Single Nucleotide Polymorphisms (Snps) of COL1A1 and COL11A1 in Class II Skeletal Malocclusion of Ethnic Javanese Patient
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Oral Diagnosis: the Clinician's Guide
Wright An imprint of Elsevier Science Limited Robert Stevenson House, 1-3 Baxter's Place, Leith Walk, Edinburgh EH I 3AF First published :WOO Reprinted 2002. 238 7X69. fax: (+ 1) 215 238 2239, e-mail: [email protected]. You may also complete your request on-line via the Elsevier Science homepage (http://www.elsevier.com). by selecting'Customer Support' and then 'Obtaining Permissions·. British Library Cataloguing in Publication Data A catalogue record for this book is available from the British Library Library of Congress Cataloging in Publication Data A catalog record for this book is available from the Library of Congress ISBN 0 7236 1040 I _ your source for books. journals and multimedia in the health sciences www.elsevierhealth.com Composition by Scribe Design, Gillingham, Kent Printed and bound in China Contents Preface vii Acknowledgements ix 1 The challenge of diagnosis 1 2 The history 4 3 Examination 11 4 Diagnostic tests 33 5 Pain of dental origin 71 6 Pain of non-dental origin 99 7 Trauma 124 8 Infection 140 9 Cysts 160 10 Ulcers 185 11 White patches 210 12 Bumps, lumps and swellings 226 13 Oral changes in systemic disease 263 14 Oral consequences of medication 290 Index 299 Preface The foundation of any form of successful treatment is accurate diagnosis. Though scientifically based, dentistry is also an art. This is evident in the provision of operative dental care and also in the diagnosis of oral and dental diseases. While diagnostic skills will be developed and enhanced by experience, it is essential that every prospective dentist is taught how to develop a structured and comprehensive approach to oral diagnosis. -

Tutankhamun's Dentition: the Pharaoh and His Teeth
Brazilian Dental Journal (2015) 26(6): 701-704 ISSN 0103-6440 http://dx.doi.org/10.1590/0103-6440201300431 1Department of Oral and Maxillofacial Tutankhamun’s Dentition: Surgery, University Hospital of Leipzig, Leipzig, Germany The Pharaoh and his Teeth 2Institute of Egyptology/Egyptian Museum Georg Steindorff, University of Leipzig, Leipzig, Germany 3Department of Orthodontics, University Hospital of Greifswald, Greifswald, Germany Niels Christian Pausch1, Franziska Naether2, Karl Friedrich Krey3 Correspondence: Dr. Niels Christian Pausch, Liebigstraße 12, 04103 Leipzig, Germany. Tel: +49- 341-97-21160. e-mail: niels. [email protected] Tutankhamun was a Pharaoh of the 18th Dynasty (New Kingdom) in ancient Egypt. Medical and radiological investigations of his skull revealed details about the jaw and teeth status of the mummy. Regarding the jaw relation, a maxillary prognathism, a mandibular retrognathism and micrognathism have been discussed previously. A cephalometric analysis was performed using a lateral skull X-ray and a review of the literature regarding Key Words: Tutankhamun’s King Tutankhamun´s mummy. The results imply diagnosis of mandibular retrognathism. dentition, cephalometric analysis, Furthermore, third molar retention and an incomplete, single cleft palate are present. mandibular retrognathism Introduction also been discussed (11). In 1922, the British Egyptologist Howard Carter found the undisturbed mummy of King Tutankhamun. The Case Report spectacular discovery enabled scientists of the following In the evaluation of Tutankhamun’s dentition and jaw decades to analyze the Pharaoh's remains. The mummy alignment, contemporary face reconstructions and coeval underwent multiple autopsies. Until now, little was artistic images can be of further use. However, the ancient published about the jaw and dentition of the King. -

Therapeutic Management of Patients with Class III Skeletal Malocclusion
Szpyt Justyna, Gębska Magdalena. Therapeutic management of patients with class III skeletal malocclusion. Mandibular prognathism, maxillary retrognathism – a case report. Journal of Education, Health and Sport. 2019;9(5):20-31. eISSN 2391-8306. DOI http://dx.doi.org/10.5281/zenodo.2656446 http://ojs.ukw.edu.pl/index.php/johs/article/view/6872 https://pbn.nauka.gov.pl/sedno-webapp/works/912455 The journal has had 7 points in Ministry of Science and Higher Education parametric evaluation. Part B item 1223 (26/01/2017). 1223 Journal of Education, Health and Sport eISSN 2391-8306 7 © The Authors 2019; This article is published with open access at Licensee Open Journal Systems of Kazimierz Wielki University in Bydgoszcz, Poland Open Access. This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author (s) and source are credited. This is an open access article licensed under the terms of the Creative Commons Attribution Non commercial license Share alike. (http://creativecommons.org/licenses/by-nc-sa/4.0/) which permits unrestricted, non commercial use, distribution and reproduction in any medium, provided the work is properly cited. The authors declare that there is no conflict of interests regarding the publication of this paper. Received: 15.04.2019. Revised: 25.04.2019. Accepted: 01.05.2019. Therapeutic management of patients with class III skeletal malocclusion. Mandibular prognathism, maxillary retrognathism – a case report Justyna Szpyt1, Magdalena Gębska2 1. Physiotherapy student, Faculty of Health Sciences, Pomeranian Medical University in Szczecin. -

Pan Imaging News V3 I4
Volume 4, Issue 4 US $6.00 Editor: Allan G. Farman, BDS, PhD (odont.), Assessing Growth and Development with Panoramic DSc (odont.), Diplomate of the Radiographs and Cephalometric Attachments: A critical American Board of Oral and Maxillofacial Radiology, Professor of tool for dental diagnosis and treatment planning Radiology and Imaging Sciences, Department of Surgical and Hospital By Dr. Allan G. Farman Dentistry, The University of It is recommended that radio- indicator of age is that the three Louisville School of Dentistry, graphs be made periodically including permanent molar teeth in each quad- Louisville, KY. both during the mixed dentition (8-9 rant erupt approximately at six-year year old) and adolescence (12-14 year intervals. The first permanent molar Featured Article: old) to evaluate growth and develop- erupts around 6 years, the second Assessing Growth and Development ment, and to look for asymptomatic permanent molar around 12 years, and with Panoramic Radiographs and dental disease [1-3]. Substantial the third molars around 18 years. Root Cephalometric Attachments: A critical differences in the assessed biological formation for permanent teeth is tool for dental diagnosis and and the known chronological age can completed roughly three years following treatment planning be indicators of a variety of inherited eruption. The first major attempt at and congenital conditions. Further, local developing a chronology for human In The Recent Literature: failure in dental eruption within the tooth development was that of Logan normal time range can be evidence of and Kronfeld (1933) and with minor Implantology dental impaction and possibly of a modification is still usable as a rough pathological process such as a hamar- and ready guide. -

Diseases of the Digestive System (KOO-K93)
CHAPTER XI Diseases of the digestive system (KOO-K93) Diseases of oral cavity, salivary glands and jaws (KOO-K14) lijell Diseases of pulp and periapical tissues 1m Dentofacial anomalies [including malocclusion] Excludes: hemifacial atrophy or hypertrophy (Q67.4) K07 .0 Major anomalies of jaw size Hyperplasia, hypoplasia: • mandibular • maxillary Macrognathism (mandibular)(maxillary) Micrognathism (mandibular)( maxillary) Excludes: acromegaly (E22.0) Robin's syndrome (087.07) K07 .1 Anomalies of jaw-cranial base relationship Asymmetry of jaw Prognathism (mandibular)( maxillary) Retrognathism (mandibular)(maxillary) K07.2 Anomalies of dental arch relationship Cross bite (anterior)(posterior) Dis to-occlusion Mesio-occlusion Midline deviation of dental arch Openbite (anterior )(posterior) Overbite (excessive): • deep • horizontal • vertical Overjet Posterior lingual occlusion of mandibular teeth 289 ICO-N A K07.3 Anomalies of tooth position Crowding Diastema Displacement of tooth or teeth Rotation Spacing, abnormal Transposition Impacted or embedded teeth with abnormal position of such teeth or adjacent teeth K07.4 Malocclusion, unspecified K07.5 Dentofacial functional abnormalities Abnormal jaw closure Malocclusion due to: • abnormal swallowing • mouth breathing • tongue, lip or finger habits K07.6 Temporomandibular joint disorders Costen's complex or syndrome Derangement of temporomandibular joint Snapping jaw Temporomandibular joint-pain-dysfunction syndrome Excludes: current temporomandibular joint: • dislocation (S03.0) • strain (S03.4) K07.8 Other dentofacial anomalies K07.9 Dentofacial anomaly, unspecified 1m Stomatitis and related lesions K12.0 Recurrent oral aphthae Aphthous stomatitis (major)(minor) Bednar's aphthae Periadenitis mucosa necrotica recurrens Recurrent aphthous ulcer Stomatitis herpetiformis 290 DISEASES OF THE DIGESTIVE SYSTEM Diseases of oesophagus, stomach and duodenum (K20-K31) Ill Oesophagitis Abscess of oesophagus Oesophagitis: • NOS • chemical • peptic Use additional external cause code (Chapter XX), if desired, to identify cause. -

The National Dental Practice-Based Research Network Adult Anterior
ORIGINAL ARTICLE The National Dental Practice-Based Research Network Adult Anterior Open Bite Study: Treatment recommendations and their association with patient and practitioner characteristics Greg Huang,a Camille Baltuck,b Ellen Funkhouser,c Hsuan-Fang (Cathy) Wang,a,d Lauren Todoki,a Sam Finkleman,a Peter Shapiro,a Roozbah Khosravi,a Hsiu-Ching (Joanna) Ko,a Geoffrey Greenlee,a Jaime De Jesus-Vinas,e Michael Vermette,f Matthew Larson,g Calogero Dolce,h Chung How Kau,i and David Harnick,j and the National Dental Practice-Based Research Network Collaborative Groupk Seattle, Wash, Portland, Ore, Birmingham, Ala, Taipei, Taiwan, San Juan, PR, Concord, NH, Eau Claire, Wis, Gainesville, Fla, and Albuquerque, NM Introduction: This aim of this paper is to describe and identify the practitioner and patient characteristics that are associated with treatment recommendations for adult anterior open bite patients across the United States. Methods: Practitioners and patients were recruited within the framework of the National Dental Practice-Based Research Network. Practitioners were asked about their demographic characteristics and their treatment recommendations for these patients. The practitioners also reported on their patients' dentofacial characteristics and provided initial cephalometric scans and intraoral photographs. Patients were asked about their demographic characteristics, previous orthodontic treatment, and goals for treatment. Four main treatment groups were evaluated: aligners, fixed appliances, temporary anchorage devices (TADs), and orthognathic surgery. Extractions were also investigated. Predictive multivariable models were created comparing various categories of treatment as well as extraction/nonextraction decisions. Results: Ninety-one practitioners (mostly orthodontists) and 347 patients were recruited from October 2015 to December 2016. Increased aligner recommendations were associated with white and Asian patients, the presence of tongue habits, and female practitioners. -

Abstracts from the 51St European Society of Human Genetics Conference: Electronic Posters
European Journal of Human Genetics (2019) 27:870–1041 https://doi.org/10.1038/s41431-019-0408-3 MEETING ABSTRACTS Abstracts from the 51st European Society of Human Genetics Conference: Electronic Posters © European Society of Human Genetics 2019 June 16–19, 2018, Fiera Milano Congressi, Milan Italy Sponsorship: Publication of this supplement was sponsored by the European Society of Human Genetics. All content was reviewed and approved by the ESHG Scientific Programme Committee, which held full responsibility for the abstract selections. Disclosure Information: In order to help readers form their own judgments of potential bias in published abstracts, authors are asked to declare any competing financial interests. Contributions of up to EUR 10 000.- (Ten thousand Euros, or equivalent value in kind) per year per company are considered "Modest". Contributions above EUR 10 000.- per year are considered "Significant". 1234567890();,: 1234567890();,: E-P01 Reproductive Genetics/Prenatal Genetics then compared this data to de novo cases where research based PO studies were completed (N=57) in NY. E-P01.01 Results: MFSIQ (66.4) for familial deletions was Parent of origin in familial 22q11.2 deletions impacts full statistically lower (p = .01) than for de novo deletions scale intelligence quotient scores (N=399, MFSIQ=76.2). MFSIQ for children with mater- nally inherited deletions (63.7) was statistically lower D. E. McGinn1,2, M. Unolt3,4, T. B. Crowley1, B. S. Emanuel1,5, (p = .03) than for paternally inherited deletions (72.0). As E. H. Zackai1,5, E. Moss1, B. Morrow6, B. Nowakowska7,J. compared with the NY cohort where the MFSIQ for Vermeesch8, A. -

Granular Cell Tumour of the Tongue in a 17Yearold Orthodontic Patient: A
bs_bs_banner Oral Surgery ISSN 1752-2471 CASE REPORT Granular cell tumour of the tongue in a 17-year-old orthodontic patient: a case report P.Hita-Davis1, P.Edwards2, S. Conley3 & T.J.Dyer4 1Oral Maxillofacial Surgery, School of Dentistry, Ann Arbor, MI, USA 2Department of Oral Pathology,Medicine and Radiology, Indiana University, Indianapolis, IN, USA 3Department of Orthodontics and Pediatric Dentistry, University of Michigan, Ann Arbor, MI, USA 4Oral Surgery, Boston University, Boston, MA, USA Key words: Abstract cyst, diagnosis, examination To describe the clinical presentation of a granular cell tumour (GCT) in an Correspondence to: orthodontic patient, as well as discuss its aetiology and treatment of Dr P Hita-Davis choice. We present a case of GCT of the tongue in an otherwise healthy Oral Maxillofacial Surgery 17-year-old male patient along with a brief review of literature on GCTs. School of Dentistry The lesion was surgically excised and orthodontic treatment was success- 1011 N. University Avenue Ann Arbor, MI 48109 fully finalised. Clinically, GCTs are indistinguishable from other benign USA connective tissue and neural tissue neoplasms and may be found in any Tel.:+1 734 764 1542 site, with cases commonly involving the gastrointestinal system, breast Fax: +1 734 615 8399 and lung. However, over 50% of cases involve the head and neck, with email: [email protected] the tongue being the most frequently involved site (65–85% of oral GCTs). GCTs demonstrate a close anatomical relationship with peripheral Accepted: 6 June 2013 nerve fibres and demonstrate the presence of myelin and axon-like doi:10.1111/ors.12055 structures thus lending credence to their neural origin. -

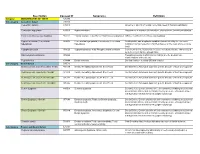
Common Icd-10 Dental Codes
COMMON ICD-10 DENTAL CODES SERVICE PROVIDERS SHOULD BE AWARE THAT AN ICD-10 CODE IS A DIAGNOSTIC CODE. i.e. A CODE GIVING THE REASON FOR A PROCEDURE; SO THERE MIGHT BE MORE THAN ONE ICD-10 CODE FOR A PARTICULAR PROCEDURE CODE AND THE SERVICE PROVIDER NEEDS TO SELECT WHICHEVER IS THE MOST APPROPRIATE. ICD10 Code ICD-10 DESCRIPTOR FROM WHO (complete) OWN REFERENCE / INTERPRETATION/ CIRCUM- STANCES IN WHICH THESE ICD-10 CODES MAY BE USED TIP:If you are viewing this electronically, in order to locate any word in the document, click CONTROL-F and type in word you are looking for. K00 Disorders of tooth development and eruption Not a valid code. Heading only. K00.0 Anodontia Congenitally missing teeth - complete or partial K00.1 Supernumerary teeth Mesiodens K00.2 Abnormalities of tooth size and form Macr/micro-dontia, dens in dente, cocrescence,fusion, gemination, peg K00.3 Mottled teeth Fluorosis K00.4 Disturbances in tooth formation Enamel hypoplasia, dilaceration, Turner K00.5 Hereditary disturbances in tooth structure, not elsewhere classified Amylo/dentino-genisis imperfecta K00.6 Disturbances in tooth eruption Natal/neonatal teeth, retained deciduous tooth, premature, late K00.7 Teething syndrome Teething K00.8 Other disorders of tooth development Colour changes due to blood incompatability, biliary, porphyria, tetyracycline K00.9 Disorders of tooth development, unspecified K01 Embedded and impacted teeth Not a valid code. Heading only. K01.0 Embedded teeth Distinguish from impacted tooth K01.1 Impacted teeth Impacted tooth (in contact with another tooth) K02 Dental caries Not a valid code. Heading only. -

Dental Health Following Cancer Treatment
Survivorship Clinic Dental health following cancer treatment Treatment for cancer often increases the risk for dental problems. As a cancer survivor, it is important for you to understand the reasons why dental care is especially important for maintaining your health. What are the risk factors for dental problems after cancer treatment? Treatment with chemotherapy before your permanent teeth were fully formed. Radiation that included the mouth and/or salivary glands, such as the following: Cranial (whole brain) Craniospinal Nasopharyngeal (nose and throat) Oropharyngeal (mouth and throat) Orbital Eye Ear Infratemporal (midfacial area behind the cheekbones) Cervical (neck) Cervical spine (spine in the neck area) Mantle (neck and chest areas) Total body irradiation (TBI) What dental problems can occur following treatment for cancer? Problems that may be a result of chemotherapy include: Increased risk for cavities Shortening or thinning of the roots of the teeth Absence of teeth or roots Problems with development of tooth enamel resulting in white or discolored patches on the teeth, grooves and pits in the teeth, and/or Easy staining of the teeth Because teeth develop slowly, these problems are more likely to develop in people who received chemotherapy over a prolonged period (several years). Fred Hutchinson Cancer Research Center Survivorship Program Survivorship Clinic Problems that may be a result of radiation to the mouth and/or salivary glands include: Increased risk for cavities Shortening or thinning of the roots -

Congenital Hypothyrodism and Its Oral Manifestations Hipotiroidismo Congénito Y Sus Manifestaciones Bucales
www.medigraphic.org.mx Revista Odontológica Mexicana Facultad de Odontología Vol. 18, No. 2 April-June 2014 pp 133-138 CASE REPORT Congenital hypothyrodism and its oral manifestations Hipotiroidismo congénito y sus manifestaciones bucales Marxy E Reynoso Rodríguez,* María A Monter García,§ Ignacio Sánchez FloresII ABSTRACT RESUMEN Hypothyroidism is one of the most common thyroid disorders. El hipotiroidismo es el más común de los trastornos de la tiroides, Hypothyroidism can be congenital in cases when the thyroid puede ser congénito si la glándula tiroides no se desarrolla correc- gland does not develop normally. Female predominance is a tamente (hipotiroidismo congénito). La predominancia femenina es characteristic of congenital hypothyroidism. Dental characteristics una característica. Entre las características odontológicas del hi- of hypothyroidism are thick lips, a large-sized tongue which, due potiroidismo se observan labios gruesos, lengua de gran tamaño, to its position, can elicit anterior open bite as well as fanned-out que debido a su posición suele producir mordida abierta anterior y anterior teeth. In these cases, delayed eruption of primary and dientes anteriores en abanico, destaca que la dentición temporal y permanent dentitions can be observed, and teeth, even though permanente presentan un retardo eruptivo característico y, aunque normal-sized, are crowded due to the small-sized jaws. This study los dientes son de tamaño normal, suelen estar apiñados por el ta- presents clinical cases of female patients diagnosed with congenital maño pequeño de los maxilares. Se presentan dos casos clínicos hypothyroidism who sought treatment at the Dental Pediatrics Unit de pacientes de sexo femenino que acuden a la clínica de Especia- of the Autonomous University of the State of Mexico. -
Description Concept ID Synonyms Definition
Description Concept ID Synonyms Definition Category ABNORMALITIES OF TEETH 426390 Subcategory Cementum Defect 399115 Cementum aplasia 346218 Absence or paucity of cellular cementum (seen in hypophosphatasia) Cementum hypoplasia 180000 Hypocementosis Disturbance in structure of cementum, often seen in Juvenile periodontitis Florid cemento-osseous dysplasia 958771 Familial multiple cementoma; Florid osseous dysplasia Diffuse, multifocal cementosseous dysplasia Hypercementosis (Cementation 901056 Cementation hyperplasia; Cementosis; Cementum An idiopathic, non-neoplastic condition characterized by the excessive hyperplasia) hyperplasia buildup of normal cementum (calcified tissue) on the roots of one or more teeth Hypophosphatasia 976620 Hypophosphatasia mild; Phosphoethanol-aminuria Cementum defect; Autosomal recessive hereditary disease characterized by deficiency of alkaline phosphatase Odontohypophosphatasia 976622 Hypophosphatasia in which dental findings are the predominant manifestations of the disease Pulp sclerosis 179199 Dentin sclerosis Dentinal reaction to aging OR mild irritation Subcategory Dentin Defect 515523 Dentinogenesis imperfecta (Shell Teeth) 856459 Dentin, Hereditary Opalescent; Shell Teeth Dentin Defect; Autosomal dominant genetic disorder of tooth development Dentinogenesis Imperfecta - Shield I 977473 Dentin, Hereditary Opalescent; Shell Teeth Dentin Defect; Autosomal dominant genetic disorder of tooth development Dentinogenesis Imperfecta - Shield II 976722 Dentin, Hereditary Opalescent; Shell Teeth Dentin Defect;