were ngerprinted to con rm the relationship genetic basis, clonal architecture and evolution in CLL pathogenesis between samples of the same MBL individual and to rule out sample has undergone significant improvements in the last few years.3–8 In cross-contamination between individuals. -

Follicular Lymphoma with Leukemic Phase at Diagnosis: a Series Of
Leukemia Research 37 (2013) 1116–1119 Contents lists available at SciVerse ScienceDirect Leukemia Research journa l homepage: www.elsevier.com/locate/leukres Follicular lymphoma with leukemic phase at diagnosis: A series of seven cases and review of the literature a c c c c Brady E. Beltran , Pilar Quinones˜ , Domingo Morales , Jose C. Alva , Roberto N. Miranda , d e e b,∗ Gary Lu , Bijal D. Shah , Eduardo M. Sotomayor , Jorge J. Castillo a Department of Oncology and Radiotherapy, Edgardo Rebagliati Martins Hospital, Lima, Peru b Division of Hematology and Oncology, Rhode Island Hospital, Brown University Alpert Medical School, Providence, RI, USA c Department of Pathology, Edgardo Rebaglati Martins Hospital, Lima, Peru d Department of Hematopathology, MD Anderson Cancer Center, Houston, TX, USA e Department of Malignant Hematology, H. Lee Moffitt Cancer Center & Research Institute, Tampa, FL, USA a r t i c l e i n f o a b s t r a c t Article history: Follicular lymphoma (FL) is a prevalent type of non-Hodgkin lymphoma in the United States and Europe. Received 23 April 2013 Although, FL typically presents with nodal involvement, extranodal sites are less common, and leukemic Received in revised form 25 May 2013 phase at diagnosis is rare. There is mounting evidence that leukemic presentation portends a worse Accepted 26 May 2013 prognosis in patients with FL. We describe 7 patients with a pathological diagnosis of FL who presented Available online 20 June 2013 with a leukemic phase. We compared our cases with 24 additional cases reported in the literature. Based on our results, patients who present with leukemic FL tend to have higher risk disease. -

Occult B-Lymphoproliferative Disorders Andy Rawstron
Occult B-lymphoproliferative Disorders Andy Rawstron To cite this version: Andy Rawstron. Occult B-lymphoproliferative Disorders. Histopathology, Wiley, 2011, 58 (1), pp.81. 10.1111/j.1365-2559.2010.03702.x. hal-00610748 HAL Id: hal-00610748 https://hal.archives-ouvertes.fr/hal-00610748 Submitted on 24 Jul 2011 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Histopathology Occult B-lymphoproliferative Disorders ForJournal: Histopathology Peer Review Manuscript ID: HISTOP-09-10-0521 Wiley - Manuscript type: Review Date Submitted by the 21-Sep-2010 Author: Complete List of Authors: Rawstron, Andy; St. James's Institute of Oncology, HMDS Chronic Lymphocytic Leukaemia, Non-Hodgkin Lymphoma, Keywords: Monoclonal B-cell Lymphocytosis Published on behalf of the British Division of the International Academy of Pathology Page 1 of 22 Histopathology Occult B-lymphoproliferative Disorders Andy C. Rawstron 1,2 Andy C. Rawstron, PhD Consultant Clinical Scientist HMDS, St. James's Institute of Oncology, Bexley Wing, Beckett Street, Leeds LS9 7TF, UK and HYMS, University of York, YO10 5DD, UK. Contact details: tel +44 113 206 8104, fax +44 113 206 7883, email: [email protected] Peer Review Published on behalf of the British Division of the International Academy of Pathology Histopathology Page 2 of 22 Abstract The term Monoclonal B-lymphocytosis (MBL) was recently introduced to identify individuals with a population of monoclonal B-cells in the absence of other features that are diagnostic of a B-lymphoproliferative disorder. -
Non-Hodgkin's Lymphoma Questions and Answers
Non-Hodgkin's Lymphoma Questions and Answers What is Non-Hodgkin's Lymphoma? Non-Hodgkin’s lymphoma (NHL) is a cancer of the lymphocytes, a type of white blood cell. When lymphocytes become cancerous (malignant), they multiply and become tumors. Lymphocytes are normally found in the blood stream and lymph nodes. Lymph nodes are found throughout the body and are identified by their location. They are a part of the body’s immune system, which includes the lymphatic system, spleen and lymphocytes. Some lymph nodes can be found just by feeling them in the neck, groin or under the arms. Some cannot be felt, but they can be seen on X-rays. NHL is the fifth most common cancer in the United States. Men are at slightly higher risk than women. It is more common in adults than children. The average age at diagnosis is 45 to 55 years. The cause of NHL remains unknown. What Are the Types and Symptoms of Non-Hodgkin’s Lymphoma? There are more than 30 different types of NHL. The specific types of NHL are associated with different symptoms. Low-grade or indolent NHL is usually associated with painless swelling of lymph nodes (usually in the neck or over the collarbone), but patients are otherwise healthy. The swelling may go away for a while, but then return. If the low-grade NHL has spread outside of the lymph nodes, such as to the stomach, there may be discomfort in the affected area. Low-grade lymphomas grow slowly. Examples of low-grade NHLs include: Marginal zone lymphomas. -

Clinical Utility of Recently Identified Diagnostic, Prognostic, And
Modern Pathology (2017) 30, 1338–1366 1338 © 2017 USCAP, Inc All rights reserved 0893-3952/17 $32.00 Clinical utility of recently identified diagnostic, prognostic, and predictive molecular biomarkers in mature B-cell neoplasms Arantza Onaindia1, L Jeffrey Medeiros2 and Keyur P Patel2 1Instituto de Investigacion Marques de Valdecilla (IDIVAL)/Hospital Universitario Marques de Valdecilla, Santander, Spain and 2Department of Hematopathology, MD Anderson Cancer Center, Houston, TX, USA Genomic profiling studies have provided new insights into the pathogenesis of mature B-cell neoplasms and have identified markers with prognostic impact. Recurrent mutations in tumor-suppressor genes (TP53, BIRC3, ATM), and common signaling pathways, such as the B-cell receptor (CD79A, CD79B, CARD11, TCF3, ID3), Toll- like receptor (MYD88), NOTCH (NOTCH1/2), nuclear factor-κB, and mitogen activated kinase signaling, have been identified in B-cell neoplasms. Chronic lymphocytic leukemia/small lymphocytic lymphoma, diffuse large B-cell lymphoma, follicular lymphoma, mantle cell lymphoma, Burkitt lymphoma, Waldenström macroglobulinemia, hairy cell leukemia, and marginal zone lymphomas of splenic, nodal, and extranodal types represent examples of B-cell neoplasms in which novel molecular biomarkers have been discovered in recent years. In addition, ongoing retrospective correlative and prospective outcome studies have resulted in an enhanced understanding of the clinical utility of novel biomarkers. This progress is reflected in the 2016 update of the World Health Organization classification of lymphoid neoplasms, which lists as many as 41 mature B-cell neoplasms (including provisional categories). Consequently, molecular genetic studies are increasingly being applied for the clinical workup of many of these neoplasms. In this review, we focus on the diagnostic, prognostic, and/or therapeutic utility of molecular biomarkers in mature B-cell neoplasms. -

MINI-REVIEW Large Cell Lymphoma Complicating Persistent Polyclonal B
Leukemia (1998) 12, 1026–1030 1998 Stockton Press All rights reserved 0887-6924/98 $12.00 http://www.stockton-press.co.uk/leu MINI-REVIEW Large cell lymphoma complicating persistent polyclonal B cell lymphocytosis J Roy1, C Ryckman1, V Bernier2, R Whittom3 and R Delage1 1Division of Hematology, 2Department of Pathology, Saint Sacrement Hospital, 3Division of Hematology, CHUQ, Saint Franc¸ois d’Assise Hospital, Laval University, Quebec City, Canada Persistent polyclonal B cell lymphocytosis (PPBL) is a rare immunoglobulin (Ig) M with a polyclonal pattern on protein lymphoproliferative disorder of unclear natural history and its electropheresis. Flow cytometry cell analysis displays the pres- potential for B cell malignancy remains unknown. We describe the case of a 39-year-old female who presented with stage IV- ence of the CD19 antigen and surface IgM with a normal B large cell lymphoma 19 years after an initial diagnosis of kappa/lambda ratio. In contrast to CLL, CD5 is absent. There PPBL; her disease was rapidly fatal despite intensive chemo- is an association between HLA-DR 7 and PPBL in more than therapy and blood stem cell transplantation. Because we had two-thirds of the patients but the reason for such an associ- recently identified multiple bcl-2/lg gene rearrangements in ation remains unclear.3,6 There has been one report of PPBL blood mononuclear cells of patients with PPBL, we sought evi- occurring in identical female twins.7 No other obvious genetic dence of this oncogene in this particular patient: bcl-2/lg gene rearrangements were found in blood mononuclear cells but not predisposition or familial inheritance has yet been described in lymphoma cells. -
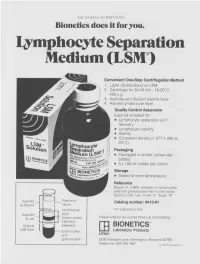
Lymphocyte Separation Medium (LSM
THE JOURNAL OF IMMUNOLOGY Bionetics does it for you. Lymphocyte Separation Medium (LSM wenient One-Step Centrifugation Method _ayer diluted blood on LSM. 2,entrifuge for 30-40 min., 18-20°C, ~.00 x g. ~,spirate and discard plasma layer -larvest lymphocyte layer. Quality Control Assurance Each lot is tested for: • Lymphocyte separation and recovery. • Lymphocyte viability. • Sterility. • Consistent density (1.077-1.080 at 20°C). Packaging • Packaged in amber, screw-cap bottles. • 5 x 100 ml bottles per carton. Storage. • Stored at room temperature. Reference Boyum, A. (1968): Isolation of mononuclear cells and granulocytes from human blood. Scand J. Clin. Lab. Invest. 21, Suppl. 97. Aspirate I IC[OI I IC~ LJI Catalog number: 8410-01 & discard serum Lymphocyte For Laboratory Use Aspirate layer & use (mononuclear Please write for our current Price List and Catalog. cells and Original platelets) ITi BIONETICS° LSM layer Erythrocytes Laboratory Products and Litton granulocytes 5516 Nicholson Lane, Kensington, Maryland 20795 Telephone: (301) 881-1557 1979 Litton Bionetics, tnc Get the most out of your high quality cytotoxic antibodies with LOW-TOX-M RABBIT COMPLEMENT LOW TOXICITY HIGH ACTIVITY Presentation: CL 3051 5 x 1 ml, lyophilized $30.00 When it comes to COMPLEMENT... come to CEDARLANE Direct orders or inquiries to: UNITED STATES: WORLDWIDE EXCEPT U.S. ,4 C~L CEDARLANE ACCURATE CHEMICAL & LABORATO RI ES SCIENTIFIC CORPORATION LIMITED 5516-8TH LINE, R.R. 2 28 TEC STREET, HICKSVtLLE, N.Y. 11801 HORNBY, ONTARIO, CANADA LOP 1E0 Telephone -

Stress and the Immune System Tracy B
4 World Health • 47th Yeor, No. 2, Morch-Aprill994 Stress and the immune system Tracy B. Herbert any people have the effects of factors as diverse as experienced the examinations, bereavement, divorce, Mconnection between stress unemployment, mental arithmetic, and getting sick. Colds, influenza, and looking after a relative with herpes and allergies seem worse Alzheimer's di sease. In general, when we are severely stressed at these studies find that stress is work or in the home. Others are related to changes in both the never sick until they go on vacation numbers of white blood cells in (that is, after the stress is over), and circulation and the quantity of then they spend the whole time antibody in the blood. Moreover, fighting the virus. Because of stress is associated with changes in intrinsic connections like these, the functioning of immune cells. many researchers are today That is, there is a relatively large exploring whether (and how) stress decrease in both lymphocyte and illness are actually linked. One proliferation and natural killer cell specific focus of this research is to activity in individuals who have study the effects of stress on the experienced stress. There seems to immune systems; after all, if stress A lymphocyte: stress may weaken the capacity be some connection between the affects immunity, that would be one of lymphocytes to combat infection. duration of the stress and the amount way in which stress could contribute of immune change. For example, the to illness. longer the stress, the greater the The function of the immune proliferation"- by incubating these decrease in the number of specific system is to protect us from cells for several days with types of white blood cells. -

Association Between Neutrophil-Lymphocyte Ratio and Herpes Zoster Infection in 1688 Living Donor Liver Transplantation Recipients at a Large Single Center
biomedicines Article Association between Neutrophil-Lymphocyte Ratio and Herpes Zoster Infection in 1688 Living Donor Liver Transplantation Recipients at a Large Single Center Ji-Hoon Sim, Young-Jin Moon, Sung-Hoon Kim, Kyoung-Sun Kim , Ju-Seung Lee, Jun-Gol Song * and Gyu-Sam Hwang Department of Anesthesiology and Pain Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul 05505, Korea; [email protected] (J.-H.S.); [email protected] (Y.-J.M.); [email protected] (S.-H.K.); [email protected] (K.-S.K.); [email protected] (J.-S.L.); [email protected] (G.-S.H.) * Correspondence: [email protected]; Tel.: +82-2-3010-3869 Abstract: Liver transplantation (LT) is closely associated with decreased immune function, a contrib- utor to herpes zoster (HZ). However, risk factors for HZ in living donor LT (LDLT) remain unknown. Neutrophil-lymphocyte ratio (NLR) and immune system function are reportedly correlated. This study investigated the association between NLR and HZ in 1688 patients who underwent LDLT between January 2010 and July 2020 and evaluated risk factors for HZ and postherpetic neuralgia (PHN). The predictive power of NLR was assessed through the concordance index and an integrated discrimination improvement (IDI) analysis. Of the total cohort, 138 (8.2%) had HZ. The incidence of HZ after LT was 11.2 per 1000 person-years and 0.1%, 1.3%, 2.9%, and 13.5% at 1, 3, 5, and 10 years, Citation: Sim, J.-H.; Moon, Y.-J.; Kim, respectively. In the Cox regression analysis, preoperative NLR was significantly associated with HZ S.-H.; Kim, K.-S.; Lee, J.-S.; Song, J.-G.; (adjusted hazard ratio [HR], 1.05; 95% confidence interval [CI], 1.02–1.09; p = 0.005) and PHN (HR, Hwang, G.-S. -

Agammaglobulinemia Hypogammaglobulinemia Hereditary Disease Immunoglobulins
Pediat. Res. 2: 72-84 (1968) Agammaglobulinemia hypogammaglobulinemia hereditary disease immunoglobulins Hereditary Alterations in the Immune Response: Coexistence of 'Agammaglobulinemia', Acquired Hypogammaglobulinemia and Selective Immunoglobulin Deficiency in a Sibship REBECCA H. BUCKLEY[75] and J. B. SIDBURY, Jr. Departments of Pediatrics, Microbiology and Immunology, Division of Immunology, Duke University School of Medicine, Durham, North Carolina, USA Extract A longitudinal immunologic study was conducted in a family in which an entire sibship of three males was unduly susceptible to infection. The oldest boy's history of repeated severe infections be- ginning in infancy and his marked deficiencies of all three major immunoglobulins were compatible with a clinical diagnosis of congenital 'agammaglobulinemia' (table I, fig. 1). Recurrent severe in- fections in the second boy did not begin until late childhood, and his serum abnormality involved deficiencies of only two of the major immunoglobulin fractions, IgG and IgM (table I, fig. 1). This phenotype of selective immunoglobulin deficiency is previously unreported. Serum concentrations of the three immunoglobulins in the youngest boy (who also had a late onset of repeated infection) were normal or elevated when he was first studied, but a marked decline in levels of each of these fractions was observed over a four-year period (table I, fig. 1). We could find no previous reports describing apparent congenital and acquired immunologic deficiencies in a sibship. Repeated infections and demonstrated specific immunologic unresponsiveness preceded gross ab- normalities in the total and fractional gamma globulin levels in both of the younger boys (tables II-IV). When the total immunoglobulin level in the second boy was 735 mg/100 ml, he failed to respond with a normal rise in titer after immunization with 'A' and 'B' blood group substances, diphtheria, tetanus, or Types I and II poliovaccines.