Ebola Virus Disease
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

DR Congo: Volcanic Eruption in Goma Situation Report #15 08 June 2021
DR Congo: Volcanic eruption in Goma Situation Report #15 08 June 2021 This report is produced by OCHA DRC in collaboration with humanitarian partners. It covers the period of June 08, 2021 (4pm Goma time).1 As of 09 June, the Situation Report will be issued on weekly basis, and in French. The next Situation Report will be published on Monday, 14 June 2021. HIGHLIGHTS • Return of displaced people from Sake towards Goma begins • Process of identification by the authorities of temporary relocation area Displaced people in Sake board a transport provided by the government to facilitate their return to Goma. 08 June, OCHA/Nadege Nodji SITUATION OVERVIEW On 08 June, the North Kivu provincial authorities started supporting with transportation the people displaced by the eruption of the Nyiragongo volcano according to the schedule announced the previous day. The Vice Governor was in Sake to oversee the return of displaced people. On the ground, OCHA teams observed a large movement of returns. Some displaced people, mainly those who lost their homes in the volcanic eruption, remained in Sake, having no accommodation in Goma. Local authorities in Sake have committed to relocating these people to a collective center, and to increasing their protection. According to the North Kivu civil protection, the distribution of government assistance announced by the Prime Minister will take place in the various districts of the city of Goma among the returnees. The Division of Social Affairs (DIVAS), UNICEF, the DRC Red Cross (CRRDC) and the International Committee of the Red Cross (ICRC) continue to work closely together in the identification, assistance, and reunification of unaccompanied children. -

Usaid Solutions for Peace and Recovery Year 4
A WOMEN’S MENTORING AND LEADERSHIP CLUB IN MABANGA WITH THEIR HYGIENE DISTRIBUTION KITS (PHOTO COURTESY OF SPR GRANTEE ACUDI) USAID SOLUTIONS FOR PEACE AND RECOVERY YEAR 4 ANNUAL REPORT, FY 2020 (OCTOBER 2019 – SEPTEMBER 2020) Contract Number AID-OAA-I-13-00042/Task Order Number AID-660-TO-16-00004 30 OCTOBER 30, 2020 This publication was produced for review by the United States Agency for International Development. It was prepared by Management Systems International (MSI), A Tetra Tech Company. USAID SOLUTIONS FOR PEACE AND RECOVERY YEAR 4 ANNUAL REPORT, FY 2020 (October 2019 – September 2020) Contracted under AID-OAA-I-13-00042/Task Order Number AID-660-TO-16-00004 USAID’s Solutions for Peace and Recovery DISCLAIMER The authors’ views expressed in this report do not necessarily reflect the views of the United States Agency for International Development or the United States Government. CONTENTS ACRONYMS AND ABBREVIATIONS ............................................................... III EXECUTIVE SUMMARY ...................................................................................... V SECURITY BACKGROUND AND CONTEXT .................................................. 1 PROJECT SUMMARY ............................................................................................. 2 ACTIVITY IMPLEMENTATION ........................................................................... 3 OBJECTIVE 1: COMMUNITY STAKEHOLDERS IDENTIFY AND ACCEPT SOLUTIONS TO SPECIFIC DRIVERS OF CONFLICT .............................................................................................................. -
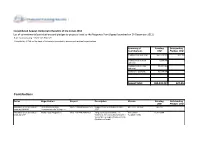
Contributions
Consolidated Appeal: Democratic Republic of the Congo 2012 List of commitments/contributions and pledges to projects listed to the Response Plan (Appeal launched on 14-December-2011) http://fts.unocha.org (Table ref: ReportF) Compiled by OCHA on the basis of information provided by donors and recipient organizations. Summary of Funding Outstanding Contributions USD Pledges USD Contributions sub total: 457,528,823 627,353 Contributions to ERF 1,000,000 0 sub total: Contributions to CHF 89,807,968 0 sub total: Carry-over sub total: 35,094,936 0 Appeal Total: 583,431,727 627,353 Contributions Donor Organization Project Description Cluster Funding Outstanding USD Pledges USD Allocation of unearmarked United Nations High DRC-12/MS/49584/R/120 Support to HCR activities in DRC MULTI CLUSTER 242,737 funds by UNAIDS Commissioner for Refugees 2012 Allocation of unearmarked World Food Programme DRC-12/F/49578/R/561 Targeted Food Assistance To SECURITE 15,310,304 funds by WFP Victims of Armed Conflict and Other ALIMENTAIRE Vulnerable Groups (PRRO 201670) (Multilateral funds) Allocation of unearmarked World Food Programme DRC-12/F/49582/R/561 Emergency Support to the SECURITE 1,349,606 funds by WFP Population Affected by Insecurity in ALIMENTAIRE The Haut and Bas Uele Districts in Orientale Province of DRC (EMOP 200186 and 200362) (Multilateral funds) Allocation of unearmarked World Food Programme DRC-12/F/51715/R/561 Emergency food assistance to newly SECURITE 6,344,551 funds by WFP displaced people in North Kivu and ALIMENTAIRE spillover into South -

ISFD-NORD-KIVU.Pdf
BANQUE CENTRALE DU CONGO Direction de la Surveillance des Intermédiaires Financiers INSTITUTIONS DU SYSTÈME FINANCIER DECENTRALISE DE LA PROVINCE DU NORD KIVU N° DENOMINATION REGION RAYON D'ACTION ADRESSE PHYSIQUE 1 COOPECCO BENI Nord Kivu Beni 135, Avenue du Stade, Quartier Résidentiel, Commune Bugulu ,Ville de Beni 2 COOPECCO-OICHA Nord Kivu Oicha Oicha, Territoire de Beni 3 MECRE-BENI/COOPEC Nord Kivu Beni 92, Boulevard Nyamwisi, Ville de Beni 4 COODEFI/COOPEC Nord Kivu Butembo 14, Avenue Kinshasa , Commune de Mususa, Ville de Butembo 5 COOPEC LA SEMENCE Nord Kivu Butembo 5, Avenue Matokeo, Ville de Butembo 6 155, Avenue Mobutu, Quartier Buturande, Cité de Kiwanja, Territoire de COOPECCO/BUTURANDE Nord Kivu Buturande Rutshuru 7 COOPEC IMARA/GOMA Nord Kivu Goma Boulevard Kanyamuhanga , en face de ONC, Ville de Goma 8 COOPEC ADEC Nord Kivu Goma Avenue des Touristes, Quartier Mikeno, Maison Bercy Ville de Goma 9 COOPEC BONNE MOISSON Nord Kivu GOMA 12, Avenue Karisimbi, Quartier Mikeno, Commune de Goma, Ville de Goma 10 294, Avenue des Alizés , Quartier Murara, Commune Karisimbi, Ville de COOPEC KESHENI Nord Kivu Goma Goma 11 COOPEC TUJENGE PAMOJA Nord Kivu Goma 45, Boulevard Kayambayonga, Ville de Goma 12 COOPEC UMOJA NI NGUVU Nord Kivu GOMA 1, avenue Sake, Quartier Katoyi, Commune de Karisimbi, Ville de Goma 13 MECRE-BIRERE/COOPEC Nord Kivu Goma 11, Avenue du Commerce, Commune Karisimbi, Ville de Goma 14 MECREGO/COOPEC Nord Kivu Goma 30, Boulevard Kanyamuhanga, Quartier de Volcans, Ville de Goma 15 MECRE-KATINDO/COOPEC Nord Kivu Goma -

Download File
UNICEF DRC | Volcano Eruption (Goma) Situation Report Volcano Eruption Goma, DRC Situation Report #3 27 May 2021 Overview The eruption of Mount Nyiragongo on the evening of 22 May 2021, and the two lava flows have affected Kibumba park as well as Buhene and Kibati in the North-East of Goma, DRC. More than 20,000 people from Goma have fled Saké, 25 km north- west of Goma on the day of eruption. 32 people have died as a direct result of the eruption (either burned by the lava or asphyxiated by fumes), including three children, while 40 have been reported missing1. As of 26 May, it is estimated that the eruption directly affected 20 villages within the groupements of Kibati, Munigi and Mutaho, representing 3,629 burned houses2. This results in around more than 20,000 displaced population. (about 4,500 households according to OCHA). Map 1: Nyiragongo Volcano Eruption & Impacted Areas (source: UNICEF) More than 195,000 people, according to the WASH cluster3, might have difficulty in accessing safe water due to a disabled water reservoir and 25,000 persons had already their water access cut off, while access to electricity was cut off in large parts of Goma city. Seven schools (five primary schools4 and two secondary schools) have been affected. 1,957 students and 49 teachers have been affected at primary school level and while 447 students and 72 teachers are affected at secondary school level5. It has also been reported that 38 health centers (including ten in Goma Health Zone, 19 in Karisimbi Health Zone and nine in Nyiragongo Health Zone) have been affected by the volcanic eruption6. -

Democratic Republic of Congo • North Kivu Situation Report No
Democratic Republic of Congo • North Kivu Situation Report No. 4 03 August 2012 This report is produced by OCHA in collaboration with humanitarian partners. It was issued by OCHA DRC. It covers the period from 28 July to 03 August 2012. The next report will be issued on or around 10 August. I. HIGHLIGHTS/KEY PR IORITIES • The CERF allocates US$9.9 million to boost humanitarian response to North Kivu crisis. • Around 30,000 IDPs reported to have fled the Kibati area due to FARDC-M23 fighting. • Priority needs in IDP settlements and camps around Goma include access to health care and potable water. II. Situation Overview Since 26 July no clashes have been reported between the RDC - Nord Kivu Armed Forces of the Democratic Republic of the Congo (FARDC) and the M23 in Rutshuru Territory. On 31 July, Orientale the armed group Patriotic Alliance for a Free and Sovereign Congo (APCLS) launched an attack on the Beni FARDC, taking over the city of Kashuga in Masisi Territory. Civilians fled to Mweso and Kitchanga when the fighting Lubero OUGANDA started. On the first of August, the FARDC retook the city. REPUBLIQUE DEMOCRATIQUE Nord Kivu Pendular population movements have also been reported DU CONGO towards Mweso, Busamba, Mpati, Kitchanga and Kanyabayonga elsewhere as a result of a looting spree by armed groups Rutshuru Karambi of 10 villages located north and south-west of Kitchanga. Walikale Kitchanga Rubare Bunagana On 3 August, an armed group attacked the FARDC in Ntamugenga Masisi Nyiragongo Kasindi in Beni Territory. Maniema Goma RWANDA Concerns have been raised in the north-east of Rutshuru Sud Kivu territory over reports of alliances and increased presence 100 Km of the armed group Democratic Forces for the Liberation Sources: ESRI, Europa Technologies, UNCS, RGC, OCHA et partenaires. -

DR Congo: Volcanic Eruption in Goma Situation Report #14 07 June 2021
DR Congo: Volcanic eruption in Goma Situation Report #14 07 June 2021 This report is produced by OCHA DRC in collaboration with humanitarian partners. It covers the period of 07 June 2021 (4pm Goma time).1 HIGHLIGHTS • The Congolese government announced the gradual return of displaced people to Goma and Nyiragongo territory • Humanitarian actors are ready to support the Government's action plan that is currently being developed Supply of inputs for the management of severe acute malnutrition to the Shasha health center in the Kirotshe health zone. 07 June, Inchi Suhene, Nutrition Cluster. SITUATION OVERVIEW On 07 June, the Prime Minister of the Democratic Republic of Congo (DRC), Jean-Michel Sama Lukonde Kyenge, announced the return of displaced people to the city of Goma and the territory of Nyiragongo. The authorities noted the end of the lava flow and the lava solidification as well as the significant decrease in earthquakes in the area. The Congolese government has declared it will facilitate the gradual return of the displaced population between 08 and 20 June along the different axes: Sake-Goma (08-09 June), Nyiragongo-Goma (10 June), Rutshuru-Goma (11-12 June), Bukavu-Minova-Goma (15-17 June), Beni-Butembo-Lubero-Goma (16-17 June), Rwanda-Goma (19-20 June). The Prime Minister also announced that people who lost their homes in the eruption will be temporarily relocated and will receive Government assistance to rebuild their homes. In addition, Congolese authorities have announced the reopening of schools and universities as of 14 June in the city of Goma and the territory of Nyiragongo, once the buildings have been inspected. -

In Search of Peace: an Autopsy of the Political Dimensions of Violence in the Democratic Republic of Congo
IN SEARCH OF PEACE: AN AUTOPSY OF THE POLITICAL DIMENSIONS OF VIOLENCE IN THE DEMOCRATIC REPUBLIC OF CONGO By AARON ZACHARIAH HALE A DISSERTATION PRESENTED TO THE GRADUATE SCHOOL OF THE UNIVERSITY OF FLORIDA IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF DOCTOR OF PHILOSOPHY UNIVERSITY OF FLORIDA 2009 1 © 2009 Aaron Zachariah Hale 2 To all the Congolese who helped me understand life’s difficult challenges, and to Fredline M’Cormack-Hale for your support and patience during this endeavor 3 ACKNOWLEDGMENTS I was initially skeptical about attending The University of Florida (UF) in 2002 for a number of reasons, but attending UF has been one of the most memorable times of my life. I have been so fortunate to be given the opportunity to study African Politics in the Department of Political Science in a cozy little town like Gainesville. For students interested in Africa, UF’s Center for African Studies (CAS) has been such a fantastic resource and meeting place for all things African. Dr. Leonardo Villalón took over the management of CAS the same year and has led and expanded the CAS to reach beyond its traditional suit of Eastern and Southern African studies to now encompass much of the sub-region of West Africa. The CAS has grown leaps and bounds in recent years with recent faculty hires from many African and European countries to right here in the United States. In addition to a strong and committed body of faculty, I have seen in my stay of seven years the population of graduate and undergraduate students with an interest in Africa only swell, which bodes well for the upcoming generation of new Africanists. -

Social Science in Humanitarian Action
Social Science in Humanitarian Action www.socialscienceinaction.org Social science and behavioural data compilation (#4), Ebola outbreak eastern DRC, June-August 2019 This rapid compilation of data analyses provides a ‘stock-take’ of social science and behavioural data related to the on-going outbreak of Ebola in North Kivu, South Kivu and Ituri provinces. Based on data gathered and analysed by organisations working in the Ebola response and in the region more broadly, it explores convergences and divergences between datasets and, when possible, differences by geographic area, demographic group, time period and other relevant variables. Data sources are listed at the end of the document. This is the fourth data synthesis brief produced by the Social Science in Humanitarian Action Platform (SSHAP) and focuses on data published between June and August 2019. It builds on the previous three data synthesis briefs, the first focusing on data from August- October 2018, the second on data from November 2018 to January 2019, and the third on data from February to May 2019.1 At the time of publication (as of 6 October 2019), 3,205 cases had been reported (3,091 confirmed and 114 probable) of which 2,142 died.2 The overall case fatality ratio was 67%, the same as the rate in the middle of June 2019.3,4. The majority of the 73 confirmed cases identified between 16 September and 6 October were from the health zones of Mambasa (30%; n=22) and Mandima (23%, n=17). This brief was prepared by Kevin Bardosh (University of Washington), Theresa Jones and Juliet Bedford (Anthrologica), with support from SSHAP and GOARN-R Social Science Group. -

U.S. Agency for International Development Bureau of Democracy, Conflict, and Humanitarian Assistance Office of Food for Peace
U.S. Agency for International Development Bureau of Democracy, Conflict, and Humanitarian Assistance Office of Food for Peace Annual Results Report (ARR) Mercy Corps DRC Award Number: FFP-A-11-00008 Submission Date: November 3, 2014 Applicable Fiscal Year: FY 2014 (Include the following information) Awardee HQ Contact Name Rebecca Inman Awardee HQ Contact Address 45 SW Ankeny Street Portland, OR 97204 USA Awardee HQ Contact Telephone Number 1 503 896 5725 Awardee HQ Contact Fax Number 1 503 896 5011 Awardee HQ Contact Email Address [email protected] (Include the following information) Host Country Office Contact Name Mark J. Dwyer Host Country Office Contact Address 02 Avenue Parallele, Quartier Volcans, Goma, North Kivu, DR Congo Host Country Office Contact Telephone + 243 821 645 268 Number Host Country Office Contact Fax Number n/a Host Country Office Contact Email Address [email protected] Annual Results Report SIMAMA Project Cooperative Agreement AID-FFP-A-11-00008-00 LIST OF ACRONYMS ARR Annual Results Report AVA Agent Villageous Agricole (Agriculture Village Agent) AVE Agent Villageous Elevage (Livestock Village Agent) BXW Banana Xanthomonas Wilt BCC Behavior Change Communication CARG Conseil Agricole Rural de Gestion (Rural Agricultural Management Advisory Board) CEDERU Centre du Développement Rural (Rural Development Center) CBO Community Based Organization CDC Community Development Committee CDP Community Development Plan CIG Common interest Groups CMD Cassava Mosaic Disease DFAP Development Food Aid Project DRC Democratic -

Democratic Republic of Congo • North Kivu Situation Report No
Democratic Republic of Congo • North Kivu Situation Report No. 18 17 December 2012 This report is produced by OCHA in collaboration with humanitarian partners. It was issued by OCHADRC. It covers the period from 11 to 18 December 2012. The next report will be issued on or around 20 December. I. HIGHLIGHTS/KEY PRIORITIES Concerns for protection of civilians as armed groups reportedly amass in Masisi Education specialists start rehabilitating 261 schools in Beni territory; 100 schools to receive food for school canteens. Mine experts continue to clean contaminated areas, surveys schools in Goma Girls, 55 percent of children separated from their families II. Situation Overview The situation in Goma and its surroundings continues to remain extremely volatile. The continuing presence of M23 fighters around the town and the reported movements of armed men in Masisi, Nyiragongo and Rutshuru territories concur to maintain a climate of volatility. Concerns for the protection of civilians are being raised in the DRC : North Kivu northeast of Masisi where a strong concentration of armed groups has been observed during the last few days. Sources Mweso indicate that a coalition of armed groups has been formed, and Walikale Rutshuru have hinted of clashes with the Mayi-Mayi Chaka group in Pinga. Kitchanga NORD KIVU Masisi The precarious security situation, which is being exacerbated by Masisi Kirolirwe an increase in burglaries as more 1,000 prisoners escaped from Kingi Kibumba the Goma prison in the wake of M23 taking control of Goma in Mushaki Nyiragongo Sake Kanyaruchinya Kibati mid-November, has forced humanitarian actors to advocate for Mutambiro better security in the areas of displacements notably the camps Bweremana RWANDA Presence of displaced persons Minova Goma around Masisi centre, and around the areas between Kalembe WalikalePriority area approved by CPIA Lac Kivu and Kitchanga and in the Mpati area. -

Ebola Virus Disease Cases by Week of Illness Onset, As of 24 November 2019
EBOLA VIRUS DISEASE Democratic Republic of the Congo External Situation Report 69 Health Emergency Information and Risk Assessment Page 1 WHO Health Emergencies Programme EBOLA VIRUS DISEASE Democratic Republic of the Congo External Situation Report 69 Date of issue: 26 November 2019 Data as reported by: 24 November 2019 Cases DeathsDeaths 1. Situation update 3303 1002199 In the week of 18 to 24 November 2019, seven new confirmed EVD cases were reported from four health zones in two affected provinces in Democratic Republic of the Congo. The majority of the confirmed cases in this week came from Mabalako Health Zone (57%; n=4). Violence and civil unrest in the week have led to the suspension of Ebola response activities in some areas of Beni, Butembo, and Oicha health zones. On 26 November 2019, some response personnel were temporarily relocated from Beni, though most remain in place to continue responding. The immediate focus will be on maintaining the safety and welfare of response personnel while preserving essential response activities in these places. The disruptions to the response and lack of access to Ebola-affected communities is threatening to reverse recent progress. As seen previously during this outbreak, such disruptions limit contact tracing, surveillance, and vaccination efforts, and they often result in increased transmission. In the past 21 days (from 4 to 24 November 2019), 12 health areas and four health zones have reported cases (Table 1, Figure 2). During this period, a total of 28 confirmed cases were reported, with the majority reported from Mabalako (54%; n=15 cases) and Beni (32%; n=9).