A Study of Health Workers' Knowledge and Practices Regarding Leprosy Care and Control at Primary Care Clinics in the Eerstehoe
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Proposed Main Seat / Sub District Within the Proposed Magisterial District Ermelo Main Seat of Msukaligwa Magisterial District
# # !C # # ### !C^ !.C# # # # !C # # # # # # # # # # ^!C # # # # # # # ^ # # ^ # # !C # ## # # # # # # # # # # # # # # # # !C# # !C # # # # # # # # # #!C # # # # # # #!C# # # # # # !C ^ # # # # # # # # # # # # ^ # # # # !C # !C # #^ # # # # # # ## # #!C # # # # # # ## !C# # # # # # # !C# ## # # # # # !C # # !C# # # # #^ # # # # # # # ## # # # # # !C # # # # ## # # # # # # ## # ## #!C # # # # # # # # # # !C # # # ## # # ## # # # # # # !C # # # ##!C ## ## ## # # # # # # # # # #^ # # ## # # # !C # # !C# # # # # # # # # # # # # # # # # # # # # # # # # # #!C # ## # ##^ # !C #!C## # # # # # # # # # # # # # ## # ## # # # !C# ^ ## # # # # # # # # # # # # # # # # # # # # # # ## # # # # # # !C # #!C # # #!C # # !C## # # # # # # !C# # # # # # # # # # ## # # # ## # ## ## # # # # # # # ## # # # # # # # # # # # # # # # # # # # # # ## # # #!C # # # ## # # # # # # # # # # ^!C # # # # # ^ # # # # # # ## # # # # # # # ## # # # # # # #!C # # !C # # !C ## # # # # #!C # # # !C# # # # # # # # # # # # # ## # # # !C# # ## # ## # # ## # # # # # # # # # # # # # # !C # # # # # # # ### #!C# # # !C !C# # !C # ## # # # # # # # # !C# # !.# # # # ## ## # #!C# # # # # # # # ## # # # # # # # # # # # # ### ##^ # # # # # # # ## # # # # ^ # !C# ## # # # # # # !C## # ## # # # # ## # # # # # ## # # # # #!C## !C# # !C# ## # !C### # # ^ # # # !C ### # # # !C# ##!C # !C # # # ^ !C ## # # #!C # ## ## # # ## # # # # # # ## !C# # # # # # # # ## # # # # # !C # ## ## # # # # !C # # ^ # ## # ## # # # !.!C ## # # ## # # # # !C # # !C# # ### # # # # # # # # # # ## !C # # # # ## !C # -

MPUMALANGA PROVINCE – 297 Cdws NKANGALA DISTRICT
MPUMALANGA PROVINCE – 297 CDWs NKANGALA DISTRICT Name & Surname Physical Address ID Numbers Contact Numbers Municipality 1. Mirriam Mbuli 693 Emthonjeni 6407170302088 0731969483 Emakhazeni MACHADODORP 2. Nonhlanhla Vivian P.O Box 1004 8207160765080 0736357262 Emakhazeni Shabangu EMAKHAZENI 3. Klara Mthombeni P.O. BOX 15 8209050295087 013-2467414 Emakhazeni WONDERFONTEIN 4. Simon Popoyi Mohlala P.O. BOX 194 BELFAST 7512285542087 0786090617 Emakhazeni 5. Philemon Nqabanisi P.O. BOX 687 BELFAST 8109175658088 0720231783 Emakhazeni Mabuza 6. Frans Mahlangu 6301055486084 0839991809 Emakhazeni 7. Yvonne Maredi 8006201124087 0762161706 Emakhazeni 8. Lungile Sibande 285 Emthonjeni 7709260474084 0825136338 Emakhazeni Machadodorp 1170 9. Sipho Prince Maseko Stand no:264 Mgwenya 7510235628085 0836880588 Emakhazeni Location WatervalBoven 10. Ntombizodwa Zwane 1626 Siyathuthuka Belfast 0735676763 Emakhazeni 1102 11. Evelyn Mahlangu 7708070300083 Emakhazeni 12. Thulisile Ellen Mabanga P.O. BOX 1195 DELMAS 8205240609088 0761907755 Delmas 13. Jan Zandile Mahlangu P.O. BOX 2938 DELMAS 7612285639089 0725624841 Delmas 14. Linah Nomathemba P.O. BOX 4867 DELMAS 6808160565081 0833621604 Delmas Mahlangu 15. Beki Shabalala P.O. BOX 2221 DELMAS 6007025474080 0827854905 Delmas 16. RankitsingJohannes 936 Deipark DELMAS 2210 7305065908085 0732679701 Delmas Sepenyane 17. Hendrietta Mabanga 249 Botleng Delmas 2210 8312150350081 0720634450 Delmas 18. Siponono Mahlangu Plot 14 Leeupoort Farm 7611060848089 0733837296 Delmas Delmas 2210 19. John Mabena 1062 Botleng Delmas 2210 6601135378080 0727728825 Delmas 20. Kgamelo Andrew Kgomo 17 Somerset Nasarethe 5301016791086 0843770203 Steve Tshwete MIDDELBURG 4066282802 21. Mandla Ellias Masango 678 MIDDELBURG 5701095753081 0729142819 Steve Tshwete 22. Josta Mpereke 2389 MIDDELBURG 5701015517087 0834446879 Steve Tshwete 23. Bhekumuzi Evans 3483 Melato Street 8309165421089 0835167888 Steve Tshwete Simelane MIDDELBURGt 24. Thulani Jeffrey Nkosi 3254 Ext 1 Mangosuthu 8208305352081 0737873361 Steve Tshwete MIDDELBURG 25. -

PHARMACEUTICAL SERVICES Centre: Provincial Office, Nelspruit Salary: R1 185 879 – 1 355 916 P.A
MPUMALANGA PROVINCE DEPARTMENT OF HEALTH “SIYANAKEKELA” SENIOR MANAGER: PHARMACEUTICAL SERVICES Centre: Provincial Office, Nelspruit Salary: R1 185 879 – 1 355 916 p.a. (OSD Requirements). All shortlisted candidates for SMS posts will be subjected to a technical exercise that intends to test relevant technical elements of the job. The recommended candidates will be subjected to a competency assessment. The successful candidate must sign a performance agreement. Reference No: MPDoH/July/17/01 Requirements: Diploma Pharm / BSC. Pharm / B. Pharm or NQF Level 7 qualification as recognized by SAQA. Current registration with SAPC. At least five (5) years of experience at a middle / senior managerial level. Good communication, interpersonal and computer skills (MS Word and Excel). Ability to work in a team. Good understanding of the National Drug Policy and good pharmacy practice guidelines. Sound knowledge of the Pharmacy Act and the related Substance Act. A valid code B driver’s license. Duties: Development of strategic and operational plan of Pharmaceutical services. Compile annual quarterly and monthly reports of Pharmaceutical services. Management of the pharmaceutical budget and monitor expenditure. Overall responsibility and accountability for medicine supply management processes. Manage warehousing of all pharmaceuticals. Manage the development and review of pharmaceutical policies. Manage Essential Medicine List Programme. Render technical and pharmaceutical support to all health programmes. Provide expert advice and training to other healthcare. Ensure the implementation of the down referral system. Implement the essential drug Programme. Supervise pharmaceutical care to Hospital patients by implementing monitoring of work procedures, policies and Guidelines. Overall responsibility and accountability for drug supply management to ensure the safe and reliable procurement, storage, control and distribution of quality pharmaceuticals. -

Albert Luthuli Local Municipality 2013/14
IDP REVIEW 2013/14 IIntegrated DDevelopment PPlan REVIEW - 2013/14 “The transparent, innovative and developmental local municipality that improves the quality of life of its people” Published by Chief Albert Luthuli Local Municipality Email: [email protected] Phone: (017) 843 4000 Website: www.albertluthuli.gov.za IDP REVIEW 2013/14 TABLE OF CONTENTS List of Acronyms 6 A From the desk of the Executive Mayor 7 B From the desk of the Municipal Manager 9 PART 1- INTRODUCTION AND BACKGROUND 1.1 INTRODUCTION 11 1.2 STATUS OF THE IDP 11 1.2.1 IDP Process 1.2.1.1 IDP Process Plan 1.2.1.2 Strategic Planning Session 1.3 LEGISLATIVE FRAMEWORK 12 1.4 INTER GOVERNMENTAL PLANNING 13 1.4.1 List of Policies 14 1.4.2 Mechanisms for National planning cycle 15 1.4.3 Outcomes Based Approach to Delivery 16 1.4.4 Sectoral Strategic Direction 16 1.4.4.1 Policies and legislation relevant to CALM 17 1.4.5 Provincial Growth and Development Strategy 19 1.4.6 Municipal Development Programme 19 1.5 CONCLUSION 19 PART 2- SITUATIONAL ANALYSIS 2.1 BASIC STATISTICS AND SERVICE BACKLOGS 21 2.2 REGIONAL CONTEXT 22 2.3 LOCALITY 22 2.3.1 List of wards within municipality with area names and coordinates 23 2.4 POPULATION TRENDS AND DISTRIBUTION 25 2.5 SPATIAL DEVELOPMENT 29 2.5.1 Land Use 29 2.5.2 Spatial Development Framework and Land Use Management System 29 Map: 4E: Settlement Distribution 31 Map 8: Spatial Development 32 2.5.3 Housing 33 2.5.3.1 Household Statistics 33 2.5.4 Type of dwelling per ward 34 2.5.5 Demographic Profile 34 2.6 EMPLOYMENT TRENDS 39 2.7 INSTITUTIONAL -

Table of Contents
GERT SIBANDE DISTRICT MUNICIPALITY FINAL IDP 2011/12 TO 2013/14 A DISTRICT MUNICIPALITY STRIVING TO EXCEL IN GOOD GOVERNANCE AND QUALITY INFRASTRUCTURE Gert Sibande District Municipality i Foreword by the Executive Mayor It gives me great pleasure to present the Draft Integrated Development Plan for the 2011/12 to 2013/14 Financial Years, in the last year of this Current Term of Office. In reviewing our 2010/11 IDP and subsequently drafting our IDP and Budget respectively for 2011/12 to 2013/14 and beyond, we have consulted quite extensively with our communities in all our constituent Local Municipalities through their varying groupings using our IDP Representative Forum and other IGR structures institutionalised within our Municipality. Culminating from the state of the Nation and state of the Province Addresses respectively, and aforementioned consultation and engagements with varying stakeholders the following Key Development objectives were identified as pertinent in bringing about improved quality of life for our entire populace:- Facilitate creation of more jobs and descent work; Form strategic partnerships in fighting hunger and poverty; Advocate for access to quality education for all our citizens; Ensure proper health care for all our communities; Ensure sustainable development of all rural communities within our jurisdictional area; Harness the building of safer and secure communities To date resounding success has been realised in number of areas, where many of our people are living decent lives as a result of the services provided by the District in collaboration with its social partners. Whilst much has been achieved, there is still much that needs to be done to reverse and ultimately eradicate undesired consequences of underdevelopment, inequality, unemployment, HIV/AIDS and poverty. -

Mpumalanga Presentation
STATE OF THE PROVINCE: MPUMALANGA Briefing the Portfolio Committee on Home Affairs: 8 SEPTEMBER 2015 Presented by the Acting Provincial Manager: Ms ME Makatu TABLE OF CONTENT Provincial Overview 12 - 31 Capacity Information 32 - 38 Human Resources 39 - 49 Counter Corruption, Security Services and Labour Relations 50 -54 Finance and Budget 55 - 62 Operations 63 - 74 Ports of Entry 75 - 78 Challenges and Achievement 79 - 80 2 SOCIO-ECONOMIC REVIEW AND OUTLOOK OF MPUMALANGA - DECEMBER 2014 KEY FINDINGS • Mpumalanga’s percentage share of the national population of 54.0 million was 7.8 per cent, or 4.2 million, in 2014. • In total over the last year, Mpumalanga recorded 14 000 less jobs, however, the province registered an increase of 8 000 jobs in the third quarter of 2014. • Mpumalanga (29.3 per cent), recorded the fourth highest strict unemployment rate among the nine provinces. The expanded unemployment rate was 42.0 per cent in the third quarter of 2014. • The male unemployment rate was 25.7 per cent, the female unemployment was 33.6 per cent and the youth (15-34 years) unemployment rate was 41.8 per cent. • By 2013, 10.8 per cent of the people 20 years and older had not received any schooling. • In 2013, the Mpumalanga’s Grade 12 pass rate (77.6 per cent) was the fifth highest/lowest. • In 2012, the HIV prevalence rate of the female population aged 15–49 in Mpumalanga was 35.6 per cent – the second highest after KwaZulu-Natal. • In 2013, Mpumalanga recorded a HDI (The Human development index is a composite, relative index that attempts to quantify the extent of human development of a community. -
Amazon Missions
AMAZON MISSIONS APRIL 2015 LIMPOPO & MPUMALANGA TOUR Chief Gustavo (Get us to work ) OUR TOUR COVERS THESE AREAS YOU’RE WELCOME TO INVITE US LIMPOPO: Ellisras, Soutpansberg, Valley of the Olifants, Ba-Phalaborwa, Bela-Bela, Bosbokrand, Me and Grant Duiwelskloof, Lephalale, Giyani, Hoedspruit, Waterberg, Letsitele, Leydsdorp, Louis Trichardt, Modimolle, Mogwadi, Mokopane, Potgietersrus, Nylstroom, Dendron, Giant Water Lily Leaves Messina, Naboomspruit, Mookgophong, Phalaborwa, Polokwane (Pietersburg), Seshego, Thabazimbi, Thohoyandou, Tzaneen, Vaalwater, Soutpansberg, Capricorn, Moria, Bandelierkop, Dendron, Roedtan. MPUMALANGA: Witbank, White River, Waterval Boven, Wakkerstroom, Volksrust, Vaalbank, Trichardt, Standerton, Skukuza, Makuna Mask Secunda, Sabie, Piet Retief, Ohrigstad, Komatipoort, Kaapmuiden, Hectorspruit, Hartebeeskop, Greylingstad, Amersfoort, Amsterdam, Avontuur, Asai Palm Fruit Badplaas, Balfour, Balmoral, Barberton, Belfast, Bethal, Breyten, Bushbuckridge, Carolina, Chrissiesmeer, Delmas, Dullstroom, Ermelo, Greylingstad. And everywhere in between. Please CALL, WHATSAPP or SMS us if you, your family or friends live in these areas and we’d love to arrange and address your group at your home, school, church, guesthouse, men’s -, ladies’ group etc. HOT OFF THE PRESS 2014 flowed excellently into 2015 which began with a bang! After a seasonal stretch in South America, we’re excited to share about the progress amongst the Indian Tribes. With Grant from NZ in Colombia Presently here now in April until May 2015, we’re on tour in Limpopo and Mpumalanga, sharing about reaching the unreached Indian Tribes in the Amazon jungle and supporting reached communities. Makuna Chiefs You’re welcome to invite us to share at any venue in your community or any other gathering you can think of! We do this with music, video, photo projection, props from the Amazon and testimonies of “Saved from the claws of death.” (See contact details below.) The pictures in this newsletter give you a good idea about what is happening. -
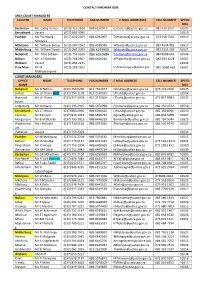
CONTACT INFORMATION AREA COURT MANAGERS CLUSTER NAME TELEPHONE FAX NUMBER E-MAIL ADDRESSES CELL NUMBER SPEED DIAL Barberton
CONTACT INFORMATION AREA COURT MANAGERS CLUSTER NAME TELEPHONE FAX NUMBER E-MAIL ADDRESSES CELL NUMBER SPEED DIAL Barberton Ms. Cathy Venter (013) 712 2104 086 6150972 [email protected] 082 334 2937 16503 Eerstehoek Vacant (017) 883 0090 16510 Evander Ms Thembela (017) 632 2204 086 6292907 [email protected] 073 158 7502 16512 Mcetywa Mdutjana Mr. William Baloyi (013) 947 2363 086 4018346 [email protected] 083 4304 485 16517 Middelburg Mr. William Nyathi (013) 262 2033 086 6293960 [email protected] 083 5355 283 16521 Nelspruit Mr. Titus Letlape (013) 753 6200 086 6292684 [email protected] 084 8388 663 16504 Nsikazi Mr. A Thabethe (013) 793 0567 086 6446010 [email protected] 082 933 3228 16527 Witbank Vacant (013) 656 2221 16534 Prov Man Mr IR (013) 283 7501 [email protected] 082 9568 663 16551 Mohlamonyane COURT MANAGERS OFFICE NAME TELEPHONE FAX NUMBER E MAIL ADDRESS CELL NUMBER SPEED NAME DIAL Nelspruit Ms N Ndlovu (013) 753 6299 013 7554077 [email protected] 076 271 2920 16525 Belfast Ms LP Thaha (Act) (013) 253 1138 013 2530035 [email protected] 16504 Waterval Ms LP Thaha (013) 257 0004 013 2570004 [email protected] 072 833 8983 16533 Boven Lydenburg Mr Chiloane (013) 235 2325 086 5070998 [email protected] 082 256 4722 16518 Eerstehoek Ms LT Mtuta (017) 883 0090 086 6046420 [email protected] 082 359 8096 16510 Carolina Mr DA Gule (017) 843 1033 086 5699732 [email protected] 082 844 5008 16507 Morgenzon Mr B Mahlambi (017) 793 3013 086 6446329 [email protected] -

Chief-Albert-Luthuli
Chief Albert Luthuli Municipality Integrated Development Plan 2020-2021 The transparent, innovative and developmental municipality that improves the quality of life of its people 6/4/2020 INDEX ACCRONYMS AND ABREVIATIONS ABET Adult Based Education and Training AIDS Acquired Immune Deficiency Syndrome ASGISA Accelerated Shared Growth Initiative South Africa CBO’s Community Based Organizations CETA Construction Education and Training Authority CHBC Community Home Base Care CIP Comprehensive Infrastructure Plan CFO Chief Financial Officer CMIP Consolidated Municipal Infrastructure Programme CM Community Services DAC District Aids Council DBSA Development Bank of South Africa DALA Department of Agriculture and Land Administration DARDLA Department of Development and Land Administration DCOGTA Department of Corporative Government and Traditional Affairs DHS Department of Human Settlements DLA Department of Land Affairs DM District Municipality DME Department of Minerals and Energy DPWR&T Department of Public Works, Roads and Transport DRDLR Department of Rural Development and Land Reform ECA Environmental Conservation Act EPWP Expanded Public Works Programme EIA Environmental Impact Assessment EIP Environmental Implementation Plan EPWP Expanded Public Works Programme EIA Environmental Impact Assessment EIP Environmental Implementation Plan EPWP Expanded Public Works Programme FBS Free basic Services FBE Free Basic Electricity GIS Geographic Information System GSDM Gert Sibande District Municipality HoD Head of Department HDI Human Development -

Mpumalanga No Fee Schools 2017
MPUMALANGA NO FEE SCHOOLS 2017 NATIONAL NAME OF SCHOOL SCHOOL PHASE ADDRESS OF SCHOOL EDUCATION DISTRICT QUINTILE LEARNER EMIS 2017 NUMBERS NUMBER 2017 800035522 ACORN - OAKS COMPREHENSIVE HIGH SCHOOL Secondary BOHLABELA 1 476 800034879 ALFRED MATSHINE COMMERCIAL SCHOOL Secondary STAND 7B CASTEEL TRUST BUSHBUCKRIDGE BOHLABELA 1 673 800030445 AMADLELO ALUHLAZA SECONDARY SCHOOL Secondary PHILA MYENI AVENUE ETHANDAKUKHANYA PIET RETIEF GERT SIBANDE 1 1386 800005058 AMALUMGELO PRIMARY SCHOOL Primary DWARS IN DIE WEG MORGENZON GERT SIBANDE 1 9 800000158 AMANZAMAHLE PRIMARY SCHOOL Primary PO BOX 1822 ERMELO ERMELO GERT SIBANDE 1 66 800000166 AMANZI PRIMARY SCHOOL Primary VYGEBOOM DAM BADPLAAS BADPLAAS GERT SIBANDE 1 104 800035381 AMON NKOSI PRIMARY SCHOOL Primary STAND NO. 6099 EXTENTION 12 BARBERTON EHLANZENI 1 727 800000240 ANDISA PRIMARY SCHOOL Primary STAND NO 3050 MABUYENI SIYABUSWA NKANGALA 1 286 800034906 ANDOVER PRIMARY SCHOOL Primary OKKERNOOTBOOM TRUST ACORNHOEK ACORNHOEK BOHLABELA 1 259 800034851 APLOS CHILOANE PRIMARY SCHOOL Primary KAZITHA TRUST ARTHURSEAT ACORNHOEK BOHLABELA 1 325 VLAKVARKFONTEIN 800000307 ARBOR PRIMARY SCHOOL Primary ARBOR DELMAS NKANGALA 1 351 FARM 800034852 ARTHURSEAT PRIMARY SCHOOL Primary ARTHURSEAT I ACORNHOEK ACORNHOEK BOHLABELA 1 236 800000406 BAADJIESBULT PRIMARY SCHOOL Combined APPELDOORN FARM CAROLINA CAROLINA GERT SIBANDE 1 184 800035179 BABATI PRIMARY SCHOOL Primary JUSTICIA TRUST JUSTICIA TRUST XIMHUNGWE BOHLABELA 1 500 800034907 BABINATAU SENIOR SECONDARY SCHOOL Secondary DINGLEDALE "B" ACORNHOEK -

Study of Knowledge, Attitudes, Perceptions and Beliefs Regarding HIV and AIDS (KAPB)
DOCUMENT RESUME ED 407 373 SP 037 287 AUTHOR Du Plessis, G. E.; And Others TITLE Study of Knowledge, Attitudes, Perceptions and Beliefs Regarding HIV and AIDS (KAPB). Memorandum Presented to the Directorate Primary Health Care of the Department of National Health and Population Development. INSTITUTION Human Sciences Research Council, Pretoria (South Africa). PUB DATE 93 NOTE 204p PUB TYPE Reports Research (143) EDRS PRICE MF01/PC09 Plus Postage. DESCRIPTORS *Acquired Immune Deficiency Syndrome; Adults; *Behavior Change; *Communicable Diseases; Elementary Secondary Education; Foreign Countries; Health Promotion; *Knowledge Level; *Public Opinion; Students; Surveys IDENTIFIERS Health Behavior; *Sexually Transmitted Diseases; *South Africa ABSTRACT This document reports on a study that assessed levels of knowledge, types of attitudes, perceptions, and beliefs (KAPB) of the general South African public regarding Human Immunodeficiency Virus (HIV) infection and Acquired Immune Deficiency Syndrome (AIDS). Interviews were conducted with 5,360 participants; survey data are summarized in 49 tables. After describing the theoretical background and methodology used in the study, findings are grouped according to differences by gender, age group, language, geographic area, educational level, population group, occupation, and differential access to sources of information about AIDS. Study results indicated: knowledge of sexually transmitted diseases (STDs) was not very high, especially regarding prevention; and many believed that contraceptives also provided protection against STDs and HIV. Overall, awareness of AIDS seemed to be high, but with a mixture of appropriate and inappropriate knowledge about HIV/AIDS in terms of transmission, nature of the disease, seriousness, prevention, and cure. Conclusions and recommendations are grouped by knowledge about HIV/AIDS, perceptions of seriousness, condom use, support for behavioral change, self-efficacy in health, perceptions of social distance, the role of communication media, and further research needs. -

Annual Performance Plan for 2013-14
f Mpumalanga Department of Health ANNUAL PERFORMANCE PLAN FOR 2013/14 Date of Tabling 09/05/2013 1 MPUMALANGA DEPARTMENT OF HEALTH ANNUAL PERFORMANCE PLAN 2013/14 1. TABLE OF CONTENTS PAGE ACRONYMS 6 1 INTRODUCTION 10 2. BACKGROUND 10 3.1 FOREWORD BY THE MEC FOR HEALTH AND SOCIAL DEVELOPMENT 11 3.2 STATEMENT BY THE HEAD OF DEPARTMENT 12 3.3 OFFICIAL SIGN OFF BY THE CHIEF FINANCIAL OFFICER, HEAD OF STATEGIC PLANNING, 14 HEAD HEALTH AND MEC FOR HEALTH AND SOCIAL DEVELOPMENT PART A 4. STRATEGIC OVERVIEW 16 4.1 VISION 4.2 MISSION 4.3 VALUES 4.4 STRATEGIC GOALS 17 4.5 SITUATION ANALYSIS 21 4.5.1 Population Profile 4.5.2 Socio-Economic Profile 4.5.3 Epidemiological Profile 4.6 PROVINCIAL SERVICE DELIVERY ENVIRONMENT 38 4.6.1 National Health Systems (NHS) Priorities for 2009-2014: The 10 Point Plan 4.6.2 Mpumalanga Department of Health Priorities 4.6.3 Mpumalanga Contribution towards Health Sector Negotiated Service Delivery Agreement (NSDA) 4.7 PROVINCIAL ORGANISATIONAL ENVIRONMENT 58 4.8 LEGISLATIVE MANDATES AND NEW POLICY INITIATIVES 59 4.9 OVERVIEW OF THE 2012/13 BUDGET AND MTEF ESTIMATES 64 4.9.1 Expenditure Estimates 4.9.2 Relating Expenditure Trends to Specific Goals 2 1. TABLE OF CONTENTS PAGE PART B – PROGRAMME AND SUB PROGRAMME PLANS 71 1. BUDGET PROGRAMME 1: ADMINISTRATION 71 1.1 Programme Purpose 1.2 Priorities 1.3 Situational Analysis and Projected Performance for Human Resources 1.4 Provincial Strategic Objectives and Targets for Administration 1.5 Quarterly Targets for Administration 1.6 Reconciling Performance Targets with Expenditure Trends and Budgets 1.7 Performance and Expenditure Trends 1.8 Risk Management 2.