Social Science in Humanitarian Action
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

DR Congo: Volcanic Eruption in Goma Situation Report #15 08 June 2021
DR Congo: Volcanic eruption in Goma Situation Report #15 08 June 2021 This report is produced by OCHA DRC in collaboration with humanitarian partners. It covers the period of June 08, 2021 (4pm Goma time).1 As of 09 June, the Situation Report will be issued on weekly basis, and in French. The next Situation Report will be published on Monday, 14 June 2021. HIGHLIGHTS • Return of displaced people from Sake towards Goma begins • Process of identification by the authorities of temporary relocation area Displaced people in Sake board a transport provided by the government to facilitate their return to Goma. 08 June, OCHA/Nadege Nodji SITUATION OVERVIEW On 08 June, the North Kivu provincial authorities started supporting with transportation the people displaced by the eruption of the Nyiragongo volcano according to the schedule announced the previous day. The Vice Governor was in Sake to oversee the return of displaced people. On the ground, OCHA teams observed a large movement of returns. Some displaced people, mainly those who lost their homes in the volcanic eruption, remained in Sake, having no accommodation in Goma. Local authorities in Sake have committed to relocating these people to a collective center, and to increasing their protection. According to the North Kivu civil protection, the distribution of government assistance announced by the Prime Minister will take place in the various districts of the city of Goma among the returnees. The Division of Social Affairs (DIVAS), UNICEF, the DRC Red Cross (CRRDC) and the International Committee of the Red Cross (ICRC) continue to work closely together in the identification, assistance, and reunification of unaccompanied children. -

Democratic Republic of Congo
DEMOCRATIC REPUBLIC OF CONGO 350 Fifth Ave 34 th Floor New York, N.Y. 10118-3299 http://www.hrw.org (212) 290-4700 Vol. 14, No. 6 (G) – August 2002 I counted thirty bodies and bags between the dam and the small rapids, and twelve beyond the rapids. Most corpses were in underwear, and many were beheaded. On the bridges there were still many traces of blood despite attempts to cover them with sand, and on the small maize field to the left of the landing the odors were unbearable. Human Rights Watch interview, Kisangani, June 2002. A Congolese man from Kisangani covers his mouth as he nears the Tshopo bridge, the scene of summary executions by RCD-Goma troops following an attempted mutiny. (c) 2002 AFP WAR CRIMES IN KISANGANI: The Response of Rwandan-backed Rebels to the May 2002 Mutiny 1630 Connecticut Ave, N.W., Suite 500 2nd Floor, 2-12 Pentonville Road 15 Rue Van Campenhout Washington, DC 20009 London N1 9HF, UK 1000 Brussels, Belgium TEL (202) 612-4321 TEL: (44 20) 7713 1995 TEL (32 2) 732-2009 FAX (202) 612-4333 FAX: (44 20) 7713 1800 FAX (32 2) 732-0471 E-mail: [email protected] E-mail: [email protected] E-mail: [email protected] August 2002 Vol. 14, No 6 (A) DEMOCRATIC REPUBLIC OF CONGO WAR CRIMES IN KISANGANI: The Response of Rwandan-backed Rebels to the May 2002 Mutiny I. SUMMARY...........................................................................................................................................................2 II. RECOMMENDATIONS......................................................................................................................................3 -

Report on Violations of Human Rights and International Humanitarian Law by the Allied Democratic Forces Armed
UNITED NATIONS JOINT HUMAN RIGHTS OFFICE OHCHR-MONUSCO Report on violations of human rights and international humanitarian law by the Allied Democratic Forces armed group and by members of the defense and security forces in Beni territory, North Kivu province and Irumu and Mambasa territories, Ituri province, between 1 January 2019 and 31 January 2020 July 2020 Table of contents Summary ......................................................................................................................................................................... 4 I. Methodology and challenges encountered ............................................................................................ 7 II. Overview of the armed group Allied Democratic Forces (ADF) ................................................. 8 III. Context of the attacks in Beni territory ................................................................................................. 8 A. Evolution of the attacks from January 2015 to December 2018 .................................................. 8 B. Context of the attacks from 1 January 2019 and 31 January 2020 ............................................ 9 IV. Modus operandi............................................................................................................................................. 11 V. Human rights violations and abuses and violations of international humanitarian law . 11 A. By ADF combattants .................................................................................................................................. -

The Tragedy of Goma Most Spectacular Manifestation of This Process Is Africa’S Lori Dengler/For the Times-Standard Great Rift Valley
concentrate heat flowing from deeper parts of the earth like a thicK BlanKet. The heat eventually causes the plate to bulge and stretch. As the plate thins, fissures form allowing vents for hydrothermal and volcanic activity. The Not My Fault: The tragedy of Goma most spectacular manifestation of this process is Africa’s Lori Dengler/For the Times-Standard Great Rift Valley. Posted June 6, 2021 https://www.times-standard.com/2021/06/06/lori- In Africa, we are witnessing the Birth of a new plate dengler-the-tragedy-of-goma/ boundary. Extensional stresses from the thinning crust aren’t uniform. The result is a number of fissures and tears On May 22nd Mount Nyiragongo in the Democratic oriented roughly north south. The rifting began in the Afar RepuBlic of the Congo (DRC) erupted. Lava flowed towards region of northern Ethiopia around 30 million years ago the city of Goma, nine miles to the south. Goma, a city of and has slowly propagated to the south at a rate of a few 670,000 people, is located on the north shore of Lake Kivu inches per year and has now reached MozamBique. In the and adjacent to the Rwanda border. Not all of the details coming millennia, the rifts will continue to grow, eventually are completely clear, but the current damage tally is 32 splitting Ethiopia, Kenya, Tanzania and much of deaths, 1000 homes destroyed, and nearly 500,000 people Mozambique into a new small continent, much liKe how displaced. Madagascar Began to Be detached from the main African continent roughly 160 million years ago. -

Usaid Solutions for Peace and Recovery Year 4
A WOMEN’S MENTORING AND LEADERSHIP CLUB IN MABANGA WITH THEIR HYGIENE DISTRIBUTION KITS (PHOTO COURTESY OF SPR GRANTEE ACUDI) USAID SOLUTIONS FOR PEACE AND RECOVERY YEAR 4 ANNUAL REPORT, FY 2020 (OCTOBER 2019 – SEPTEMBER 2020) Contract Number AID-OAA-I-13-00042/Task Order Number AID-660-TO-16-00004 30 OCTOBER 30, 2020 This publication was produced for review by the United States Agency for International Development. It was prepared by Management Systems International (MSI), A Tetra Tech Company. USAID SOLUTIONS FOR PEACE AND RECOVERY YEAR 4 ANNUAL REPORT, FY 2020 (October 2019 – September 2020) Contracted under AID-OAA-I-13-00042/Task Order Number AID-660-TO-16-00004 USAID’s Solutions for Peace and Recovery DISCLAIMER The authors’ views expressed in this report do not necessarily reflect the views of the United States Agency for International Development or the United States Government. CONTENTS ACRONYMS AND ABBREVIATIONS ............................................................... III EXECUTIVE SUMMARY ...................................................................................... V SECURITY BACKGROUND AND CONTEXT .................................................. 1 PROJECT SUMMARY ............................................................................................. 2 ACTIVITY IMPLEMENTATION ........................................................................... 3 OBJECTIVE 1: COMMUNITY STAKEHOLDERS IDENTIFY AND ACCEPT SOLUTIONS TO SPECIFIC DRIVERS OF CONFLICT .............................................................................................................. -

Volcano Eruption Goma, DRC Situation Report #4 1St June2021
UNICEF DRC | Volcano Eruption (Goma) Situation Report Volcano Eruption Goma, DRC Situation Report #4 1st June2021 Situation Overview The sudden eruption of Mount Nyiragongo on the evening of 22 May 2021, led to two lava flows towards Kibumba park as well as Buhene and Kibati in the North-East of Goma, DRC. 32 people died as a direct result of the eruption (either burned by the lava or asphyxiated by fumes), including three children, while 40 have been reported missing1. As of 26 May, it is estimated that the eruption directly affected 20 villages within the groupements of Kibati, Munigi and Mutaho, with an estimated 3,629 burned houses 2 . According to the WASH cluster 3 , over 195,000 people might have Map 1: Location of the evacuated and host areas (source: UNICEF) difficulty in accessing safe water due to a disabled water reservoir directly damaged by the lava. while access to electricity was cut off in large parts of Goma city. Seven schools (five primary schools4 and two secondary schools) and 37 health centers 5 have been affected by the volcanic eruption. During the night of 27 May, the government decided to evacuate ten neighbourhoods of Goma city (Majengo, Mabanga Nord, Mabanga Sud, Bujovu, Virunga, Murara, Mapendo, Mikeno, Kayembe, Le Volcan) towards Sake, thus leading to important population movements and increased humanitarian needs, before asking the population to go to the town of Rutshuru instead on May 28. As of June 1st, according OCHA6, this evacuation has led to the displacement of around 234,000 people in DRC, with around 63,000 people displaced to Sake, around 67,000 to Minova, around 53,000 to Rutshuru, 11,000 to Lubero, 40,000 to Bukavu. -
Walikale Nicholas Garrett Artisanal Cassiterite Mining and Trade in North Kivu June 1, 2008 Implications for Poverty Reduction and Security
Walikale Nicholas Garrett Artisanal Cassiterite Mining and Trade in North Kivu June 1, 2008 Implications for Poverty Reduction and Security 1 ACKNOWLEDGEMENTS This report was prepared by Nicholas Garrett for the Communities and Artisanal & Small-scale Mining initiative (CASM). Nicholas Garrett is a Mining Consultant from the UK Resource Consulting Services Ltd (RSS), and specialising in conflict and post-conflict minerals management and corporate social responsibility in high-risk environments. The contribution of Estelle A. Levin and Harrison Mitchell (RSS) and of those who have reviewed the final report is acknowledged, as well as to everyone who provided support to the author to conduct extensive research on the ground in the DR Congo. Front cover photo: Artisanal cassiterite mining in Bisie, North Kivu/DRC © Nicholas Garrett Disclaimer: The views expressed in this report are those of the author and do not necessarily reflect those of CASM or other organizations. 2 CONTENTS List of Acronyms 5 Sections Preface and Methodology 6 Synopsis 7 Background and Context 12 Legal Framework 18 Governance 23 Geography, Physical Access, Infrastructure and Transport 32 Structure of Production 37 Economics of Production 41 Economics of Trade 43 Payments to Authorities 56 Demography and Poverty 63 External Stakeholders and Development Assistance 62 Conclusion and Recommendations 76 Bibliography 87 Fact Boxes Box 1: What is Cassiterite? 13 Box 2: Key Features of Artisanal Mining (AM) in North Kivu 16 Box 3: SAESSCAM 22 Box 4: Workers’ Income in Bisie -
Contributions
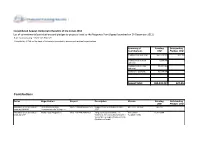
Consolidated Appeal: Democratic Republic of the Congo 2012 List of commitments/contributions and pledges to projects listed to the Response Plan (Appeal launched on 14-December-2011) http://fts.unocha.org (Table ref: ReportF) Compiled by OCHA on the basis of information provided by donors and recipient organizations. Summary of Funding Outstanding Contributions USD Pledges USD Contributions sub total: 457,528,823 627,353 Contributions to ERF 1,000,000 0 sub total: Contributions to CHF 89,807,968 0 sub total: Carry-over sub total: 35,094,936 0 Appeal Total: 583,431,727 627,353 Contributions Donor Organization Project Description Cluster Funding Outstanding USD Pledges USD Allocation of unearmarked United Nations High DRC-12/MS/49584/R/120 Support to HCR activities in DRC MULTI CLUSTER 242,737 funds by UNAIDS Commissioner for Refugees 2012 Allocation of unearmarked World Food Programme DRC-12/F/49578/R/561 Targeted Food Assistance To SECURITE 15,310,304 funds by WFP Victims of Armed Conflict and Other ALIMENTAIRE Vulnerable Groups (PRRO 201670) (Multilateral funds) Allocation of unearmarked World Food Programme DRC-12/F/49582/R/561 Emergency Support to the SECURITE 1,349,606 funds by WFP Population Affected by Insecurity in ALIMENTAIRE The Haut and Bas Uele Districts in Orientale Province of DRC (EMOP 200186 and 200362) (Multilateral funds) Allocation of unearmarked World Food Programme DRC-12/F/51715/R/561 Emergency food assistance to newly SECURITE 6,344,551 funds by WFP displaced people in North Kivu and ALIMENTAIRE spillover into South -

OCHA DRC Kinshasa Goma Kisangani Kisangani Bukavu Bunia
OCHA DRC Kinshasa Goma Kisangani Bukavu Bunia Mbandaka CONTEXT More than ever before since the onset of the war, the reporting period provided ample and eloquent arguments to perceive the humanitarian crisis in the DRC as a unique drama caused in the first place by unbridled violence, defiant impunity and ongoing violation of fundamental humanitarian principles. What comes first is the cold-blooded settlement of scores between two foreign troops in DRC’s third largest town, using heavy armament and ignoring humanitarian cease-fires in a total disregard for the fate of 600,000 civilians. Such exceptional circumstances led to the non less remarkable adoption of the UNSC Resolution 1304, marked by references to Chapter VII of the UN Charter, and by the presence of Ugandan and Rwandan Foreign ministers. Parallel to blatant violations of humanitarian principles, the level of daily mortality as a direct effect of the ongoing war in eastern DRC, as surveyed recently by International Rescue Committee, gives a horrific account of the silent disaster experienced by Congolese civilians in eastern provinces. Daily violence, mutual fears combined with shrinking access to most basic health services, are breeding an environment of vulnerability that led civilians of Kivu to portray themselves as the “wrecked of the earth”. In a poorly inhabited and remote province such as Maniema, an FAO mission estimated at 68% of the population the proportion of those who had to flee from home at one point since August 1998 (110,000 are still hiding in the forest). A third, most ordinary facet of DRC’s humanitarian crisis, is that witnessed by a humanitarian team in a village on the frontline in northern Katanga, where the absence of food and non food trade across the frontline (with the exception of discreet exchanges between troops) brings both displaced and host communities on the verge of starvation. -
Kitona Operations: Rwanda's Gamble to Capture Kinshasa and The
Courtesy of Author Courtesy of Author of Courtesy Rwandan Patriotic Army soldiers during 1998 Congo war and insurgency Rwandan Patriotic Army soldiers guard refugees streaming toward collection point near Rwerere during Rwanda insurgency, 1998 The Kitona Operation RWANDA’S GAMBLE TO CAPTURE KINSHASA AND THE MIsrEADING OF An “ALLY” By JAMES STEJSKAL One who is not acquainted with the designs of his neighbors should not enter into alliances with them. —SUN TZU James Stejskal is a Consultant on International Political and Security Affairs and a Military Historian. He was present at the U.S. Embassy in Kigali, Rwanda, from 1997 to 2000, and witnessed the events of the Second Congo War. He is a retired Foreign Service Officer (Political Officer) and retired from the U.S. Army as a Special Forces Warrant Officer in 1996. He is currently working as a Consulting Historian for the Namib Battlefield Heritage Project. ndupress.ndu.edu issue 68, 1 st quarter 2013 / JFQ 99 RECALL | The Kitona Operation n early August 1998, a white Boeing remain hurdles that must be confronted by Uganda, DRC in 1998 remained a safe haven 727 commercial airliner touched down U.S. planners and decisionmakers when for rebels who represented a threat to their unannounced and without warning considering military operations in today’s respective nations. Angola had shared this at the Kitona military airbase in Africa. Rwanda’s foray into DRC in 1998 also concern in 1996, and its dominant security I illustrates the consequences of a failure to imperative remained an ongoing civil war the southwestern Bas Congo region of the Democratic Republic of the Congo (DRC). -

ISFD-NORD-KIVU.Pdf
BANQUE CENTRALE DU CONGO Direction de la Surveillance des Intermédiaires Financiers INSTITUTIONS DU SYSTÈME FINANCIER DECENTRALISE DE LA PROVINCE DU NORD KIVU N° DENOMINATION REGION RAYON D'ACTION ADRESSE PHYSIQUE 1 COOPECCO BENI Nord Kivu Beni 135, Avenue du Stade, Quartier Résidentiel, Commune Bugulu ,Ville de Beni 2 COOPECCO-OICHA Nord Kivu Oicha Oicha, Territoire de Beni 3 MECRE-BENI/COOPEC Nord Kivu Beni 92, Boulevard Nyamwisi, Ville de Beni 4 COODEFI/COOPEC Nord Kivu Butembo 14, Avenue Kinshasa , Commune de Mususa, Ville de Butembo 5 COOPEC LA SEMENCE Nord Kivu Butembo 5, Avenue Matokeo, Ville de Butembo 6 155, Avenue Mobutu, Quartier Buturande, Cité de Kiwanja, Territoire de COOPECCO/BUTURANDE Nord Kivu Buturande Rutshuru 7 COOPEC IMARA/GOMA Nord Kivu Goma Boulevard Kanyamuhanga , en face de ONC, Ville de Goma 8 COOPEC ADEC Nord Kivu Goma Avenue des Touristes, Quartier Mikeno, Maison Bercy Ville de Goma 9 COOPEC BONNE MOISSON Nord Kivu GOMA 12, Avenue Karisimbi, Quartier Mikeno, Commune de Goma, Ville de Goma 10 294, Avenue des Alizés , Quartier Murara, Commune Karisimbi, Ville de COOPEC KESHENI Nord Kivu Goma Goma 11 COOPEC TUJENGE PAMOJA Nord Kivu Goma 45, Boulevard Kayambayonga, Ville de Goma 12 COOPEC UMOJA NI NGUVU Nord Kivu GOMA 1, avenue Sake, Quartier Katoyi, Commune de Karisimbi, Ville de Goma 13 MECRE-BIRERE/COOPEC Nord Kivu Goma 11, Avenue du Commerce, Commune Karisimbi, Ville de Goma 14 MECREGO/COOPEC Nord Kivu Goma 30, Boulevard Kanyamuhanga, Quartier de Volcans, Ville de Goma 15 MECRE-KATINDO/COOPEC Nord Kivu Goma -

Download File
UNICEF DRC | Volcano Eruption (Goma) Situation Report Volcano Eruption Goma, DRC Situation Report #3 27 May 2021 Overview The eruption of Mount Nyiragongo on the evening of 22 May 2021, and the two lava flows have affected Kibumba park as well as Buhene and Kibati in the North-East of Goma, DRC. More than 20,000 people from Goma have fled Saké, 25 km north- west of Goma on the day of eruption. 32 people have died as a direct result of the eruption (either burned by the lava or asphyxiated by fumes), including three children, while 40 have been reported missing1. As of 26 May, it is estimated that the eruption directly affected 20 villages within the groupements of Kibati, Munigi and Mutaho, representing 3,629 burned houses2. This results in around more than 20,000 displaced population. (about 4,500 households according to OCHA). Map 1: Nyiragongo Volcano Eruption & Impacted Areas (source: UNICEF) More than 195,000 people, according to the WASH cluster3, might have difficulty in accessing safe water due to a disabled water reservoir and 25,000 persons had already their water access cut off, while access to electricity was cut off in large parts of Goma city. Seven schools (five primary schools4 and two secondary schools) have been affected. 1,957 students and 49 teachers have been affected at primary school level and while 447 students and 72 teachers are affected at secondary school level5. It has also been reported that 38 health centers (including ten in Goma Health Zone, 19 in Karisimbi Health Zone and nine in Nyiragongo Health Zone) have been affected by the volcanic eruption6.