Anthropometric Nutrition Survey and IYCF Study-Laghman Province
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Justice & Security Practices, Perceptions, and Problems in Kabul and Nangarhar
Justice & Security Practices, Perceptions, and Problems in Kabul and Nangarhar M AY 2014 Above: Behsud Bridge, Nangarhar Province (Photo by TLO) A TLO M A P P I N G R EPORT Justice and Security Practices, Perceptions, and Problems in Kabul and Nangarhar May 2014 In Cooperation with: © 2014, The Liaison Office. All rights reserved. No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form or by any means, electronic, recording or otherwise without prior written permission of the publisher, The Liaison Office. Permission can be obtained by emailing [email protected] ii Acknowledgements This report was commissioned from The Liaison Office (TLO) by Cordaid’s Security and Justice Business Unit. Research was conducted via cooperation between the Afghan Women’s Resource Centre (AWRC) and TLO, under the supervision and lead of the latter. Cordaid was involved in the development of the research tools and also conducted capacity building by providing trainings to the researchers on the research methodology. While TLO makes all efforts to review and verify field data prior to publication, some factual inaccuracies may still remain. TLO and AWRC are solely responsible for possible inaccuracies in the information presented. The findings, interpretations and conclusions expressed in the report are those of the authors and do not necessarily reflect the views of Cordaid. The Liaison Office (TL0) The Liaison Office (TLO) is an independent Afghan non-governmental organization established in 2003 seeking to improve local governance, stability and security through systematic and institutionalized engagement with customary structures, local communities, and civil society groups. -
Left in the Dark
LEFT IN THE DARK FAILURES OF ACCOUNTABILITY FOR CIVILIAN CASUALTIES CAUSED BY INTERNATIONAL MILITARY OPERATIONS IN AFGHANISTAN Amnesty International is a global movement of more than 3 million supporters, members and activists in more than 150 countries and territories who campaign to end grave abuses of human rights. Our vision is for every person to enjoy all the rights enshrined in the Universal Declaration of Human Rights and other international human rights standards. We are independent of any government, political ideology, economic interest or religion and are funded mainly by our membership and public donations. First published in 2014 by Amnesty International Ltd Peter Benenson House 1 Easton Street London WC1X 0DW United Kingdom © Amnesty International 2014 Index: ASA 11/006/2014 Original language: English Printed by Amnesty International, International Secretariat, United Kingdom All rights reserved. This publication is copyright, but may be reproduced by any method without fee for advocacy, campaigning and teaching purposes, but not for resale. The copyright holders request that all such use be registered with them for impact assessment purposes. For copying in any other circumstances, or for reuse in other publications, or for translation or adaptation, prior written permission must be obtained from the publishers, and a fee may be payable. To request permission, or for any other inquiries, please contact [email protected] Cover photo: Bodies of women who were killed in a September 2012 US airstrike are brought to a hospital in the Alingar district of Laghman province. © ASSOCIATED PRESS/Khalid Khan amnesty.org CONTENTS MAP OF AFGHANISTAN .......................................................................................... 6 1. SUMMARY ......................................................................................................... 7 Methodology .......................................................................................................... -
THE ANSO REPORT -Not for Copy Or Sale
The Afghanistan NGO Safety Office Issue: 72 16-30 April 2011 ANSO and our donors accept no liability for the results of any activity conducted or omitted on the basis of this report. THE ANSO REPORT -Not for copy or sale- Inside this Issue COUNTRY SUMMARY Central Region 2 The IEA announced the ini- salary lines, banks, demon- A second, equally lethal 5 Northern Region tiation of their ‘Spring Offen- stration, arbakai shura and effective trend that has Western Region 10 sive’ on April 29th, an event meetings and shops but we developed in line with the that occurs an a yearly basis will need to monitor the previous, is the surgical Eastern Region 14 and is generally intended as a target pattern closely to targeting of key leadership Southern Region 20 strategic statement regarding fully understand this scope (military, political, and ci- their goals, methodology, as of this term. When taken in vilian) with suicide attacks. 27 ANSO Info Page well as guidance to their lead- conjunction with the in- Of note, this trend, when ership though is also an ele- struction to deliver coupled with the above, ment of their wider infor- “meticulous military plans” proves to be particular dif- YOU NEED TO KNOW mation operations plan. The however we would stop ficult to mitigate for the operation, known as ‘Badar’, short of seeing it as carte target groups, as seen in • IEA announces spring offen- while short on tactical details, blanche to attack any place the penetration of the sive, Operation Badar contains a few comments of that targets recreate or gath- MoD this period in Kabul. -
Daily Situation Report 31 October 2010 Safety and Security Issues Relevant to Sssi Personnel and Clients
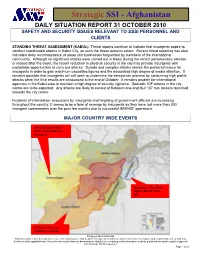
Strategic SSI - Afghanistan DAILY SITUATION REPORT 31 OCTOBER 2010 SAFETY AND SECURITY ISSUES RELEVANT TO SSSI PERSONNEL AND CLIENTS STANDING THREAT ASSESSMENT (KABUL): Threat reports continue to indicate that insurgents aspire to conduct coordinated attacks in Kabul City, as such the threat remains extant. Recent threat reporting has also indicated likely reconnaissance of areas and businesses frequented by members of the international community. Although no significant attacks were carried out in Kabul during the recent parliamentary election, or indeed after the event, the recent reduction in physical security in the city may provide insurgents with exploitable opportunities to carry out attacks. Suicide and complex attacks remain the preferred choice for insurgents in order to gain maximum casualties figures and the associated high degree of media attention. It remains possible that insurgents will still seek to undermine the democratic process by conducting high profile attacks when the final results are announced at the end of October. It remains prudent for international agencies in the Kabul area to maintain a high degree of security vigilance. Sporadic IDF attacks in the city centre are to be expected. Any attacks are likely to consist of between one and four 107 mm rockets launched towards the city centre. Incidents of intimidation, executions by insurgents and targeting of government officials are increasing throughout the country. It seems to be a form of revenge by insurgents as they have lost more than 300 insurgent commanders over the past few months due to successful IM/ANSF operations. MAJOR COUNTRY WIDE EVENTS Herat: Influencial local Tribal Leader killed by insurgents Nangarhar: Five attacks against Border Police OPs Helmand: Five local residents murdered Privileged and Confidential This information is intended only for the use of the individual or entity to which it is addressed and may contain information that is privileged, confidential, and exempt from disclosure under applicable law. -

PDMC Laghman Meeting Minutes
Laghman Provincial Disaster Management Committee (PDMC) Meeting Minutes Provincial Governor’s Office – Wednesday, 04 March, 2015 Participants: WFP, UNICEF, WHO, NCRO, SERVE, IRC, NRC, MADERA, SCA, IOM, DRC, ARCS, OCHA, ANDMA, ANA, ANP, DRRD, DoPH, DoRR, DoEnvironment, DoEducation, DoPW, DoAIL, Governor’s Office and other government officials. A. Introduction and Opening Remarks of Provincial Governor: On Wednesday 04 October 15, the Provincial Governor (PG) for Laghman called a Provincial Disaster Management Committee meeting (PDMC). After a short round of introductions, the PG welcomed PDMC members, further he extend of condolences with families, lost their family members due to recent rainfall, snowfall/avalanches and flood particularly to the people of Laghman province and he also highlighted on recent natural hazards (Rainfall, Flood and Snowfall) occurred on 25 February, 2015. The PG gratitude from humanitarian community’s efforts for there on timely response to the affected families he also appreciated the ANSAF’s on time action in rescued the people in Mehterlam and Qarghayi districts of Laghman province, especially ANA rescued 90 Nomad people Marooned in Qarghayi district of Laghman. The PG also highlighted on devastation caused by rainfall and flood which lifted 5 killed, 13 injured, about more than 500 families affected, 800 Jirebs or 400 Acores Agriculture land/Crops washed away and about 39 irrigation canal and intakes severely damaged or destroyed. The PG calcified devastations in three categories to facilitate the response for both (Humanitarian Community and Government line departments). 1. Response to Emergency need and saves lives. 2. Mid-terms actions as reactivation of irrigation system (cleaning of intakes and irrigation canal) opening the routs. -

Men, Masculinities, Conflict and Peacebuilding in Afghanistan
Navigating norms and insecurity: Men, masculinities, conflict and peacebuilding in Afghanistan WORKING PAPER | NOVEMBER 2018 Henri Myrttinen European Union initiative CONTENTS ACKNOWLEDGEMENTS ........................................................................................................................... 1 INTRODUCTION ....................................................................................................................................... 2 GENDER, CONFLICT AND PEACEBUILDING .............................................................................................. 3 Why masculinities? ............................................................................................................................. 4 BACKGROUND ......................................................................................................................................... 5 Project background ............................................................................................................................. 5 Women, peace and security in Afghanistan ....................................................................................... 6 Background to the target provinces ................................................................................................... 7 RESEARCH FINDINGS ............................................................................................................................. 11 Gender norms .................................................................................................................................. -

19 October 2020 "Generated on Refers to the Date on Which the User Accessed the List and Not the Last Date of Substantive Update to the List
Res. 1988 (2011) List The List established and maintained pursuant to Security Council res. 1988 (2011) Generated on: 19 October 2020 "Generated on refers to the date on which the user accessed the list and not the last date of substantive update to the list. Information on the substantive list updates are provided on the Council / Committee’s website." Composition of the List The list consists of the two sections specified below: A. Individuals B. Entities and other groups Information about de-listing may be found at: https://www.un.org/securitycouncil/ombudsperson (for res. 1267) https://www.un.org/securitycouncil/sanctions/delisting (for other Committees) https://www.un.org/securitycouncil/content/2231/list (for res. 2231) A. Individuals TAi.155 Name: 1: ABDUL AZIZ 2: ABBASIN 3: na 4: na ﻋﺒﺪ اﻟﻌﺰﻳﺰ ﻋﺒﺎﺳﯿﻦ :(Name (original script Title: na Designation: na DOB: 1969 POB: Sheykhan Village, Pirkowti Area, Orgun District, Paktika Province, Afghanistan Good quality a.k.a.: Abdul Aziz Mahsud Low quality a.k.a.: na Nationality: na Passport no: na National identification no: na Address: na Listed on: 4 Oct. 2011 (amended on 22 Apr. 2013) Other information: Key commander in the Haqqani Network (TAe.012) under Sirajuddin Jallaloudine Haqqani (TAi.144). Taliban Shadow Governor for Orgun District, Paktika Province as of early 2010. Operated a training camp for non- Afghan fighters in Paktika Province. Has been involved in the transport of weapons to Afghanistan. INTERPOL- UN Security Council Special Notice web link: https://www.interpol.int/en/How-we-work/Notices/View-UN-Notices- Individuals click here TAi.121 Name: 1: AZIZIRAHMAN 2: ABDUL AHAD 3: na 4: na ﻋﺰﯾﺰ اﻟﺮﺣﻤﺎن ﻋﺒﺪ اﻻﺣﺪ :(Name (original script Title: Mr Designation: Third Secretary, Taliban Embassy, Abu Dhabi, United Arab Emirates DOB: 1972 POB: Shega District, Kandahar Province, Afghanistan Good quality a.k.a.: na Low quality a.k.a.: na Nationality: Afghanistan Passport no: na National identification no: Afghan national identification card (tazkira) number 44323 na Address: na Listed on: 25 Jan. -
An Annotated Bibliography of Nuristan (Kafiristan) and the Kalash Kafirs of Chitral Part One
Historisk-filosofiske Meddelelser udgivet af Det Kongelige Danske Videnskabernes Selskab Bind 41, nr. 3 Hist. Filos. Medd. Dan. Vid. Selsk. 41, no. 3 (1966) AN ANNOTATED BIBLIOGRAPHY OF NURISTAN (KAFIRISTAN) AND THE KALASH KAFIRS OF CHITRAL PART ONE SCHUYLER JONES With a Map by Lennart Edelberg København 1966 Kommissionær: Munksgaard X Det Kongelige Danske Videnskabernes Selskab udgiver følgende publikationsrækker: The Royal Danish Academy of Sciences and Letters issues the following series of publications: Bibliographical Abbreviation. Oversigt over Selskabets Virksomhed (8°) Overs. Dan. Vid. Selsk. (Annual in Danish) Historisk-filosofiske Meddelelser (8°) Hist. Filos. Medd. Dan. Vid. Selsk. Historisk-filosofiske Skrifter (4°) Hist. Filos. Skr. Dan. Vid. Selsk. (History, Philology, Philosophy, Archeology, Art History) Matematisk-fysiske Meddelelser (8°) Mat. Fys. Medd. Dan. Vid. Selsk. Matematisk-fysiske Skrifter (4°) Mat. Fys. Skr. Dan. Vid. Selsk. (Mathematics, Physics, Chemistry, Astronomy, Geology) Biologiske Meddelelser (8°) Biol. Medd. Dan. Vid. Selsk. Biologiske Skrifter (4°) Biol. Skr. Dan. Vid. Selsk. (Botany, Zoology, General Biology) Selskabets sekretariat og postadresse: Dantes Plads 5, København V. The address of the secretariate of the Academy is: Det Kongelige Danske Videnskabernes Selskab, Dantes Plads 5, Köbenhavn V, Denmark. Selskabets kommissionær: Munksgaard’s Forlag, Prags Boulevard 47, København S. The publications are sold by the agent of the Academy: Munksgaard, Publishers, 47 Prags Boulevard, Köbenhavn S, Denmark. HISTORI SK-FILOSO FISKE MEDDELELSER UDGIVET AF DET KGL. DANSKE VIDENSKABERNES SELSKAB BIND 41 KØBENHAVN KOMMISSIONÆR: MUNKSGAARD 1965—66 INDHOLD Side 1. H jelholt, H olger: British Mediation in the Danish-German Conflict 1848-1850. Part One. From the MarCh Revolution to the November Government. -

Strategic SSI - Afghanistan
Strategic SSI - Afghanistan DAILY SITUATION REPORT 20 MARCH 2010 MAJOR COUNTRY WIDE EVENTS Insurgents intend to conduct numerous attacks in the Jalalabad Region over the next 5 days SECURITY THREATS RELEVANT TO SSSI PERSONNEL AND CLIENTS UNCLASSIFIED THREAT WARNINGS NATIONWIDE: • Information at hand indicates that insurgents intend to conduct numerous attacks in the Jalalabad Region over the next 5 days. It is believed that these attacks may include suicide IEDs, rocket attacks and ambushes on Jalalabad City, Jalalabad Airfield and Government Offices. These attacks are intended to occur in the same time frame as the New Year celebrations on Sunday 22nd March. It is reported that the Insurgents and Islamic parties are warning people of Jalalabad not to participate in the New Year celebrations. • Insurgent capability and intent to carry out attacks in Kabul City remain elevated. Threat reporting continues to be received with regard to insurgent planning to conduct attacks in the city. BOLO: White corolla, reportedly 5 pax, vehicle registration #45344. • Kabul: Imminent threat of SVBIED on the road from Green Village to KIA (route BOTTLE). Privileged and Confidential 1 This information is intended only for the use of the individual or entity to which it is addressed and may contain information that is privileged, confidential and exempt from disclosure under applicable law. You are hereby notified that any dissemination, distribution, or copying of this information is strictly prohibited without the explicit approval from StrategicSSI Management. Strategic SSI - Afghanistan BREAKDOWN OF INCIDENTS REPORTED FOR AFGHANISTAN IN SSSI DSR FOR PERIOD 19 MAR – 20 MAR 2010 Incidents for report period Murder, 0 Crime, 2 Arson, 1 IDF Attack, 2 Insurgency, 4 Ambush, 3 Kidnap, 3 Attack, 6 Miscellaneous, Expl device, 4 1 Successes, 12 Table illustrating the number of Killed and Wounded, Captured and Arrested as per the reporting’s of the SSSI DSR. -

Eric Newby Worked Briefly in Advertising Before Joininga Finnish Four-Masted Bark in 1938, an Experience He Described in the Last Grain Race
PENGUIN BOOKS A SHORT WALK IN THE HINDU RUSH Born in London in 1919 and educated at St. Paul's School, Eric Newby worked briefly in advertising before joininga Finnish four-masted bark in 1938, an experience he described in The Last Grain Race. In 1942 he was captured off Sicily while trying to rejoin the submarine from which he had landed to attack a German airfield. When the Snow Comes, They Will Take You Away describes how he escaped with the aid of the woman he subsequently married. For nine years or so he worked in the wholesale fashion business, "tottering up the back stairs of stores with armfuls of stock" (of which he wrote in Something Wholesale), and in a Mayfair couture house. Then he left to explore wildest Nuristan, an expedition hilariously chronicled in A Short Walk in the Hindu Kush. In 1963—after some years as fashion buyer to a chai n of department stores-—together with his wife, Wanda, he made a 1,200-mile descent of the Ganges, described in Slowly down the Ganges. On his return he became travel editor of the Observer. Other books by Eric Newby include Love and War in the Apennines, The World Atlas of Exploration, and Great Ascents. His most recent book, The Big Red Train Ride, an account of his journey from Moscow to the Pacific on the Trans-Siberian Railway, is also published by Penguin Books. He and his wife now live in Devonshire when not traveling abroad. ERIC NEWBY A Short Walk in the Hindu Kush Preface by Evelyn Waugh PENGUIN BOOKS Penguin Books Ltd, Harmondsworth, Middlesex, England Penguin Books, 625 Madison Avenue, New York, New York 10022, U.S.A. -

Lead Inspector General for Operation Freedom's Sentinel April 1, 2021
OFS REPORT TO CONGRESS FRONT MATTER OPERATION FREEDOM’S SENTINEL LEAD INSPECTOR GENERAL REPORT TO THE UNITED STATES CONGRESS APRIL 1, 2021–JUNE 30, 2021 FRONT MATTER ABOUT THIS REPORT A 2013 amendment to the Inspector General Act established the Lead Inspector General (Lead IG) framework for oversight of overseas contingency operations and requires that the Lead IG submit quarterly reports to Congress on each active operation. The Chair of the Council of Inspectors General for Integrity and Efficiency designated the DoD Inspector General (IG) as the Lead IG for Operation Freedom’s Sentinel (OFS). The DoS IG is the Associate IG for the operation. The USAID IG participates in oversight of the operation. The Offices of Inspector General (OIG) of the DoD, the DoS, and USAID are referred to in this report as the Lead IG agencies. Other partner agencies also contribute to oversight of OFS. The Lead IG agencies collectively carry out the Lead IG statutory responsibilities to: • Develop a joint strategic plan to conduct comprehensive oversight of the operation. • Ensure independent and effective oversight of programs and operations of the U.S. Government in support of the operation through either joint or individual audits, inspections, investigations, and evaluations. • Report quarterly to Congress and the public on the operation and activities of the Lead IG agencies. METHODOLOGY To produce this quarterly report, the Lead IG agencies submit requests for information to the DoD, the DoS, USAID, and other Federal agencies about OFS and related programs. The Lead IG agencies also gather data and information from other sources, including official documents, congressional testimony, policy research organizations, press conferences, think tanks, and media reports. -

Selected Papers Hindukush Cultural Conference Moesgard 1970
BEITRAGE ZUR SODASIENFORSCHUNG SODASIEN - INSTITUT UNIVERSITAT HEIDELBERG BAND 1 FRANZ STEINER VERLAG . WIESBADEN 1974 ISBN 3-515-01217-6 Alle Rechte vorbehalten Ohne ausdriickliche Genehmigung des Verlages ist es auch nicht gestattet, das Werk oder einzelne Teile daraus nachzudrucken oder auf photomechanischem Wege (Photoko~ie,Mikrokopie usw.) zu ~ervielfalti~en @ 19 74 by Franz Steiner Verlag GmbH, Wiesbaden Satz und Druck: Druckerei Wolf, Heppenheim Printed in Germany This photo may symbolize the Conferenee: From right to left Professor Georg Morgenstierne, Oslo, President of the Conferenee, Ahmad Ali Motamedi, Director General of the Antiquitie~ of Afghbt~I- stan, Ahmad Yusuf Nuristani fro~~NisheigFom,student of the Umiversi- ty of Kabul, ~ittfngmound a the elentss o2€ 9 reaaam4mzok- iom af r WaFg~aliiArmem im %he pa Mws,vlse; (Pkmh~P~sban '&3.re$rug ram 9, CONTENTS Page INTRODUCTION (K.Jettmar) .................................... IX I. LINGUISTIC INTRODUCTION G.Morgenstierne: Languages of Nuristan and Surrounding Regions ...................................... 1 11. CONTRIBUTIONS TO THE HISTORY OF NURISTAN K.Kristiansen: A Kafir on KAfir History and Festivals .................................... 11 R.F.Strand: Native Accounts of Kom History ............ 22 Wazir Ali Shah: Invasions Preceding the Conquest of Nuristan ..................................... 24 111. CONTRIBUTIONS TO THE PROBLEM OF THE PRE-MUSLIM RELIGION OF NURISTAN Shahzada Hussam-ul-Mulk: The Cosmology of the Red Kafirs ....................................... 26 G.Buddruss: Some Reflections on a Kafir Myth .......... 31 W.Lentz: Western Parallels to the Deeds of Imra ....... 37 K.Jettmar: Iranian Influence on the Cultures of the Hindukush .................................... 39 IV. CONTRIBUTIONS TO A SOCIOLOGY OF NURISTAN S.Jones: Kalashum Political Organisation .............. 44 R.F.Strand: Principles of Kinship Organisation among the Kom Nuristani ...............................