Identification of Protective Immune Responses and the Immunomodulatory Capacity of Litomosoides Sigmodontis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Functional Parasitic Worm Secretome: Mapping the Place of Onchocerca Volvulus Excretory Secretory Products
pathogens Review The Functional Parasitic Worm Secretome: Mapping the Place of Onchocerca volvulus Excretory Secretory Products Luc Vanhamme 1,*, Jacob Souopgui 1 , Stephen Ghogomu 2 and Ferdinand Ngale Njume 1,2 1 Department of Molecular Biology, Institute of Biology and Molecular Medicine, IBMM, Université Libre de Bruxelles, Rue des Professeurs Jeener et Brachet 12, 6041 Gosselies, Belgium; [email protected] (J.S.); [email protected] (F.N.N.) 2 Molecular and Cell Biology Laboratory, Biotechnology Unit, University of Buea, Buea P.O Box 63, Cameroon; [email protected] * Correspondence: [email protected] Received: 28 October 2020; Accepted: 18 November 2020; Published: 23 November 2020 Abstract: Nematodes constitute a very successful phylum, especially in terms of parasitism. Inside their mammalian hosts, parasitic nematodes mainly dwell in the digestive tract (geohelminths) or in the vascular system (filariae). One of their main characteristics is their long sojourn inside the body where they are accessible to the immune system. Several strategies are used by parasites in order to counteract the immune attacks. One of them is the expression of molecules interfering with the function of the immune system. Excretory-secretory products (ESPs) pertain to this category. This is, however, not their only biological function, as they seem also involved in other mechanisms such as pathogenicity or parasitic cycle (molting, for example). Wewill mainly focus on filariae ESPs with an emphasis on data available regarding Onchocerca volvulus, but we will also refer to a few relevant/illustrative examples related to other worm categories when necessary (geohelminth nematodes, trematodes or cestodes). -

Baylisascariasis
Baylisascariasis Importance Baylisascaris procyonis, an intestinal nematode of raccoons, can cause severe neurological and ocular signs when its larvae migrate in humans, other mammals and birds. Although clinical cases seem to be rare in people, most reported cases have been Last Updated: December 2013 serious and difficult to treat. Severe disease has also been reported in other mammals and birds. Other species of Baylisascaris, particularly B. melis of European badgers and B. columnaris of skunks, can also cause neural and ocular larva migrans in animals, and are potential human pathogens. Etiology Baylisascariasis is caused by intestinal nematodes (family Ascarididae) in the genus Baylisascaris. The three most pathogenic species are Baylisascaris procyonis, B. melis and B. columnaris. The larvae of these three species can cause extensive damage in intermediate/paratenic hosts: they migrate extensively, continue to grow considerably within these hosts, and sometimes invade the CNS or the eye. Their larvae are very similar in appearance, which can make it very difficult to identify the causative agent in some clinical cases. Other species of Baylisascaris including B. transfuga, B. devos, B. schroeder and B. tasmaniensis may also cause larva migrans. In general, the latter organisms are smaller and tend to invade the muscles, intestines and mesentery; however, B. transfuga has been shown to cause ocular and neural larva migrans in some animals. Species Affected Raccoons (Procyon lotor) are usually the definitive hosts for B. procyonis. Other species known to serve as definitive hosts include dogs (which can be both definitive and intermediate hosts) and kinkajous. Coatimundis and ringtails, which are closely related to kinkajous, might also be able to harbor B. -

Strongyloides Myopotami (Secernentea: Strongyloididae) from the Intestine of Feral Nutrias (Myocastor Coypus) in Korea
ISSN (Print) 0023-4001 ISSN (Online) 1738-0006 Korean J Parasitol Vol. 52, No. 5: 531-535, October 2014 ▣ CASE REPORT http://dx.doi.org/10.3347/kjp.2014.52.5.531 Strongyloides myopotami (Secernentea: Strongyloididae) from the Intestine of Feral Nutrias (Myocastor coypus) in Korea Seongjun Choe, Dongmin Lee, Hansol Park, Mihyeon Oh, Hyeong-Kyu Jeon, Keeseon S. Eom* Department of Parasitology, Medical Research Institute and Parasite Resource Bank, Chungbuk National University School of Medicine, Cheongju 361-763, Korea Abstract: Surveys on helminthic fauna of the nutria, Myocastor coypus, have seldom been performed in the Republic of Korea. In the present study, we describe Strongyloides myopotami (Secernentea: Strongyloididae) recovered from the small intestine of feral nutrias. Total 10 adult nutrias were captured in a wetland area in Gimhae-si (City), Gyeongsangnam- do (Province) in April 2013. They were transported to our laboratory, euthanized with ether, and necropsied. About 1,300 nematode specimens were recovered from 10 nutrias, and some of them were morphologically observed by light and scanning electron microscopies. They were 3.7-4.7 (4.0± 0.36) mm in length, 0.03-0.04 (0.033) mm in width. The worm dimension and other morphological characters, including prominent lips of the vulva, blunted conical tail, straight type of the ovary, and 8-chambered stoma, were all consistent with S. myopotami. This nematode fauna is reported for the first time in Korea. Key words: Strongyloides myopotami, nutria, Myocastor coypus The nutria (Myocastor coypus) or coypu rat is a large rodent notic diseases caused by viruses, bacteria, and parasites [1]. -
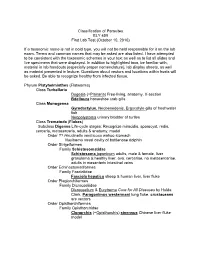
Classification of Parasites BLY 459 First Lab Test (October 10, 2010)
Classification of Parasites BLY 459 First Lab Test (October 10, 2010) If a taxonomic name is not in bold type, you will not be held responsible for it on the lab exam. Terms and common names that may be asked are also listed. I have attempted to be consistent with the taxonomic schemes in your text as well as to list all slides and live specimens that were displayed. In addition to highlighted taxa, be familiar with, material in lab handouts (especially proper nomenclature), lab display sheets, as well as material presented in lecture. Questions about vectors and locations within hosts will be asked. Be able to recognize healthy from infected tissue. Phylum Platyhelminthes (Flatworms) Class Turbellaria Dugesia (=Planaria ) Free-living, anatomy, X-section Bdelloura horseshoe crab gills Class Monogenea Gyrodactylus , Neobenedenis, Ergocotyle gills of freshwater fish Neopolystoma urinary bladder of turtles Class Trematoda ( Flukes ) Subclass Digenea Life-cycle stages: Recognize miracidia, sporocyst, redia, cercaria , metacercaria, adults & anatomy, model Order ?? Hirudinella ventricosa wahoo stomach Nasitrema nasal cavity of bottlenose dolphin Order Strigeiformes Family Schistosomatidae Schistosoma japonicum adults, male & female, liver granuloma & healthy liver, ova, cercariae, no metacercariae, adults in mesenteric intestinal veins Order Echinostomatiformes Family Fasciolidae Fasciola hepatica sheep & human liver, liver fluke Order Plagiorchiformes Family Dicrocoeliidae Dicrocoelium & Eurytrema Cure for All Diseases by Hulda Clark, Paragonimus -

Angiostrongylus Cantonensis in Recife, Pernambuco, Brazil
Letter Arq Neuropsiquiatr 2009;67(4):1093-1096 AlicAtA DiSEASE Neuroinfestation by Angiostrongylus cantonensis in Recife, Pernambuco, Brazil Ana Rosa Melo Correa Lima1, Solange Dornelas Mesquita2, Silvana Sobreira Santos1, Eduardo Raniere Pessoa de Aquino1, Luana da Rocha Samico Rosa3, Fábio Souza Duarte3, Alessandra Oliveira Teixeira1, Zenize Rocha da Silva Costa4, Maria Lúcia Brito Ferreira5 Angiostrongylus cantonensis, is a nematode in the panying the patient reported that she had presented a rash as- Secernentea class, Strongylidae order, Metastrongylidæ sociated with joint pain, followed by progressive difficulty in superfamily and Angiostrongylidæ family1, and is the walking for 30 days, which was associated with sleepiness over most common cause of human eosinophilic meningi- the last 15 days. tis worldwide. This parasite has rats and other mammals In the patient’s past history, there were references to mental as definitive hosts and snails, freshwater shrimp, fish, retardation and lack of ability to understanding simple orders. frogs and monitor lizards as intermediate hosts1. Mam- She presented independent gait and had frequently run away mals are infected by ingestion of intermediate hosts from home into the surrounding area. There was mention of in- and raw/undercooked snails or vegetables, contain- voluntary movements, predominantly of the upper limbs, which ing third-stage larvae2. Once infested, the larvae pen- intensified after the change of health status that motivated the etrate the vasculature of the intestinal tract and pro- current search for medical assistance. In November 2007, the pa- mote an inflammatory reaction with eosinophilia and tient presented with generalized tonic-clonic seizures and was lymphocytosis. This produces rupture of the blood- medicated with carbamazepine, 200 mg/twice a day. -

Worms, Nematoda
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Faculty Publications from the Harold W. Manter Laboratory of Parasitology Parasitology, Harold W. Manter Laboratory of 2001 Worms, Nematoda Scott Lyell Gardner University of Nebraska - Lincoln, [email protected] Follow this and additional works at: https://digitalcommons.unl.edu/parasitologyfacpubs Part of the Parasitology Commons Gardner, Scott Lyell, "Worms, Nematoda" (2001). Faculty Publications from the Harold W. Manter Laboratory of Parasitology. 78. https://digitalcommons.unl.edu/parasitologyfacpubs/78 This Article is brought to you for free and open access by the Parasitology, Harold W. Manter Laboratory of at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in Faculty Publications from the Harold W. Manter Laboratory of Parasitology by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. Published in Encyclopedia of Biodiversity, Volume 5 (2001): 843-862. Copyright 2001, Academic Press. Used by permission. Worms, Nematoda Scott L. Gardner University of Nebraska, Lincoln I. What Is a Nematode? Diversity in Morphology pods (see epidermis), and various other inverte- II. The Ubiquitous Nature of Nematodes brates. III. Diversity of Habitats and Distribution stichosome A longitudinal series of cells (sticho- IV. How Do Nematodes Affect the Biosphere? cytes) that form the anterior esophageal glands Tri- V. How Many Species of Nemata? churis. VI. Molecular Diversity in the Nemata VII. Relationships to Other Animal Groups stoma The buccal cavity, just posterior to the oval VIII. Future Knowledge of Nematodes opening or mouth; usually includes the anterior end of the esophagus (pharynx). GLOSSARY pseudocoelom A body cavity not lined with a me- anhydrobiosis A state of dormancy in various in- sodermal epithelium. -

Fibre Couplings in the Placenta of Sperm Whales, Grows to A
news and views Most (but not all) nematodes are small Daedalus and nondescript. For example, Placento- T STUDIOS nema gigantissima, which lives as a parasite Fibre couplings in the placenta of sperm whales, grows to a CS./HOL length of 8 m, with a diameter of 2.5 cm. The The nail, says Daedalus, is a brilliant and free-living, marine Draconema has elongate versatile fastener, but with a fundamental O ASSO T adhesive organs on the head and along the contradiction. While being hammered in, HO tail, and moves like a caterpillar. But the gen- it is a strut, loaded in compression. It must BIOP eral uniformity of most nematode species be thick enough to resist buckling. Yet has hampered the establishment of a classifi- once in place it is a tie, loaded in tension, 8 cation that includes both free-living and par- and should be thin and flexible to bear its asitic species. Two classes have been recog- load efficiently. He is now resolving this nized (the Secernentea and Adenophorea), contradiction. based on the presence or absence of a caudal An ideal nail, he says, should be driven sense organ, respectively. But Blaxter et al.1 Figure 2 The bad — eelworm (root knot in by a force applied, not to its head, but to have concluded from the DNA sequences nematode), which forms characteristic nodules its point. Its shaft would then be drawn in that the Secernentea is a natural group within on the roots of sugar beet and rice. under tension; it could not buckle, and the Adenophorea. -

Subclase Secernentea
Orden Ascaridida T. 21. ASCARIDIDOS. Generalidades y Clasificación. Incluye parásitos con tres labios de gran tamaño. En los machos, cuando existen alas caudales, éstas se localizan Ascaridioideos y Anisakoideos. lateralmente. 1. GENERALIDADES Y CLASIFICACIÓN Los ascarídidos son nematodos con fasmidios (quimiorreceptores posteriores); pertenecen por tanto a la Clase Secernentea. Los machos presentan generalmente alas caudales o bolsas copuladoras. Los ascarídidos de interés veterinario se clasifican en base al siguiente esquema taxonómico: Orden Ascaridida Superfamilia Ascaridoidea Familia Ascarididae Género Ascaris Género Parascaris Género Toxocara Género Toxascaris Fig. 1. Extremo caudal del macho en Ascarididae. Superfamilia Anisakoidea Familia Anisakidae Género Anisakis Superfamilia Ascaridoidea Género Contracaecum Género Phocanema Por lo general son nematodos de gran tamaño. No Género Pseudoterranova presentan cápsula bucal y el esófago carece de bulbo posterior Superfamilia Heterakoidea pronunciado. En algunas especies el esófago está seguido de un Familia Heterakidae: G. Heterakis ventrículo posterior corto que puede derivarse en un apéndice Familia Ascaridiidae: G. Ascaridia 1 ventricular, mientras que otras presentan una prolongación del 2.1. GÉNERO ASCARIS intestino en sentido craneal que se conoce como ciego intestinal (Fig. 12, Familia Anisakidae). Existen dos espículas en los machos Ascaris suum y el ciclo de vida puede ser directo o indirecto. Es un parásito del cerdo con distribución cosmopolita y de 2. FAMILIA ASCARIDIDAE considerable importancia económica. Sin embargo, su prevalencia está disminuyendo debido a los cada vez más frecuentes sistemas Los labios, que como característica del Orden están bien de producción intensiva y a la instauración de tratamientos desarrollados, presentan una serie de papilas labiales externas e antihelmínticos periódicos. Durante años se ha considerado internas, así como un borde denticular en su cara interna. -
Monophyly of Clade III Nematodes Is Not Supported by Phylogenetic Analysis of Complete Mitochondrial Genome Sequences
UC Davis UC Davis Previously Published Works Title Monophyly of clade III nematodes is not supported by phylogenetic analysis of complete mitochondrial genome sequences Permalink https://escholarship.org/uc/item/7509r5vp Journal BMC Genomics, 12(1) ISSN 1471-2164 Authors Park, Joong-Ki Sultana, Tahera Lee, Sang-Hwa et al. Publication Date 2011-08-03 DOI http://dx.doi.org/10.1186/1471-2164-12-392 Peer reviewed eScholarship.org Powered by the California Digital Library University of California Park et al. BMC Genomics 2011, 12:392 http://www.biomedcentral.com/1471-2164/12/392 RESEARCHARTICLE Open Access Monophyly of clade III nematodes is not supported by phylogenetic analysis of complete mitochondrial genome sequences Joong-Ki Park1*, Tahera Sultana2, Sang-Hwa Lee3, Seokha Kang4, Hyong Kyu Kim5, Gi-Sik Min2, Keeseon S Eom6 and Steven A Nadler7 Abstract Background: The orders Ascaridida, Oxyurida, and Spirurida represent major components of zooparasitic nematode diversity, including many species of veterinary and medical importance. Phylum-wide nematode phylogenetic hypotheses have mainly been based on nuclear rDNA sequences, but more recently complete mitochondrial (mtDNA) gene sequences have provided another source of molecular information to evaluate relationships. Although there is much agreement between nuclear rDNA and mtDNA phylogenies, relationships among certain major clades are different. In this study we report that mtDNA sequences do not support the monophyly of Ascaridida, Oxyurida and Spirurida (clade III) in contrast to results for nuclear rDNA. Results from mtDNA genomes show promise as an additional independently evolving genome for developing phylogenetic hypotheses for nematodes, although substantially increased taxon sampling is needed for enhanced comparative value with nuclear rDNA. -

Review of the Genus Mansonella Faust, 1929 Sensu Lato (Nematoda: Onchocercidae), with Descriptions of a New Subgenus and a New Subspecies
Zootaxa 3918 (2): 151–193 ISSN 1175-5326 (print edition) www.mapress.com/zootaxa/ Article ZOOTAXA Copyright © 2015 Magnolia Press ISSN 1175-5334 (online edition) http://dx.doi.org/10.11646/zootaxa.3918.2.1 http://zoobank.org/urn:lsid:zoobank.org:pub:DE65407C-A09E-43E2-8734-F5F5BED82C88 Review of the genus Mansonella Faust, 1929 sensu lato (Nematoda: Onchocercidae), with descriptions of a new subgenus and a new subspecies ODILE BAIN1†, YASEN MUTAFCHIEV2, KERSTIN JUNKER3,8, RICARDO GUERRERO4, CORALIE MARTIN5, EMILIE LEFOULON5 & SHIGEHIKO UNI6,7 1Muséum National d'Histoire Naturelle, Parasitologie comparée, UMR 7205 CNRS, CP52, 61 rue Buffon, 75231 Paris Cedex 05, France 2Institute of Biodiversity and Ecosystem Research, Bulgarian Academy of Sciences, 2 Gagarin Street, 1113 Sofia, Bulgaria E-mail: [email protected] 3ARC-Onderstepoort Veterinary Institute, Private Bag X05, Onderstepoort, 0110, South Africa 4Instituto de Zoología Tropical, Faculdad de Ciencias, Universidad Central de Venezuela, PO Box 47058, 1041A, Caracas, Venezuela. E-mail: [email protected] 5Muséum National d'Histoire Naturelle, Parasitologie comparée, UMR 7245 MCAM, CP52, 61 rue Buffon, 75231 Paris Cedex 05, France E-mail: [email protected], [email protected] 6Institute of Biological Sciences, Faculty of Science, University of Malaya, 50603 Kuala Lumpur, Malaysia E-mail: [email protected] 7Department of Parasitology, Graduate School of Medicine, Osaka City University, Abeno-ku, Osaka 545-8585, Japan 8Corresponding author. E-mail: [email protected] †In memory of our colleague Dr Odile Bain, who initiated this study and laid the ground work with her vast knowledge of the filarial worms and detailed morphological studies of the species presented in this paper Table of contents Abstract . -

Epidemiology of Angiostrongylus Cantonensis and Eosinophilic Meningitis
Epidemiology of Angiostrongylus cantonensis and eosinophilic meningitis in the People’s Republic of China INAUGURALDISSERTATION zur Erlangung der Würde eines Doktors der Philosophie vorgelegt der Philosophisch-Naturwissenschaftlichen Fakultät der Universität Basel von Shan Lv aus Xinyang, der Volksrepublik China Basel, 2011 Genehmigt von der Philosophisch-Naturwissenschaftlichen Fakult¨at auf Antrag von Prof. Dr. Jürg Utzinger, Prof. Dr. Peter Deplazes, Prof. Dr. Xiao-Nong Zhou, und Dr. Peter Steinmann Basel, den 21. Juni 2011 Prof. Dr. Martin Spiess Dekan der Philosophisch- Naturwissenschaftlichen Fakultät To my family Table of contents Table of contents Acknowledgements 1 Summary 5 Zusammenfassung 9 Figure index 13 Table index 15 1. Introduction 17 1.1. Life cycle of Angiostrongylus cantonensis 17 1.2. Angiostrongyliasis and eosinophilic meningitis 19 1.2.1. Clinical manifestation 19 1.2.2. Diagnosis 20 1.2.3. Treatment and clinical management 22 1.3. Global distribution and epidemiology 22 1.3.1. The origin 22 1.3.2. Global spread with emphasis on human activities 23 1.3.3. The epidemiology of angiostrongyliasis 26 1.4. Epidemiology of angiostrongyliasis in P.R. China 28 1.4.1. Emerging angiostrongyliasis with particular consideration to outbreaks and exotic snail species 28 1.4.2. Known endemic areas and host species 29 1.4.3. Risk factors associated with culture and socioeconomics 33 1.4.4. Research and control priorities 35 1.5. References 37 2. Goal and objectives 47 2.1. Goal 47 2.2. Objectives 47 I Table of contents 3. Human angiostrongyliasis outbreak in Dali, China 49 3.1. Abstract 50 3.2. -

Zoonotic Abbreviata Caucasica in Wild Chimpanzees (Pan Troglodytes Verus) from Senegal
pathogens Article Zoonotic Abbreviata caucasica in Wild Chimpanzees (Pan troglodytes verus) from Senegal Younes Laidoudi 1,2 , Hacène Medkour 1,2 , Maria Stefania Latrofa 3, Bernard Davoust 1,2, Georges Diatta 2,4,5, Cheikh Sokhna 2,4,5, Amanda Barciela 6 , R. Adriana Hernandez-Aguilar 6,7 , Didier Raoult 1,2, Domenico Otranto 3 and Oleg Mediannikov 1,2,* 1 IRD, AP-HM, Microbes, Evolution, Phylogeny and Infection (MEPHI), IHU Méditerranée Infection, Aix Marseille Univ, 19-21, Bd Jean Moulin, 13005 Marseille, France; [email protected] (Y.L.); [email protected] (H.M.); [email protected] (B.D.); [email protected] (D.R.) 2 IHU Méditerranée Infection, 19-21, Bd Jean Moulin, 13005 Marseille, France; [email protected] (G.D.); [email protected] (C.S.) 3 Department of Veterinary Medicine, University of Bari, 70010 Valenzano, Italy; [email protected] (M.S.L.); [email protected] (D.O.) 4 IRD, SSA, APHM, VITROME, IHU Méditerranée Infection, Aix-Marseille University, 19-21, Bd Jean Moulin, 13005 Marseille, France 5 VITROME, IRD 257, Campus International UCAD-IRD, Hann, Dakar, Senegal 6 Jane Goodall Institute Spain and Senegal, Dindefelo Biological Station, Dindefelo, Kedougou, Senegal; [email protected] (A.B.); [email protected] (R.A.H.-A.) 7 Department of Social Psychology and Quantitative Psychology, Faculty of Psychology, University of Barcelona, Passeig de la Vall d’Hebron 171, 08035 Barcelona, Spain * Correspondence: [email protected]; Tel.: +33-041-373-2401 Received: 19 April 2020; Accepted: 23 June 2020; Published: 27 June 2020 Abstract: Abbreviata caucasica (syn.