Orphanet Journal of Rare Diseases Biomed Central
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

On the Active Site Thiol of Y-Glutamylcysteine Synthetase
Proc. Natl. Acad. Sci. USA Vol. 85, pp. 2464-2468, April 1988 Biochemistry On the active site thiol of y-glutamylcysteine synthetase: Relationships to catalysis, inhibition, and regulation (glutathione/cystamine/Escherichia coli/kidney/enzyme inactivation) CHIN-SHIou HUANG, WILLIAM R. MOORE, AND ALTON MEISTER Cornell University Medical College, Department of Biochemistry, 1300 York Avenue, New York, NY 10021 Contributed by Alton Meister, December 4, 1987 ABSTRACT y-Glutamylcysteine synthetase (glutamate- dithiothreitol, suggesting that cystamine forms a mixed cysteine ligase; EC 6.3.2.2) was isolated from an Escherichia disulfide between cysteamine and an enzyme thiol (15). coli strain enriched in the gene for this enzyme by recombinant Inactivation of the enzyme by the L- and D-isomers of DNA techniques. The purified enzyme has a specific activity of 3-amino-1-chloro-2-pentanone, as well as that by cystamine, 1860 units/mg and a molecular weight of 56,000. Comparison is prevented by L-glutamate (14). Treatment of the enzyme of the E. coli enzyme with the well-characterized rat kidney with cystamine prevents its interaction with the sulfoxi- enzyme showed that these enzymes have similar catalytic prop- mines. Titration of the enzyme with 5,5'-dithiobis(2- erties (apparent Km values, substrate specificities, turnover nitrobenzoate) reveals that the enzyme has a single exposed numbers). Both enzymes are feedback-inhibited by glutathione thiol that reacts with this reagent without affecting activity but not by y-glutamyl-a-aminobutyrylglycine; the data indicate (16). 5,5'-Dithiobis(2-nitrobenzoate) does not interact with that glutathione binds not only at the glutamate binding site but the thiol that reacts with cystamine. -

Review Article Cystathionine -Synthase in Physiology and Cancer
Hindawi BioMed Research International Volume 2018, Article ID 3205125, 11 pages https://doi.org/10.1155/2018/3205125 Review Article Cystathionine �-Synthase in Physiology and Cancer Haoran Zhu,1,2 Shaun Blake,1,2 Keefe T. Chan,1 Richard B. Pearson ,1,2,3,4 and Jian Kang 1 1 Division of Research, Peter MacCallum Cancer Centre, 305 Grattan Street, Melbourne, Victoria 3000, Australia 2Sir Peter MacCallum Department of Oncology, Australia 3Department of Biochemistry and Molecular Biology, University of Melbourne, Parkville, Victoria 3052, Australia 4Department of Biochemistry and Molecular Biology, Monash University, Clayton, Victoria 3168, Australia Correspondence should be addressed to Richard B. Pearson; [email protected] Received 23 March 2018; Accepted 29 May 2018; Published 28 June 2018 Academic Editor: Maria L. Tornesello Copyright © 2018 Haoran Zhu et al. Tis is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Cystathionine �-synthase (CBS) regulates homocysteine metabolism and contributes to hydrogen sulfde (H2S) biosynthesis through which it plays multifunctional roles in the regulation of cellular energetics, redox status, DNA methylation, and protein modifcation. Inactivating mutations in CBS contribute to the pathogenesis of the autosomal recessive disease CBS-defcient homocystinuria. Recent studies demonstrating that CBS promotes colon and ovarian cancer growth in preclinical models highlight a newly identifed oncogenic role for CBS. On the contrary, tumor-suppressive efects of CBS have been reported in other cancer types, suggesting context-dependent roles of CBS in tumor growth and progression. Here, we review the physiological functions of CBS, summarize the complexities regarding CBS research in oncology, and discuss the potential of CBS and its key metabolites, including homocysteine and H2S, as potential biomarkers for cancer diagnosis or therapeutic targets for cancer treatment. -

Product Sheet Info
Master Clone List for NR-19279 ® Vibrio cholerae Gateway Clone Set, Recombinant in Escherichia coli, Plates 1-46 Catalog No. NR-19279 Table 1: Vibrio cholerae Gateway® Clones, Plate 1 (NR-19679) Clone ID Well ORF Locus ID Symbol Product Accession Position Length Number 174071 A02 367 VC2271 ribD riboflavin-specific deaminase NP_231902.1 174346 A03 336 VC1877 lpxK tetraacyldisaccharide 4`-kinase NP_231511.1 174354 A04 342 VC0953 holA DNA polymerase III, delta subunit NP_230600.1 174115 A05 388 VC2085 sucC succinyl-CoA synthase, beta subunit NP_231717.1 174310 A06 506 VC2400 murC UDP-N-acetylmuramate--alanine ligase NP_232030.1 174523 A07 132 VC0644 rbfA ribosome-binding factor A NP_230293.2 174632 A08 322 VC0681 ribF riboflavin kinase-FMN adenylyltransferase NP_230330.1 174930 A09 433 VC0720 phoR histidine protein kinase PhoR NP_230369.1 174953 A10 206 VC1178 conserved hypothetical protein NP_230823.1 174976 A11 213 VC2358 hypothetical protein NP_231988.1 174898 A12 369 VC0154 trmA tRNA (uracil-5-)-methyltransferase NP_229811.1 174059 B01 73 VC2098 hypothetical protein NP_231730.1 174075 B02 82 VC0561 rpsP ribosomal protein S16 NP_230212.1 174087 B03 378 VC1843 cydB-1 cytochrome d ubiquinol oxidase, subunit II NP_231477.1 174099 B04 383 VC1798 eha eha protein NP_231433.1 174294 B05 494 VC0763 GTP-binding protein NP_230412.1 174311 B06 314 VC2183 prsA ribose-phosphate pyrophosphokinase NP_231814.1 174603 B07 108 VC0675 thyA thymidylate synthase NP_230324.1 174474 B08 466 VC1297 asnS asparaginyl-tRNA synthetase NP_230942.2 174933 B09 198 -

A Mathematical Model of Glutathione Metabolism Michael C Reed*1, Rachel L Thomas1, Jovana Pavisic1,2, S Jill James3, Cornelia M Ulrich4 and H Frederik Nijhout2
Theoretical Biology and Medical Modelling BioMed Central Research Open Access A mathematical model of glutathione metabolism Michael C Reed*1, Rachel L Thomas1, Jovana Pavisic1,2, S Jill James3, Cornelia M Ulrich4 and H Frederik Nijhout2 Address: 1Department of Mathematics, Duke University, Durham, NC 27708, USA, 2Department of Biology, Duke University, Durham, NC 27708, USA, 3Department of Pediatrics, University of Arkansas for Medical Sciences, Little Rock, AK 72205, USA and 4Fred Hutchinson Cancer Research Center, Seattle, WA 98109-1024, USA Email: Michael C Reed* - [email protected]; Rachel L Thomas - [email protected]; Jovana Pavisic - [email protected]; S Jill James - [email protected]; Cornelia M Ulrich - [email protected]; H Frederik Nijhout - [email protected] * Corresponding author Published: 28 April 2008 Received: 27 November 2007 Accepted: 28 April 2008 Theoretical Biology and Medical Modelling 2008, 5:8 doi:10.1186/1742-4682-5-8 This article is available from: http://www.tbiomed.com/content/5/1/8 © 2008 Reed et al; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Abstract Background: Glutathione (GSH) plays an important role in anti-oxidant defense and detoxification reactions. It is primarily synthesized in the liver by the transsulfuration pathway and exported to provide precursors for in situ GSH synthesis by other tissues. Deficits in glutathione have been implicated in aging and a host of diseases including Alzheimer's disease, Parkinson's disease, cardiovascular disease, cancer, Down syndrome and autism. -

Supplementary Information
Supplementary information (a) (b) Figure S1. Resistant (a) and sensitive (b) gene scores plotted against subsystems involved in cell regulation. The small circles represent the individual hits and the large circles represent the mean of each subsystem. Each individual score signifies the mean of 12 trials – three biological and four technical. The p-value was calculated as a two-tailed t-test and significance was determined using the Benjamini-Hochberg procedure; false discovery rate was selected to be 0.1. Plots constructed using Pathway Tools, Omics Dashboard. Figure S2. Connectivity map displaying the predicted functional associations between the silver-resistant gene hits; disconnected gene hits not shown. The thicknesses of the lines indicate the degree of confidence prediction for the given interaction, based on fusion, co-occurrence, experimental and co-expression data. Figure produced using STRING (version 10.5) and a medium confidence score (approximate probability) of 0.4. Figure S3. Connectivity map displaying the predicted functional associations between the silver-sensitive gene hits; disconnected gene hits not shown. The thicknesses of the lines indicate the degree of confidence prediction for the given interaction, based on fusion, co-occurrence, experimental and co-expression data. Figure produced using STRING (version 10.5) and a medium confidence score (approximate probability) of 0.4. Figure S4. Metabolic overview of the pathways in Escherichia coli. The pathways involved in silver-resistance are coloured according to respective normalized score. Each individual score represents the mean of 12 trials – three biological and four technical. Amino acid – upward pointing triangle, carbohydrate – square, proteins – diamond, purines – vertical ellipse, cofactor – downward pointing triangle, tRNA – tee, and other – circle. -

Gamma-Glutamyltransferase 1 Promotes Clear Cell Renal Cell Carcinoma Initiation and Progression
Author Manuscript Published OnlineFirst on May 31, 2019; DOI: 10.1158/1541-7786.MCR-18-1204 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Gamma-glutamyltransferase 1 promotes clear cell renal cell carcinoma initiation and progression Ankita Bansal1, Danielle J. Sanchez1,2, Vivek Nimgaonkar1, David Sanchez1, Romain Riscal1, Nicolas Skuli1, M. Celeste Simon1,2* 1Abramson Family Cancer Research Institute, 456 BRB II/III, 421 Curie Boulevard, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA 19104-6160, USA 2Department of Cell and Developmental Biology, 456 BRB II/III, 421 Curie Boulevard, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA 19104-6160, USA Running Title: GGT1 in clear cell renal cell carcinoma * Corresponding Author: Dr. M. Celeste Simon, Ph.D. Abramson Family Cancer Research Institute, 456 BRB II/III, 421 Curie Boulevard, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA 19104-6160, USA, Email: [email protected] Phone: 215-746-5532 Keywords: cancer metabolism, kidney cancer, glutathione, GGT1, chemotherapy Financial Support: This work was supported by NIH grant P01CA104838 to M.C.S. Conflicts of Interest Statement: The authors declare that no conflict of interest exists. Word Count: 4872 (excluding references and figure legends) Figures: 6 primary figures, 6 supplemental figures 1 Downloaded from mcr.aacrjournals.org on September 25, 2021. © 2019 American Association for Cancer Research. Author Manuscript Published OnlineFirst on May 31, 2019; DOI: 10.1158/1541-7786.MCR-18-1204 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. -
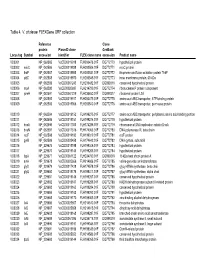
Table 4. V. Cholerae Flexgene ORF Collection
Table 4. V. cholerae FLEXGene ORF collection Reference Clone protein PlasmID clone GenBank Locus tag Symbol accession identifier FLEX clone name accession Product name VC0001 NP_062585 VcCD00019918 FLH200476.01F DQ772770 hypothetical protein VC0002 mioC NP_062586 VcCD00019938 FLH200506.01F DQ772771 mioC protein VC0003 thdF NP_062587 VcCD00019958 FLH200531.01F DQ772772 thiophene and furan oxidation protein ThdF VC0004 yidC NP_062588 VcCD00019970 FLH200545.01F DQ772773 inner membrane protein, 60 kDa VC0005 NP_062589 VcCD00061243 FLH236482.01F DQ899316 conserved hypothetical protein VC0006 rnpA NP_062590 VcCD00025697 FLH214799.01F DQ772774 ribonuclease P protein component VC0007 rpmH NP_062591 VcCD00061229 FLH236450.01F DQ899317 ribosomal protein L34 VC0008 NP_062592 VcCD00019917 FLH200475.01F DQ772775 amino acid ABC transporter, ATP-binding protein VC0009 NP_062593 VcCD00019966 FLH200540.01F DQ772776 amino acid ABC transproter, permease protein VC0010 NP_062594 VcCD00019152 FLH199275.01F DQ772777 amino acid ABC transporter, periplasmic amino acid-binding portion VC0011 NP_062595 VcCD00019151 FLH199274.01F DQ772778 hypothetical protein VC0012 dnaA NP_062596 VcCD00017363 FLH174286.01F DQ772779 chromosomal DNA replication initiator DnaA VC0013 dnaN NP_062597 VcCD00017316 FLH174063.01F DQ772780 DNA polymerase III, beta chain VC0014 recF NP_062598 VcCD00019182 FLH199319.01F DQ772781 recF protein VC0015 gyrB NP_062599 VcCD00025458 FLH174642.01F DQ772782 DNA gyrase, subunit B VC0016 NP_229675 VcCD00019198 FLH199346.01F DQ772783 hypothetical protein -

Diseases Catalogue
Diseases catalogue AA Disorders of amino acid metabolism OMIM Group of disorders affecting genes that codify proteins involved in the catabolism of amino acids or in the functional maintenance of the different coenzymes. AA Alkaptonuria: homogentisate dioxygenase deficiency 203500 AA Phenylketonuria: phenylalanine hydroxylase (PAH) 261600 AA Defects of tetrahydrobiopterine (BH 4) metabolism: AA 6-Piruvoyl-tetrahydropterin synthase deficiency (PTS) 261640 AA Dihydropteridine reductase deficiency (DHPR) 261630 AA Pterin-carbinolamine dehydratase 126090 AA GTP cyclohydrolase I deficiency (GCH1) (autosomal recessive) 233910 AA GTP cyclohydrolase I deficiency (GCH1) (autosomal dominant): Segawa syndrome 600225 AA Sepiapterin reductase deficiency (SPR) 182125 AA Defects of sulfur amino acid metabolism: AA N(5,10)-methylene-tetrahydrofolate reductase deficiency (MTHFR) 236250 AA Homocystinuria due to cystathionine beta-synthase deficiency (CBS) 236200 AA Methionine adenosyltransferase deficiency 250850 AA Methionine synthase deficiency (MTR, cblG) 250940 AA Methionine synthase reductase deficiency; (MTRR, CblE) 236270 AA Sulfite oxidase deficiency 272300 AA Molybdenum cofactor deficiency: combined deficiency of sulfite oxidase and xanthine oxidase 252150 AA S-adenosylhomocysteine hydrolase deficiency 180960 AA Cystathioninuria 219500 AA Hyperhomocysteinemia 603174 AA Defects of gamma-glutathione cycle: glutathione synthetase deficiency (5-oxo-prolinuria) 266130 AA Defects of histidine metabolism: Histidinemia 235800 AA Defects of lysine and -

Nineteen-Year Follow-Up of a Patient with Severe Glutathione Synthetase Deficiency
Journal of Human Genetics (2016) 61, 669–672 & 2016 The Japan Society of Human Genetics All rights reserved 1434-5161/16 www.nature.com/jhg SHORT COMMUNICATION Nineteen-year follow-up of a patient with severe glutathione synthetase deficiency Paldeep S Atwal1,2, Casey R Medina1, Lindsay C Burrage1 and V Reid Sutton1 Glutathione synthetase deficiency is a rare autosomal recessive disorder resulting in low levels of glutathione and an increased susceptibility to oxidative stress. Patients with glutathione synthetase deficiency typically present in the neonatal period with hemolytic anemia, metabolic acidosis and neurological impairment. Lifelong treatment with antioxidants has been recommended in an attempt to prevent morbidity and mortality associated with the disorder. Here, we present a 19-year-old female who was diagnosed with glutathione synthetase deficiency shortly after birth and who has been closely followed in our metabolic clinic. Despite an initial severe presentation, she has had normal intellectual development and few complications of her disorder with a treatment regimen that includes polycitra (citric acid, potassium citrate and sodium citrate), vitamin C, vitamin E and selenium. Journal of Human Genetics (2016) 61, 669–672; doi:10.1038/jhg.2016.20; published online 17 March 2016 INTRODUCTION patients with GSSD due to the accumulation of γ-glutamylcysteine Glutathione (GSH) is a ubiquitous tripeptide (L-y-glutamyl-L-cystei- being hydrolyzed to 5-oxoproline and cysteine by γ-glutamyl cyclo- nylglycine) known to function in many aspects of cellular activity transferase. This accumulation of 5-oxoproline exceeds the capacity of including protein and DNA synthesis, transport, detoxification of 5-oxoprolinase leading to high urinary excretion of 5-oxoproline that xenobiotics and carcinogens, metabolism, and defense against free is detectable on urine organic acid analysis.6 In the present report, 1 γ radicals and oxidative stress. -

The Glutathione Cycle Shapes Synaptic Glutamate Activity
bioRxiv preprint doi: https://doi.org/10.1101/325530; this version posted October 17, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. The glutathione cycle shapes synaptic glutamate activity Thomas W. Sedlaka, 1,2, Bindu D. Paulb,1, Greg M. Parkera,b, Lynda D. Hesterb, Yu Taniguchia, Atsushi Kamiyaa, Solomon H. Snyder,a,b,c,2, Akira Sawaa aDepartment of Psychiatry, Johns Hopkins University School of Medicine, Baltimore, Maryland 21205, USA bThe Solomon H. Snyder Department of Neuroscience, Johns Hopkins University School of Medicine, Baltimore, Maryland 21205, USA cDepartment of Pharmacology and Molecular Sciences, Johns Hopkins University School of Medicine, Baltimore, Maryland 21205, USA 1T.W.S. and B.D.P. contributed equally to this work. 2Corresponding authors Correspondence to: [email protected] [email protected] 1 bioRxiv preprint doi: https://doi.org/10.1101/325530; this version posted October 17, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Abstract Glutamate is the most abundant excitatory neurotransmitter, present at the bulk of cortical synapses, and participating in many physiologic and pathologic processes ranging from learning and memory to stroke. The tripeptide, glutathione, is one third glutamate and present at up to low millimolar intracellular concentrations in brain, mediating antioxidant defenses and drug detoxification. Because of the substantial amounts of brain glutathione and its rapid turnover under homeostatic control, we hypothesized that glutathione is a relevant reservoir of glutamate, and could influence synaptic excitability. -

Parental Selenium Nutrition Affects the One-Carbon Metabolism
life Article Parental Selenium Nutrition Affects the One-Carbon Metabolism and the Hepatic DNA Methylation Pattern of Rainbow Trout (Oncorhynchus mykiss) in the Progeny 1, 2, 1 1 Pauline Wischhusen y , Takaya Saito y ,Cécile Heraud , Sadasivam J. Kaushik , 1 2 1, , Benoit Fauconneau , Philip Antony Jesu Prabhu , Stéphanie Fontagné-Dicharry * y 2, and Kaja H. Skjærven y 1 INRAE, University of Pau and Pays de l’Adour, E2S UPPA, NUMEA, 64310 Saint Pee sur Nivelle, France; [email protected] (P.W.); [email protected] (C.H.); [email protected] (S.J.K.); [email protected] (B.F.) 2 Institute of Marine Research, P.O. Box 1870, 5020 Bergen, Norway; [email protected] (T.S.); [email protected] (P.A.J.P.); [email protected] (K.H.S.) * Correspondence: [email protected] These authors contributed equally to this work. y Received: 11 June 2020; Accepted: 23 July 2020; Published: 25 July 2020 Abstract: Selenium is an essential micronutrient and its metabolism is closely linked to the methionine cycle and transsulfuration pathway. The present study evaluated the effect of two different selenium supplements in the diet of rainbow trout (Onchorhynchus mykiss) broodstock on the one-carbon metabolism and the hepatic DNA methylation pattern in the progeny. Offspring of three parental groups of rainbow trout, fed either a control diet (NC, basal Se level: 0.3 mg/kg) or a diet supplemented with sodium selenite (SS, 0.8 mg Se/kg) or hydroxy-selenomethionine (SO, 0.7 mg Se/kg), were collected at swim-up fry stage. -

SSIEM Classification of Inborn Errors of Metabolism 2011
SSIEM classification of Inborn Errors of Metabolism 2011 Disease group / disease ICD10 OMIM 1. Disorders of amino acid and peptide metabolism 1.1. Urea cycle disorders and inherited hyperammonaemias 1.1.1. Carbamoylphosphate synthetase I deficiency 237300 1.1.2. N-Acetylglutamate synthetase deficiency 237310 1.1.3. Ornithine transcarbamylase deficiency 311250 S Ornithine carbamoyltransferase deficiency 1.1.4. Citrullinaemia type1 215700 S Argininosuccinate synthetase deficiency 1.1.5. Argininosuccinic aciduria 207900 S Argininosuccinate lyase deficiency 1.1.6. Argininaemia 207800 S Arginase I deficiency 1.1.7. HHH syndrome 238970 S Hyperammonaemia-hyperornithinaemia-homocitrullinuria syndrome S Mitochondrial ornithine transporter (ORNT1) deficiency 1.1.8. Citrullinemia Type 2 603859 S Aspartate glutamate carrier deficiency ( SLC25A13) S Citrin deficiency 1.1.9. Hyperinsulinemic hypoglycemia and hyperammonemia caused by 138130 activating mutations in the GLUD1 gene 1.1.10. Other disorders of the urea cycle 238970 1.1.11. Unspecified hyperammonaemia 238970 1.2. Organic acidurias 1.2.1. Glutaric aciduria 1.2.1.1. Glutaric aciduria type I 231670 S Glutaryl-CoA dehydrogenase deficiency 1.2.1.2. Glutaric aciduria type III 231690 1.2.2. Propionic aciduria E711 232000 S Propionyl-CoA-Carboxylase deficiency 1.2.3. Methylmalonic aciduria E711 251000 1.2.3.1. Methylmalonyl-CoA mutase deficiency 1.2.3.2. Methylmalonyl-CoA epimerase deficiency 251120 1.2.3.3. Methylmalonic aciduria, unspecified 1.2.4. Isovaleric aciduria E711 243500 S Isovaleryl-CoA dehydrogenase deficiency 1.2.5. Methylcrotonylglycinuria E744 210200 S Methylcrotonyl-CoA carboxylase deficiency 1.2.6. Methylglutaconic aciduria E712 250950 1.2.6.1. Methylglutaconic aciduria type I E712 250950 S 3-Methylglutaconyl-CoA hydratase deficiency 1.2.6.2.