Drc 7 2.1 Key Regional Themes 7
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Tangled! Congolese Provincial Elites in a Web of Patronage
Researching livelihoods and services affected by conflict Tangled! Congolese provincial elites in a web of patronage Working paper 64 Lisa Jené and Pierre Englebert January 2019 Written by Lisa Jené and Pierre Englebert SLRC publications present information, analysis and key policy recommendations on issues relating to livelihoods, basic services and social protection in conflict-affected situations. This and other SLRC publications are available from www.securelivelihoods.org. Funded by UK aid from the UK Government, Irish Aid and the EC. Disclaimer: The views presented in this publication are those of the author(s) and do not necessarily reflect the UK Government’s official policies or represent the views of Irish Aid, the EC, SLRC or our partners. ©SLRC 2018. Readers are encouraged to quote or reproduce material from SLRC for their own publications. As copyright holder SLRC requests due acknowledgement. Secure Livelihoods Research Consortium Overseas Development Institute (ODI) 203 Blackfriars Road London SE1 8NJ United Kingdom T +44 (0)20 3817 0031 F +44 (0)20 7922 0399 E [email protected] www.securelivelihoods.org @SLRCtweet Cover photo: Provincial Assembly, Lualaba. Lisa Jené, 2018 (CC BY-NC-ND 2.0). B About us The Secure Livelihoods Research Consortium (SLRC) is a global research programme exploring basic services, livelihoods and social protection in fragile and conflict-affected situations. Funded by UK Aid from the UK Government’s Department for International Development (DFID), with complementary funding from Irish Aid and the European Commission (EC), SLRC was established in 2011 with the aim of strengthening the evidence base and informing policy and practice around livelihoods and services in conflict. -

IMCK Newsletter 17.3.Pages
INSTITUT MEDICAL CHRETIEN DU KASAI !1 OFINSTITUT MEDICAL!5 CHRETIEN DU KASAI B.P. 205 KANANGA B.P. 205 KANANGA INSTITUT MEDICAL CHRETIENREPUBLIQUE DEMOCRATIQUE DU DUKASAI CONGO REPUBLIQUE DEMOCRATIQUE DU CONGO Christian Medical Institute Hôpitalof – theEcole d’infirmiers Kasai – Ecole de laborantins - Serving – Service de santé communautairein Central - Service d’ophtalmologie Congo Service dentaire – Centre d’études et de recyclage Hôpital – Ecole d’infirmiers – Ecole de laborantins – Service de santé communautaire - Service d’ophtalmologie E-mail : [email protected] Service dentaire – Centre d’études et de recyclage B. P. 205 Kananga, Republic Democratic du Congo ; Email: [email protected] E-mail : [email protected] 2. Find a way to channel a greater percentage of donations back into that unpopular category 2. Find a way to channel a greater percentage of donations back into that unpopular category of “undesignated” gifts so that we can have the flexibility to apply them where A Periodic Newsletter operational needs are Issuethe most desperate. No. 41 But ifJanuary you cannot (and - thatMarch is understandable, 2017 of “undesignated” gifts so that we can have the flexibility to apply them whereA considering all the news stories one sees about mismanaged funds), then consider operational needs are the most desperate. But if you cannot (and that is understandable, designating gifts carefully to those things that are at the core of IMCK’s operational considering all the news stories one sees about mismanaged funds), then consider The current conflict in the Kasai has needs.I askedFor example the new: Specify IMCK money Administrator, for medicines and Kastin medical Katawa, supplies; Specifyto describe money designating gifts carefully to those things that are at the core of IMCK’s operational added new suffering and danger. -

Introduction Generale
P a g e | 1 INTRODUCTION GENERALE 0.1. Problématique Le présent mémoire porte sur les logotypes et la signification : Analyse de la dénotation et de la connotation des logotypes des banques Trust Merchant Bank (TMB) et Rawbank. En effet, Sperber1 dit qu’il n’y a rien de plus banal que la communication, car les êtres humains sont par nature des êtres communiquant par la parole, le geste, l’écrit, l’habillement et voire le silence, etc. La célèbre école de Palo Alto le dit tout haut aussi: on ne peut pas ne pas communiquer, tout est communication2. La communication, nous la pratiquons tous les jours sans y penser (mais également en y pensant) et généralement avec un succès assez impressionnant, même si parfois nous sommes confrontés à ses limites et à ses échecs. La communication demeure l’élément fondamental et complexe de la vie sociale qui rend possible l’interaction des personnes et dont la caractéristique essentielle est, selon Daniel Lagache3, la réciprocité. Elle est ce par quoi une personne influence une autre et en est influencée, car elle n’est pas indépendante des effets de son action. Morin affirme même que la communication a plusieurs fonctions : l’information, la connaissance, l’explication et la compréhension. Toutefois, pour lui, le problème central dans la communication humaine est celui de la compréhension, car on communique pour comprendre et se comprendre4. Raison pour laquelle, les chercheurs en matière de communication, surtout de notre ère, époque marquée par l’accroissement des entreprises dans la plupart des secteurs de la vie sociale, se trouvent confronté à de nouvelles problématiques qui sont autant d’enjeux pour améliorer la communication. -
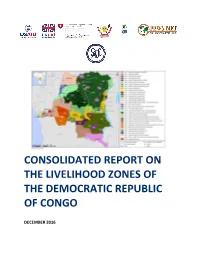
DRC Consolidated Zoning Report
CONSOLIDATED REPORT ON THE LIVELIHOOD ZONES OF THE DEMOCRATIC REPUBLIC OF CONGO DECEMBER 2016 Contents ACRONYMS AND ABBREVIATIONS ......................................................................................... 5 ACKNOWLEDGEMENTS .......................................................................................................... 6 1. INTRODUCTION ................................................................................................................ 7 1.1 Livelihoods zoning ....................................................................................................................7 1.2 Implementation of the livelihood zoning ...................................................................................8 2. RURAL LIVELIHOODS IN DRC - AN OVERVIEW .................................................................. 11 2.1 The geographical context ........................................................................................................ 11 2.2 The shared context of the livelihood zones ............................................................................. 14 2.3 Food security questions ......................................................................................................... 16 3. SUMMARY DESCRIPTIONS OF THE LIVELIHOOD ZONES .................................................... 18 CD01 COPPERBELT AND MARGINAL AGRICULTURE ....................................................................... 18 CD01: Seasonal calendar .................................................................................................................... -

The DRC Seed Sector
A Quarter-Billion Dollar Industry? The DRC Seed Sector BRIEF DESCRIPTION: Compelling investment opportunities exist for seed companies and seed start-ups in the Democratic Republic of the Congo (DRC). This document outlines the market potential and consumer demand trends in the DRC and highlights the high potential of seed production in the country. 1 Executive Summary Compelling investment opportunities exist for seed companies and seed start-ups in the Democratic Republic of the Congo (DRC). This document outlines the market potential and consumer demand trends in the DRC and highlights the high potential of seed production in the country. The DRC is the second largest country in Africa with over 80 million hectares of agricultural land, of which 4 to 7 million hectares are irrigable. Average rainfall varies between 800 mm and 1,800 mm per annum. Bimodal and extended unimodal rainfall patterns allow for two agricultural seasons in approximately 75% of the country. Average relative humidity ranges from 45% to 90% depending on the time of year and location. The market potential for maize, rice and bean seed in the DRC is estimated at $191 million per annum, of which a mere 3% has been exploited. Maize seed sells at $3.1 per kilogramme of hybrid seed and $1.6 per kilogramme of OPV seed, a higher price than in Tanzania, Kenya, Uganda and Zambia. Seed-to-grain ratios are comparable with regional benchmarks at 5.5:1 for hybrid maize seed and 5.0:1 for OPV maize seed. The DRC is defined by four relatively distinct sales zones, which broadly coincide with the country’s four principal climate zones. -

DR Congo: Volcanic Eruption in Goma Situation Report #15 08 June 2021
DR Congo: Volcanic eruption in Goma Situation Report #15 08 June 2021 This report is produced by OCHA DRC in collaboration with humanitarian partners. It covers the period of June 08, 2021 (4pm Goma time).1 As of 09 June, the Situation Report will be issued on weekly basis, and in French. The next Situation Report will be published on Monday, 14 June 2021. HIGHLIGHTS • Return of displaced people from Sake towards Goma begins • Process of identification by the authorities of temporary relocation area Displaced people in Sake board a transport provided by the government to facilitate their return to Goma. 08 June, OCHA/Nadege Nodji SITUATION OVERVIEW On 08 June, the North Kivu provincial authorities started supporting with transportation the people displaced by the eruption of the Nyiragongo volcano according to the schedule announced the previous day. The Vice Governor was in Sake to oversee the return of displaced people. On the ground, OCHA teams observed a large movement of returns. Some displaced people, mainly those who lost their homes in the volcanic eruption, remained in Sake, having no accommodation in Goma. Local authorities in Sake have committed to relocating these people to a collective center, and to increasing their protection. According to the North Kivu civil protection, the distribution of government assistance announced by the Prime Minister will take place in the various districts of the city of Goma among the returnees. The Division of Social Affairs (DIVAS), UNICEF, the DRC Red Cross (CRRDC) and the International Committee of the Red Cross (ICRC) continue to work closely together in the identification, assistance, and reunification of unaccompanied children. -

La Ville De Kinshasa
« Kin la belle… – et Kin la poubelle» La ville de Kinshasa Suite à la dégradation économique et plu- En 1881, Henry sieurs vagues de pilla- Morton Stanley ges, les anciens quar- fonde le poste tiers de l’élite (la Léopoldville, Gombe, Ma Campa- nommé après gne à Ngaliema et par le Roi des quelques parties de Belges, colonisa- Limete) sont aujourd’hui d’un charme plutôt morbide. teur du Congo. L’endroit est spacieux et facile à défen- La réhabilitation des routes demeure un défi majeur. dre, ils existent plusieurs villages autochtones sur le Le personnel de la mission EUPOL RD Congo à Kinshasa, Dans les cités, des tornades de pluie font écouler des site. Léopoldville devient centre administratif du octobre 2008. maisons pendant chaque saison de pluie. Congo-Belge en 1929 (avant, c’était la ville de Boma « Kinshasa – the beauty and the beast »: Due to the de- sur la côte atlantique). La capitale devient Kinshasa en gradation of the economic situation and several lootings, 1966. / I n 1881, Henry Morton Stanley founds Leopold- EUPOL RDC et EUSEC RDC, ville, a settlement named after the Belgian King, owner the ancient elite’s quarters of Gombe, Ma Campagne in les deux missions PESD Ngaliema and some parts of Limete show nowadays a of the colony. The site is vast and easy to defend; there rather morbid charme. Rehabilitating Kinshasa’s roads en République Démocratique du Congo, are already several villages of natives in the area. Leo- rests a major challenge for the city’s development. In the vous souhaitent un bon séjour poldville is named administrative center of the Belgian- popular quarters, violent rain downpours bring down à Kinshasa. -

Democratic Republic of the Congo of the Congo Democratic Republic
Democratic Republic of the Congo of the Congo Democratic Republic Main objectives Impact • UNHCR provided international protection to some In 2005, UNHCR aimed to strengthen the protection 204,300 refugees in the DRC of whom some 15,200 framework through national capacity building, registra- received humanitarian assistance. tion, and the prevention of and response to sexual and • Some of the 22,400 refugees hosted by the DRC gender-based violence; facilitate the voluntary repatria- were repatriated to their home countries (Angola, tion of Angolan, Burundian, Rwandan, Ugandan and Rwanda and Burundi). Sudanese refugees; provide basic assistance to and • Some 38,900 DRC Congolese refugees returned to locally integrate refugee groups that opt to remain in the the DRC, including 14,500 under UNHCR auspices. Democratic Republic of the Congo (DRC); prepare and UNHCR monitored the situation of at least 32,000 of organize the return and reintegration of DRC Congolese these returnees. refugees into their areas of origin; and support initiatives • With the help of the local authorities, UNHCR con- for demobilization, disarmament, repatriation, reintegra- ducted verification exercises in several refugee tion and resettlement (DDRRR) and the Multi-Country locations, which allowed UNHCR to revise its esti- Demobilization and Reintegration Programme (MDRP) mates of the beneficiary population. in cooperation with the UN peacekeeping mission, • UNHCR continued to assist the National Commission UNDP and the World Bank. for Refugees (CNR) in maintaining its advocacy role, urging local authorities to respect refugee rights. UNHCR Global Report 2005 123 Working environment Recurrent security threats in some regions have put another strain on this situation. -

Usaid Solutions for Peace and Recovery Year 4
A WOMEN’S MENTORING AND LEADERSHIP CLUB IN MABANGA WITH THEIR HYGIENE DISTRIBUTION KITS (PHOTO COURTESY OF SPR GRANTEE ACUDI) USAID SOLUTIONS FOR PEACE AND RECOVERY YEAR 4 ANNUAL REPORT, FY 2020 (OCTOBER 2019 – SEPTEMBER 2020) Contract Number AID-OAA-I-13-00042/Task Order Number AID-660-TO-16-00004 30 OCTOBER 30, 2020 This publication was produced for review by the United States Agency for International Development. It was prepared by Management Systems International (MSI), A Tetra Tech Company. USAID SOLUTIONS FOR PEACE AND RECOVERY YEAR 4 ANNUAL REPORT, FY 2020 (October 2019 – September 2020) Contracted under AID-OAA-I-13-00042/Task Order Number AID-660-TO-16-00004 USAID’s Solutions for Peace and Recovery DISCLAIMER The authors’ views expressed in this report do not necessarily reflect the views of the United States Agency for International Development or the United States Government. CONTENTS ACRONYMS AND ABBREVIATIONS ............................................................... III EXECUTIVE SUMMARY ...................................................................................... V SECURITY BACKGROUND AND CONTEXT .................................................. 1 PROJECT SUMMARY ............................................................................................. 2 ACTIVITY IMPLEMENTATION ........................................................................... 3 OBJECTIVE 1: COMMUNITY STAKEHOLDERS IDENTIFY AND ACCEPT SOLUTIONS TO SPECIFIC DRIVERS OF CONFLICT .............................................................................................................. -

Cycles Approved by OHRM for S
Consolidated list of duty stations approved by OHRM for rest and recuperation (R & R) (as of 1 July 2015) Duty Station Frequency R & R Destination AFGHANISTAN Entire country 6 weeks Dubai ALGERIA Tindouf 8 weeks Las Palmas BURKINA FASO Dori 12 weeks Ouagadougou BURUNDI Bujumbura, Gitega, Makamba, Ngozi 8 weeks Nairobi CENTRAL AFRICAN REPUBLIC Entire country 6 weeks Yaoundé CHAD Abeche, Farchana, Goré, Gozbeida, Mao, N’Djamena, Sarh 8 weeks Addis Ababa COLOMBIA Quibdo 12 weeks Bogota COTE D’IVOIRE Entire country except Abidjan and Yamoussoukro 8 weeks Accra DEMOCRATIC REPUBLIC OF THE CONGO Aru, Beni, Bukavu, Bunia, Butembo, Dungu, Goma, Kalemie, Mahagi, Uvira 6 weeks Entebbe Bili, Bandundu, Gemena, Kamina, Kananga, Kindu, Kisangani, Matadi, Mbandaka, Mbuji-Mayi 8 weeks Entebbe Lubumbashi 12 weeks Entebbe DEMOCRATIC PEOPLE’S REPUBLIC OF KOREA Pyongyang 8 weeks Beijing ETHIOPIA Kebridehar 6 weeks Addis Ababa Jijiga 8 weeks Addis Ababa GAZA Gaza (entire) 8 weeks Amman GUINEA Entire country 6 weeks Accra HAITI Entire country 8 weeks Santo Domingo INDONESIA Jayapura 12 weeks Jakarta IRAQ Baghdad, Basrah, Kirkuk, Dohuk 4 weeks Amman Erbil, Sulaymaniah 8 weeks Amman KENYA Dadaab, Wajir, Liboi 6 weeks Nairobi Kakuma 8 weeks Nairobi KYRGYZSTAN Osh 8 weeks Istanbul LIBERIA Entire country 8 weeks Accra LIBYA Entire country 6 weeks Malta MALI Gao, Kidal, Tesalit 4 weeks Dakar Tombouctou, Mopti 6 weeks Dakar Bamako, Kayes 8 weeks Dakar MYANMAR Sittwe 8 weeks Yangon Myitkyina (Kachin State) 12 weeks Yangon NEPAL Bharatpur, Bidur, Charikot, Dhunche, -

Mecanisme De Referencement
EN CAS DE VIOLENCE SEXUELLE, VOUS POUVEZ VOUS ORIENTEZ AUX SERVICES CONFIDENTIELLES SUIVANTES : RACONTER A QUELQU’UN CE QUI EST ARRIVE ET DEMANDER DE L’AIDE La/e survivant(e) raconte ce qui lui est arrivé à sa famille, à un ami ou à un membre de la communauté; cette personne accompagne la/e survivant(e) au La/e survivant(e) rapporte elle-même ce qui lui est arrivé à un prestataire de services « point d’entrée » psychosocial ou de santé OPTION 1 : Appeler la ligne d’urgence 122 OPTION 2 : Orientez-vous vers les acteurs suivants REPONSE IMMEDIATE Le prestataire de services doit fournir un environnement sûr et bienveillant à la/e survivant(e) et respecter ses souhaits ainsi que le principe de confidentialité ; demander quels sont ses besoins immédiats ; lui prodiguer des informations claires et honnêtes sur les services disponibles. Si la/e survivant(e) est d'accord et le demande, se procurer son consentement éclairé et procéder aux référencements ; l’accompagner pour l’aider à avoir accès aux services. Point d’entrée médicale/de santé Hôpitaux/Structures permanentes : Province du Haut Katanga ZS Lubumbashi Point d’entrée pour le soutien psychosocial CS KIMBEIMBE, Camps militaire de KIMBEIMBE, route Likasi, Tel : 0810405630 Ville de Lubumbashi ZS KAMPEMBA Division provinciale du Genre, avenue des chutes en face de la Division de Transport, HGR Abricotiers, avenue des Abricotiers coin avenue des plaines, Q/ Bel Air, Bureau 5, Centre ville de Lubumbashi. Tel : 081 7369487, +243811697227 Tel : 0842062911 AFEMDECO, avenue des pommiers, Q/Bel Air, C/KAMPEMBA, Tel : 081 0405630 ZS RUASHI EASD : n°55, Rue 2, C/ KATUBA, Ville de Lubumbashi. -

An Inventory of Fish Species at the Urban Markets of Lubumbashi, Democratic Republic of Congo
FISHERIES AND HIV/AIDS IN AFRICA: INVESTING IN SUSTAINABLE SOLUTIONS PROJECT REPORT | 1983 An inventory of fi sh species at the urban markets of Lubumbashi, Democratic Republic of Congo. Mujinga, W. • Lwamba, J. • Mutala, S. • Hüsken, S.M.C. • Reducing poverty and hunger by improving fisheries and aquaculture www.worldfi shcenter.org An inventory of fish species at the urban markets of Lubumbashi, Democratic Republic of Congo. Mujinga, W., Lwamba, J., Mutala, S. et Hüsken, S.M.C. Translation by Prof. A. Ngosa November 2009 Fisheries and HIV/AIDS in Africa: Investing in Sustainable Solutions This report was produced under the Regional Programme “Fisheries and HIV/AIDS in Africa: Investing in Sustainable Solutions” by the WorldFish Center and the Food and Agriculture Organization of the United Nations (FAO), with financial assistance from the Swedish International Development Cooperation Agency (Sida) and the Norwegian Ministry of Foreign Affairs. This publication should be cited as: Mujinga, W., Lwamba, J., Mutala, S. and Hüsken, S.M.C. (2009). An inventory of fish species at the urban markets in Lubumbashi, Democratic Republic of Congo. Regional Programme Fisheries and HIV/AIDS in Africa: Investing in Sustainable Solutions. The WorldFish Center. Project Report 1983. Authors’ affiliations: W. Mujinga : University of Lubumbashi, Clinique Universitaire. J. Lwamba : University of Lubumbashi, Clinique Universitaire. S. Mutala: The WorldFish Center DRC S.M.C. Hüsken: The WorldFish Center Zambia National Library of Malaysia Cataloguing-in-Publication Data Cover design: Vizual Solution © 2010 The WorldFish Center All rights reserved. This publication may be reproduced in whole or in part for educational or non-profit purposes without permission of, but with acknowledgment to the author(s) and The WorldFish Center.