Vol 8, No 4 April 2016 ISSN 2072-1439 Indexed in Pubm Ed
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

THE OHIO STATE UNIVERSITY Dean's List AUTUMN SEMESTER 2016 Australia Data As of January 19, 2017 Sorted by Zip Code, City and Last Name
THE OHIO STATE UNIVERSITY Dean's List AUTUMN SEMESTER 2016 Australia Data as of January 19, 2017 Sorted by Zip Code, City and Last Name Student Name (Last, First, Middle) City State Zip Bailey, Meg Elizabeth Merewether 2291 Caudle, Emily May Canberra 2609 Davis, Sarah Kate Canberra 2615 Thek, Hannah Louise Surrey Hills 3127 Engel, Rachel Olivia Glen Iris 3146 Taig, Darcy Lachlan Melbourne 3166 THE OHIO STATE UNIVERSITY Enrollment Services - Analysis and Reporting January 19, 2017 Page 1 of 119 Contact: [email protected] THE OHIO STATE UNIVERSITY Dean's List AUTUMN SEMESTER 2016 Bangladesh Data as of January 19, 2017 Sorted by Zip Code, City and Last Name Student Name (Last, First, Middle) City State Zip Bari, Rizvi Dhaka 1215 THE OHIO STATE UNIVERSITY Enrollment Services - Analysis and Reporting January 19, 2017 Page 2 of 119 Contact: [email protected] THE OHIO STATE UNIVERSITY Dean's List AUTUMN SEMESTER 2016 Brazil Data as of January 19, 2017 Sorted by Zip Code, City and Last Name Student Name (Last, First, Middle) City State Zip Rodrigues Franklin, Ana Beatriz Rio de Janeiro 22241 Gomes Pereira Painhas, Henrique Curitiba 80240 Sprintzin, Leonardo Curitiba 80240 Missell, Daniel Caxias do Sul 95020 THE OHIO STATE UNIVERSITY Enrollment Services - Analysis and Reporting January 19, 2017 Page 3 of 119 Contact: [email protected] THE OHIO STATE UNIVERSITY Dean's List AUTUMN SEMESTER 2016 Canada Data as of January 19, 2017 Sorted by Zip Code, City and Last Name Student Name (Last, First, Middle) City State Zip Lu, George Shizhou Vancouver -

Representing Talented Women in Eighteenth-Century Chinese Painting: Thirteen Female Disciples Seeking Instruction at the Lake Pavilion
REPRESENTING TALENTED WOMEN IN EIGHTEENTH-CENTURY CHINESE PAINTING: THIRTEEN FEMALE DISCIPLES SEEKING INSTRUCTION AT THE LAKE PAVILION By Copyright 2016 Janet C. Chen Submitted to the graduate degree program in Art History and the Graduate Faculty of the University of Kansas in partial fulfillment of the requirements for the degree of Doctor of Philosophy. ________________________________ Chairperson Marsha Haufler ________________________________ Amy McNair ________________________________ Sherry Fowler ________________________________ Jungsil Jenny Lee ________________________________ Keith McMahon Date Defended: May 13, 2016 The Dissertation Committee for Janet C. Chen certifies that this is the approved version of the following dissertation: REPRESENTING TALENTED WOMEN IN EIGHTEENTH-CENTURY CHINESE PAINTING: THIRTEEN FEMALE DISCIPLES SEEKING INSTRUCTION AT THE LAKE PAVILION ________________________________ Chairperson Marsha Haufler Date approved: May 13, 2016 ii Abstract As the first comprehensive art-historical study of the Qing poet Yuan Mei (1716–97) and the female intellectuals in his circle, this dissertation examines the depictions of these women in an eighteenth-century handscroll, Thirteen Female Disciples Seeking Instructions at the Lake Pavilion, related paintings, and the accompanying inscriptions. Created when an increasing number of women turned to the scholarly arts, in particular painting and poetry, these paintings documented the more receptive attitude of literati toward talented women and their support in the social and artistic lives of female intellectuals. These pictures show the women cultivating themselves through literati activities and poetic meditation in nature or gardens, common tropes in portraits of male scholars. The predominantly male patrons, painters, and colophon authors all took part in the formation of the women’s public identities as poets and artists; the first two determined the visual representations, and the third, through writings, confirmed and elaborated on the designated identities. -

Postmen in the Mountains
POSTMEN IN THE MOUNTAINS Running time (90 Min.), "in Mandarin with English subtitles," Distributor Contact: Publicist: Ken Eisen Sharon Kitchens Shadow Distribution SKpr, LLC. P.O. Box 1246 P.O. Box 254 Waterville, ME 04903 Camden, ME 04843 ph (207) 872-5111 ph (207) 596.5686 fax (207) 872-5502 mobile (207) 542.3723 [email protected] [email protected] www.shadow distribution.com http://www.prcmovie.com/postmen/ Best Film-Montreal World Film Festival Audience Award-Maine International Film Festival Best Pictures, Best Director, Best Actor-Golden Rooster Awards (China) Best Foreign Film-Japanese Academy 1 CREDITS CREW Director: Huo Jianqi Screenplay: Si Wu Based on a Short Story by Peng Jianming Producers: Kang Jianmin, Han Sanping Cinematography: Zhao Lei Art: Song Jun Music: Wang Xiaofeng Advisors: Liu Liqing, Zheng Maoqing, Lin Mingtai, Ding Laiwen Supervisors: Ouyang Changlin, Shi Jiuhui, Li Xiaogeng Planning: Pan Yichen, Shi Dongming, Zhou Peixue Executive Producer: Li Chunhua CAST Teng Lujan.......Father Liu Ye....Son Gong Yehong....Grandmother Chen Hao....Dong Girl 2 THE STORY Father (Teng Rujun) has been a postman all his life. His job is to deliver mail to the remote mountain areas of Hunan, China by foot. He is in his late 40s. But now, poor health is forcing him to retire. He cannot trust anyone else but his son (Liu Ye) to take over the job. The morning comes that Son is ready for his first trip as a postman. It's going to be a 3-day trip., 122 kilometers, as it always is. Father cannot rest easy, ans insists that heill come along, knowing the importance of his job, and not quite able to give it up. -
Historical Background of Wang Yang-Ming's Philosophy of Mind
Ping Dong Historical Background of Wang Yang-ming’s Philosophy of Mind From the Perspective of his Life Story Historical Background of Wang Yang-ming’s Philosophy of Mind Ping Dong Historical Background of Wang Yang-ming’s Philosophy of Mind From the Perspective of his Life Story Ping Dong Zhejiang University Hangzhou, Zhejiang, China Translated by Xiaolu Wang Liang Cai School of International Studies School of Foreign Language Studies Zhejiang University Ningbo Institute of Technology Hangzhou, Zhejiang, China Zhejiang University Ningbo, Zhejiang, China ISBN 978-981-15-3035-7 ISBN 978-981-15-3036-4 (eBook) https://doi.org/10.1007/978-981-15-3036-4 © The Editor(s) (if applicable) and The Author(s) 2020. This book is an open access publication. Open Access This book is licensed under the terms of the Creative Commons Attribution- NonCommercial-NoDerivatives 4.0 International License (http://creativecommons.org/licenses/by-nc- nd/4.0/), which permits any noncommercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if you modified the licensed material. You do not have permission under this license to share adapted material derived from this book or parts of it. The images or other third party material in this book are included in the book’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the book’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. -

THE OHIO STATE UNIVERSITY Dean's List AUTUMN SEMESTER 2014 Armenia Sorted by Zip Code, City and Last Name
THE OHIO STATE UNIVERSITY Dean's List AUTUMN SEMESTER 2014 Armenia Sorted by Zip Code, City and Last Name Student Name (Last, First, Middle) City State Zip Wang, Aoning Columbus 43202 THE OHIO STATE UNIVERSITY Enrollment Services - Analysis and Reporting June 21, 2016 Page 1 of 100 Contact: [email protected] THE OHIO STATE UNIVERSITY Dean's List AUTUMN SEMESTER 2014 Australia Sorted by Zip Code, City and Last Name Student Name (Last, First, Middle) City State Zip Davis, Sarah Kate Dunlop 2615 McCallum, Harrison John Gold Coast 4218 THE OHIO STATE UNIVERSITY Enrollment Services - Analysis and Reporting June 21, 2016 Page 2 of 100 Contact: [email protected] THE OHIO STATE UNIVERSITY Dean's List AUTUMN SEMESTER 2014 Bahamas Sorted by Zip Code, City and Last Name Student Name (Last, First, Middle) City State Zip Delancy, Lesa Nassau N7018 THE OHIO STATE UNIVERSITY Enrollment Services - Analysis and Reporting June 21, 2016 Page 3 of 100 Contact: [email protected] THE OHIO STATE UNIVERSITY Dean's List AUTUMN SEMESTER 2014 Brazil Sorted by Zip Code, City and Last Name Student Name (Last, First, Middle) City State Zip Kenny, Phillipe John Dalledone Curitiba 80540 Franzoni Ereno, Gustavo Curitiba 81200 THE OHIO STATE UNIVERSITY Enrollment Services - Analysis and Reporting June 21, 2016 Page 4 of 100 Contact: [email protected] THE OHIO STATE UNIVERSITY Dean's List AUTUMN SEMESTER 2014 Bulgaria Sorted by Zip Code, City and Last Name Student Name (Last, First, Middle) City State Zip Boyadzhiev, Kristian Daniel Sofia 1700 THE OHIO STATE UNIVERSITY -

Understanding Chinese Consumers: Growth Engine of the World Special Edition
China consumer report 2021 Understanding Chinese Consumers: Growth Engine of the World Special edition 2020 November 2020 China consumer report 2021 Understanding Chinese Consumers: Growth Engine of the World Special edition Chief editors: Daniel Zipser, Felix Poh Authors: Antonio Achille, Caleb Balloch, Lambert Bu, Cherry Chen, Guang Chen, Lucille Chen, Will Enger, Johnny Ho, Xin Huang, Daniel Hui, Dymfke Kuijpers, Nick Leung, Lavonda Li, Joanna Mak, Joe Ngai, Felix Poh, David Pountney, Alex Sawaya, Steve Saxon , Jeongmin Seong, Sha Sha, Kay Tu, Jonathan Woetzel, Chenan Xia, Lei Xu, Hai Ye, Jackey Yu, Stefano Zerbi, Cherie Zhang, Jia Zhou, Daniel Zipser Managing editors: Glenn Leibowitz, Lin Lin, Zhijuan Lu Project management: Johnny Ho, Kay Tu, Pauline Chen, Hao Xu, Chloe Chan Copyright © 2020 McKinsey & Company China consumer report 2021 Understanding Chinese Consumers: Growth Engine of the World Special edition 2 China consumer report 2021 Contents Foreword 5 China: Still the world’s growth engine after COVID-19 Revving the engine: The COVID-19 impact 8 Fast forward China: How COVID-19 is accelerating 5 key 10 trends shaping the Chinese economy How COVID-19 has changed Chinese consumption 34 How Chinese consumers are changing shopping habits in 44 response to COVID-19 Winning the future of grocery retail in China 56 What can other countries learn from China’s travel recovery 68 path? A perspective on luxury goods companies during and after 80 coronavirus The driver’s seat: Leadership perspectives 88 Leading through a crisis: How McDonald’s -
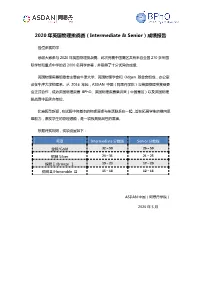
2020 年英国物理挑战赛(Intermediate & Senior)成绩报告
2020 年英国物理挑战赛(Intermediate & Senior)成绩报告 各位参赛同学: 感谢大家参与 2020 年英国物理挑战赛。此次竞赛中国赛区共有来自全国 270 多所国 际学校和重点中学的近 2000 名同学参赛,并取得了十分优异的成绩。 英国物理奥赛组委会主要由牛津大学、英国物理学会和 Odgen 基金会组成,办公室 设在牛津大学物理系。从 2016 年起,ASDAN 中国(阿思丹学院)与英国物理奥赛组委 会正式合作,成为英国物理奥赛 BPhO、英国物理奥赛集训营(中国赛区)以及英国物理 挑战赛中国承办单位。 比赛题型新颖,在试题中将基本的物理原理与生活联系在一起,旨在拓展学生的横向思 维能力,激发学生的物理潜能,是一项极具挑战性的赛事。 根据评奖规则,奖项设置如下: 奖项 Intermediate 分数线 Senior 分数线 金牌/Gold 32 – 50 26 – 50 银牌 Silver 24 – 31 21 – 25 铜牌Ⅰ/Bronze Ⅰ 19 – 23 17 – 20 铜牌Ⅱ/Honorable Ⅱ 15 – 18 12 – 16 ASDAN 中国(阿思丹学院) 2020 年 5 月 附件:2020 年英国物理挑战赛(Intermediate & Senior)获奖名单 Intermediate Name School Award YANWEN GU Nanjing Foreign Language School Gold YUZHOU YANG Nanjing Foreign Language School Gold LOK YAT Shanghai High School International Division Gold HARRISON CHAN XUERUI HE No.2 High School of East China Normal University Gold ZIHAN WANG Shenzhen College of International Education Gold ZHAOCHENG LU Shanghai High School International Division Gold CHENXU LYU YK PAO SCHOOL Gold JIARUI CAI United World College Of Changshu China Gold CHENGYUN ZHU Hefei No.6 High School Gold NANJING NORMAL UNIVERSITY SUZHOU SICHENG MA Gold EXPERIMENTAL SCHOOL RONG GUAN Guanghua Cambridge International School Gold ZIYANG WANG Shenzhen College of International Education Gold QINGCHUAN CHEN Shenzhen College of International Education Gold ZHAOCONG YUAN Shenzhen College of International Education Gold QIANSHUO YE Shenzhen College of International Education Gold The Experimental High School Attached to Beijing Normal XIANGYAN JIN Gold University ANQI YUAN Beijing National Day -

Clinical Guide to Commonly Used Chinese Herbal Formulas
CLINICAL GUIDE TO COMMONLY USED CHINESE HERBAL FORMULAS i John Scott, DOM Lorena Monda, DOM John Heuertz, DOM 6th Edition (2nd printing) 2017 Herbal Medicine Press Copyright: 2017, 2014, 2011, 2009, 2006, 1999, 1997, 1995 Herbal Medicine Press PO Box 781 Placitas, New Mexico 87043 The information in this book is strictly educational and should not be used to treat medical conditions except by knowledgeable health practitioners. ii TABLE OF CONTENTS Pinyin Table of Contents . ix The Formulas: Agastache Tummy Syrup . 1 (Huo Xiang Zheng Qi Gao) Amber Stone-Transforming Formula . 2 (Hu Po Hua Shi Pian) Andrographis Formula . 3 (Chuan Xin Lian Kang Yan Pian) An Mien Formula . 4 (An Mien Pian) Astragalus Formula . 5 (Huang Qi Jian Zhong Tang) Astragalus & Ligustrum Formula . 6 (Huang Qi Dong Qing Pian) Baked Licorice Formula . 7 (Zhi Gan Cao Tang) Blood Palace Formula . 8 (Xue Fu Zhu Yu Tang) Bone & Sinew Formula . 9 (Zheng Gu Xu Jin Fang) Bupleurum & Cinnamon Formula . 10 (Chai Hu Gui Zhi Tang) Bupleurum & Tang Kuei Formula . 11 (Xiao Yao San) Bupleurum D Formula . 12 (Chai Hu Jia Long Gu Mu Li Tang) Capillaris Forumula . 13 (Yin Chen Hao Fang) Chai Hu Shu Gan Formula . 14 (Chai Hu Shu Gan Tang) Chase Wind, Penetrate Bone Formula . 16 (Zhui Feng Tou Gu Wan) Children’s Clear & Release Formula . 17 (Yin Qiao Gan Mao Fang) Children’s Clear Lung Formula . 19 (Xiao Er Zi Qing Fei Fang) Children’s Ear Formula . 20 (Hai Er Fang) Children’s Jade Defense Formula . 21 (Xiao Er Zi Yu Fang) Chong Release Formula . 22 (Jia Wei Tao Hong Si Wu Tong) iii Cinnamon & Poria Formula . -
A Study on Status and Related Measures of Small Medium Enterprises' Technological Innovation
2011 International Conference on Management and Service Science (MASS 2011) Wuhan, China 12-14 August 2011 Pages 1-829 IEEE Catalog Number: CFP1141H-PRT ISBN: 978-1-4244-6579-8 1/7 TABLE OF CONTENTS A STUDY ON STATUS AND RELATED MEASURES OF SMALL MEDIUM ENTERPRISES’ TECHNOLOGICAL INNOVATION ..............................................................................................................................................................1 Yi Su, Bai-Zhou Li ANALYZING COMPLEXITY OF ENTERPRISE PRODUCTION SYSTEM BASED ON CAS THEORY ........................................5 Junwei Zhang, Xiuquan Deng, Bing Bai, Dehua Gao FORECAST ON SHANGHAI’S INPUT-INTENSITY OF R&D BASED ON THE MODEL DGM (1, 1).............................................9 Bin Hu, Yinglin Qin THE EVALUATION OF THE CONSTRUCTION DEGREE OF DALIAN’ TECHNOLOGY INNOVATION SYSTEM BASED ON FUZZY BORDA METHOD.....................................................................................................................................13 Lijie Sun A STUDY ON THE CONSUMPTIVE BEHAVIOR OF INNOVATIVE PROPERTY SERVICES PRODUCTS - BASED ON THE CONSTRUCTION OF TWO-ORIENTATED COMMUNITY...................................................................................17 Miao Yue INFLUENCE OF FAMILY RELATIONSHIPS ON FAMILY BUSINESS SUCCESSION: A CONCEPTUAL MODEL .............................................................................................................................................................................................................22 Xiaoting Wang, -

2021 First Quarterly Results Announcement
Hong Kong Exchanges and Clearing Limited and The Stock Exchange of Hong Kong Limited take no responsibility for the contents of this announcement, make no representation as to its accuracy or completeness and expressly disclaim any liability whatsoever for any loss howsoever arising from or in reliance upon the whole or any part of the contents of this announcement. Linekong Interactive Group Co., Ltd. 藍港互動集團有限公司 (Incorporated in the Cayman Islands with limited liability) (Stock Code: 8267) 2021 FIRST QUARTERLY RESULTS ANNOUNCEMENT The board of directors (the “Board”) of Linekong Interactive Group Co., Ltd. (the “Company”) is pleased to announce the unaudited results of the Company and its subsidiaries for the three months ended March 31, 2021. This announcement, containing the full text of the 2021 first quarterly report of the Company, complies with the relevant requirements of the Rules Governing the Listing of Securities on the GEM of The Stock Exchange of Hong Kong Limited in relation to information to accompany preliminary announcement of quarterly results. Printed version of the Company’s 2021 first quarterly report will be delivered to the shareholders of the Company in due course. By order of the Board Linekong Interactive Group Co., Ltd. WANG Feng Chairman Beijing, the PRC, May 14, 2021 As at the date of this announcement, the executive directors of the Company are Mr. WANG Feng, Ms. LIAO Mingxiang, Mr. CHEN Hao and Mr. WANG Jin (also known as YAN Yusong); the non-executive director of the Company is Mr. JI Xuefeng; and the independent non-executive directors of the Company are Ms. -

Meeting Materials
APPENDIX F: EXAMINATION SINGLE HERB LIST Herbs included on this list will provide the basis for single herb questions used on the examination. Herb nomenclature are taken from Chen and Chen's Chinese Medical Herbology and Pharmacology, 2004 and Bensky, Clavey, and Stoger's Chinese Herbal Medicine: Materia Medica, 2004. These herbs are listed in the reference materials, but are not endorsed as safe by the Department of Consumer Affairs, the Acupuncture Board, or the Federal Food and Drug Administration. PINYIN CHINESE (KOREAN) LATIN PHARMACEUTICAL Ai Ye 3tJl (OH~) Artemisiae Argyi, Folium Ba Ji Tian S'1~ (ll~9~) Morindae Officinalis, Radix 1 Bai Bian Dou BIili (~¥:!~) Lab/ab Semen album Bai Bu a~ (~¥) Stemonae, Radix Bai Guo B~ (~.i11-) Ginkgo, Semen Bai He a~ (~ti°) Li/ii, Bu/bus Bai Jiang Cao fflt9¥ (IIH~~) Patriniae, Herba cum Radice Bai Jie Zi B3f-r (7HX~) Sinapis, Semen Bai Mao Gen B~ffi (~£2) Imperatae, Rhizoma Bai Qian Bw.f (~~) Cynanchi Stauntonii, Radix et Rhizoma Bai Shao B~ (~~) Paeoniae Alba, Radix\ Bai Tou Weng a.:•<~~~> Pulsatillae, Radix Bai Wei Cynanchi Atrati, Radix et Rhizoma s• <~ □ I> Bai Zhi B~ (~XI) Angelicae Dahuricae, Radix Bai Zhu sJtt (~~> Atractylodis Macrocephalae, Rhizoma Bai Zi Ren ~=fi= (~X~<2J) Platycladi, Semen Ban Lan Gen ~Effi (~Etc) lsatidis, Radix Ban Xia Pinelliae, Rhizoma ~- (~c5"~) BeiMu st -BJ (IIff £) Fritillariae, Bu/bus Bei Sha Shen :ftzJ>~ (~N~) Glehniae, Radix BiBo1 Piperis Longi, Fructus -~ (ilW") BianXu •• (¥:!~) Polygoni Avicularis, Herba Trionycis, ·Carapax Bie Jia •Efl (~U) Bo He • fsii -

ANNUAL REPORT Contents
2015 ANNUAL REPORT Contents Corporate Information 2 Chairman’s Statement 4 Company Structure 5 Management Discussion and Analysis 6 Corporate Governance Report 12 Directors and Senior Management 22 Report of the Directors 29 Independent Auditor’s Report 40 Consolidated Statement of Profit or Loss 42 Consolidated Statement of Profit or Loss and Other Comprehensive Income 43 Consolidated Statement of Financial Position 44 Consolidated Statement of Changes in Equity 46 Consolidated Cash Flow Statement 47 Notes to the Consolidated Financial Statements 48 Financial Summary 100 Corporate Information Board of Directors and Committees Board of Directors Committees Executive Directors Audit Committee Mr. Chen Cunyou (Chairman) Mr. Lau Ying Kit (Chairman) Mr. Ge Hongbing Mr. Cheung Man Sang Mr. Zhang Shulin Non-Executive Directors Mr. Lin Lei Mr. Han Yonggui (Vice Chairman) Mr. Li Xuejun Nomination Committee Mr. Zhu Zhenghua Mr. Zhang Shulin (Chairman) Mr. Chen Hao Mr. Lau Ying Kit Mr. Huang Yugang Mr. Cheung Man Sang Mr. Lin Lei Independent Non-Executive Directors Mr. Lau Ying Kit Remuneration Committee Mr. Cheung Man Sang Mr. Cheung Man Sang (Chairman) Mr. Zhang Shulin Mr. Lau Ying Kit Mr. Lin Lei Mr. Zhang Shulin Mr. Lin Lei Other Corporate Information Authorised Representatives Company Secretary Mr. Chen Cunyou Mr. Chui Wing Fai, CPA Mr. Dai Zumian (alternate to Chen Cunyou) Mr. Chui Wing Fai Registered Office c/o Maples Corporate Services Limited Headquarters in the PRC PO Box 309, Ugland House 389 Kening Road Science Park Grand Cayman, KY1-1104,