Analysis of
National Flagship Programme
National Rural Health Mission
(For the Years: 2009-10, 2010-2011 and 2011-12)
District: Chhatarpur
State: Madhya Pradesh
Supported by UNICEF
Under GoI – UN Joint Programme on Convergence
1
Disclaimer
With Technical support from Randstad India Limited for designing of tools, data analysis and drafting of the report. Data collection was carried out from the districts by the UNICEF supported District Facilitators under GoI-UN joint programme on convergence
2
Acronyms
ANM ANC
Auxiliary Nurse Midwife Ante Natal Care
ARSH ASHA AYUSH BPM BEmONC CEmONC CHC
Adolescent Reproductive and Sexual Health
Accredited Social Health Activist Ayurveda, Yoga and Naturopathy, Unani, Siddha and Homeopathy Block Programme Manager Basic Emergency Obstetric and Newborn Care Comprehensive Emergency Obstetric and Newborn Care Community Health Centre
- DH
- District Hospital
- DHAP
- District Health Action Plan
DHS DOT
District Health Society Directly Observed Therapy
DPM DPMU FGD
District Programme Manager District Programme Management Unit Focused Group Discussion
GP HIV HMIS ICDS IPHS JSY
Gram Panchayat Human Immunodeficiency Virus Health Management Information System
Integrated Child Development Services
Indian Public Health Standards Janani Suraksha Yojana
- LHV
- Lady Health Visitor
New Born Care Corner Pre-Conception Pre Natal Diagnostic Act Panchayat Raj Institute
NBCC PCPNDT PRI PHC PNC
Primary Health Centre Post Natal Care
RKS RTI STI SHC
Rogi Kalyan Samiti Reproductive Tract Infection Sexually Transmitted Infection Sub-Health Centre
- TT
- Tetanus Toxoid
VHND VHSC VHSNC
Village Health and Nutrition Day Village Health and Sanitation Committee Village Health, Sanitation and Nutrition Committee
3
Contents
A. Background……………………………………………………………………………………………………..…………………………..5 B. Objectives…………………………………………………………………………………………………..…………………………....….5 C. Material and Methodology……………………………………………………………………..………………………………......5 D. Results & Discussion…………………………………………………………………………….……………..……………………….7 1. Health Facilities…………………………………………………………………………………...……………..……………………….7 2. Infrastructure preparedness………………………………………………………………….….……..………………………....8 3. Service Delivery……………………………………………………………………………..…..……..……………………………….12 3.1 Maternal Care………………………………………………………………………………….……..………………………………..14 3.2 Child Care…………………………………………………………….……………………..………..………………………………….18
4. Communitisation of Maternal, Child and Comprehensive Care
4.1 ASHA programme……………………………………………………………………………..……..………………………………19
5 Platforms for Convergence
5.1 Village Health and Nutrition Day…………………………………………….……………….……..………………………..21 5.2 Village Health, Sanitation and Nutrition Committees………..…………………………… ……..………………..22 6. Training…………………………………………………………………………………………..……..…………………………………..24
7. Processes
7.1 Planning……………………………………………………………………………………………..…………………………………....25 7.2 Monitoring Structures………………………………………………………………………………..…………………………….27 8. Finance…………………………………………………………………………………………..……..…………………………………..28 E. Key Findings…………………………………………………………………………………….……..………………………………….29 F. Suggestions………………………………………………………………………………………..……..……………………………….33
Annexure
Fund utilization statement for the year 2009-10, 2010-11 and 2011-12..…………………………………37
4
A. BACKGROUND
The GOI- UNJPC programme is being implemented for promoting convergence at the district level to meet MDGs, improve participatory planning and implementation of plans and schemes, and strengthen monitoring at all levels; Government, Panchayats and Community. It also includes strengthening data collection and reporting mechanism for fund flows and social audit. The present study was carried out with support from UNICEF in 35 districts across 7 states of the country where GOI- UNJPC (UN Joint Programme on Convergence) is being implemented with the Planning Commission.
In Madhya Pradesh state, Chhatarpur is one of the districts covered under the aforesaid programme.
Analysis of the National Rural Health Mission (NRHM) was undertaken in this district to understand and assess the status of health services in the district and role of various stakeholders in planning and implementation, for achieving the targets set as per the District Programme Implementation Plan (PIP). As regards the relevant data/information on health services in the district and sub-district levels, the study examines the data available for the last three years; 2009-2010, 2010-2011 and 2011-12. The analysis was undertaken to identify areas which require strengthening and gaps that need to be addressed, which would be of help to the District Level Implementers and Planners to improve the implementation of the programme. It would also be of use to the State Governments to issue directives wherever required for making the programme effective and increasing its outreach.
B. OBJECTIVE
In District Chhatarpur, the study was undertaken with the following objectives:-
••
Analyse the processes and results, covering various elements and components of the programme as per the PIP for the years 2009-10, 2010-11 and 2011-12. Identify bottlenecks at different levels in planning and implementation of the programme.
•••
Assess the extent of outreach of the health services. Examine the role of functionaries and health workers at district, block and village levels. Identify the existing and possible areas of convergence.
C. MATERIAL AND METHODS
The methodology was a mix of quantitative and qualitative analysis including Desk review, data collection from secondary sources, Focus Group Discussions, In-depth interview and field visits.
Desk Review
A desk review/literature review was undertaken of the NRHM guidelines, DLHS-3 data, Programme Implementation plans (PIPs) at State and District level, HMIS data at the district level, Monthly and Annual Progress Reports, and Financial utilization statements at the District level. The documents were reviewed on the following thematic areas:-
5
••••••
District Planning under NRHM Financial Plans at district level and utilization District Health Infrastructure Human Resource for Health- Planning and Training Maternal and Child Health, including ASHA programme Convergence platforms at community level- Village level committees
Tool Development for Data Collection
Based on the desk review and following a participatory process, a tool was developed for quantitative and qualitative data collection. The tool was divided into the following three sections.
Section A - Statistical information from Secondary Sources. Section B - Checklist for observation during the field visit on the Village Health and Nutrition Day (VHND) Section C - Guidelines for discussions with focused groups and structured interview with District Planning Officer.
Statistical Information was collected for three years; 2009-10, 2010-11 and 2011-12, on the indicators; infrastructure availability in the district for implementing the programme, Maternal and Child Health including, Janani Suraksha Yojana (JSY) & ASHA programme, VHND, VHSNC and financial utilization in the district.
Under NRHM, VHND is recognized as one of the important platforms for inter-sectoral convergence between ICDS and NRHM. Through the checklist at Section B in the tool, information was collected on the planning and preparation undertaken for organizing VHND and services provided on that day.
A set of guidelines were prepared for discussions with the stakeholders who play or ought to be playing (as per the NRHM guidelines) a significant role in planning, implementing and monitoring the programme, to get an insight into their perspective and role at district, block and village level. Pointers for focused group discussions were also laid out for end line beneficiaries, for whom the programme is intended to; for obtaining their feedback and identify the areas that need strengthening. The following groups and officials were interacted with to collect qualitative information.
• ANMs • ASHAs • PRI representatives • Beneficiaries like pregnant women and lactating mothers, and out-door patients. • Village Health, Sanitation and Nutrition Committee members • District and Block Programme Managers • District Planning Officer
6
The draft tool was shared with District Facilitators (DF) who has been appointed under GOI- UNJPC and UNICEF officials. After incorporating the feedback the tool was pre-tested in the District-Rajgarh of State Madhya Pradesh. Following which the tool was finalized and in a one day orientation programme, the techniques for administering the tool in the districts was shared with the DFs.
Data Collection
The data collection was done by the District Facilitators during the period, January, 2012 to May, 2012.
For section A of the tool, the programmatic and financial data was collected from the following Secondary sources, i.e.; the databases maintained within the system.
District Health Data 2009-10, 2010-11 and 2011-12 District Programme Implementation Plan HMIS data at the District Level Fund utilization statement ICDS reports 2009 -10 and 2010-11 District specific data from DLHS-3, 2007-08 on the following indicators:
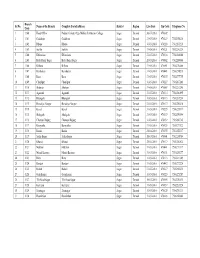
For Section B & C, qualitative information was collected from the three village of district Chhatarpur district. The each of these 3 villages was selected from different blocks. The socioeconomic status was the main criteria for selecting these villages like % SC population and low literacy of female. And all these villages are headed by a women sarpanch.
The profile of the 3 villages is given hereunder-
- Block
- GP
- Village
- SC
- ST Other Total
- % SC % ST
- %
- of Female
Literacy as per 2001 census
Nowgaon
Bijawar
11%
- Mau
- Sahaniya 1185
Heerapur 229 Dhimrwa 18
96 1869 3150 37.6 3.0
490 719 31.9 0.0
42 1086 1146 1.6 3.6
Sahaniya Jakhron Kala
8%
0
Buxwaha
12%
Dhimrwa
In each of the selected villages, FGDs were conducted with ANMs, ASHAs, PRI representatives, pregnant women, lactating mother and out-door patients. At the district level, in-depth interview was conducted with the District Planning Officer and FGD was conducted with district and block Programme managers.
7
D. RESULTS & DISCUSSIONS 1. Health Facilities in the District
Table 1 Health facilities in the district
Sr. No
1.
- Facility
- Number
- Medical College
- 0
1
2.
District Hospital
3.
- Civil Hospital
- 0
4.
Community Health Centres (CHC) Primary Health Centre (PHC) Sub-Health Centres (SHC) Civil Dispensaries Additional Primary Health Centres Ayurvedic Hospitals Ayurvedic Dispensaries Homeopathic Hospitals SNCU
10 36
192
1
5. 6. 7. 8.
0
9.
1
10. 11. 12. 13.
28
83
- NRC
- 7
Data source 1
The table above shown the status of district health institutions in the district, in which all the peripheral centre include AYUSH facilities mentioned. District have 1 DH, 10 Community Health Centre, 36 Primary Health Centre and 192 Sub Health Centre. There is no Civil Hospital in the district. AYUSH facilities are available in 10 health institutions.
2. Infrastructure preparedness 2.1 District Hospital (DH)
Table 2 Facilities in the District Hospital
Facility
District Hospital
Number
1
Nutritional Rehabilitation Centre Sick New Born Care Units (SNCU)
1 (20 bedded)
Level one 2, level two -1
Source2
1 Source data received from District Project Monitoring Unit, Chhatarpur 2 DPMU, Chhatarpur
8
In district Chhatarpur SNCU started in the year 2011. As per the IPHS standards, the DH has Malnutrition Treatment Centre/Nutritional Rehabilitation Centre and SNCU.
In 2009-10 the district reported 733 neonatal deaths and it increased to 818 and 783 in the subsequent year; 2010-11, 2011-12. In 2009-10 5.4%, in 2010-11, 4.9% and in 2011-12 10% new-borns were underweight.
2.2 Community Health Centre (CHC)
Table 3 Status of the Community Health Centre
- Status of CHCs
- 2009-10
- 2010-11
- 2011-12
- 11
- Total no. of CHC required as
per Population Norms Total no. of CHCs
- 10
- 10
10
2
10
2
10
- 2
- CHCs
- qualified
- to
- be
Comprehensive Emergency Obstetric and New Born Care (CEmONC)
Note – CHCs required for 2009-10 and 2010-11 as per 2001 Census and 2011-12 as per 2011 census.
Table 4 Facilities at the Community Health Centre
- Facilities at CHC
- 2009-10
- 2010-11
- 2011-12
CHCs with blood storage facility
- 0
- 0
- 0
CHCs with surgery facility
- 2
- 2
- 2
District Chhatarpur has 10 Community Health Centres (CHCs) out of that two centres are equipped with CEmONC facility i.e. CHC Nowgaong and CHC Bada Malhera while CHC Luvkush Nagar is identified to equip as CEmONC facility. Although, both the CEmONC CHCs equipped with surgery facility however no blood storage unit establish in CEmONC.
Human Resource in CHCs
Table 5 Status of Human Resources at the Community Health Centre as on August 20123
- Regular
- Contractual
- Post
- Sanction
- Available
- Sanction
- Available
Specialists
- Anesthesia
- 3 (one each at
CEmONC CHC)
10
- -
- -
- -
Obstetric & Gynecologist Pediatrics
11
--
-
- -
- 3 (one each at
CEmONC CHC)
- 10
- Physician
- 1
- -
- -
3 Table 3,4,5 data received from DPMU Chhatarpur.
9
- Surgeon
- 10
- 1
- -
- -
Other Staff
MO-Allopathic MO-AYUSH Pharmacist Staff Nurse ANM/HW(Female) LHV
23 10 18 51 29 14 12 10
11
1
5-
4-
11 11 38
8
- -
- -
6
14
-
38-
Lab. Technician Radiographer
- 5
- 5
-
5
- -
- 3
Total
- 203
- 92 (45 %)
- 30
- 20 (67%)
In CHCs, total 55% regular posts are vacant against the total sanctioned position while 33% contractual posts are vacant only 11% posts of specialist Doctors are filled against the total sanctioned positions. Anesthesia and Pediatrician post sanction in CEmONC CHC.
In last three years (from 2009-10 to 2011-12) Total 34% of the institutional deliveries are conducted in the CHCs. Two CHCs are functioning as CEmONC i.e. Nowgaon and Bada Malhera while 7 CHCs are strengthen as BEmONC. Thus, it is clearly indicated that there is strong need to fill the vacant posts at the CHCs in order to enhance the services.
2.3 Primary Health Centre (PHC)
Table 6 Facilities at the Public Health Centres
Facility at PHC
Total No. of PHCs required as per Population norms
- 2009-10
- 2010-11
- 2011-12
- 45
- 38
- 38
Total No. of PHCs exists No. of PHCs with Basic Emergency Obstetric and New
33
6
36 16
36 16
Born Care (BEmONC) facilities No. of PHCs with New Born Care Corners No. of PHCs with labour room facility
- 8
- 19
33
19
- 33
- 29
The district has 36 PHCs and in 2011-12, 16 PHCs centres were upgraded and qualified as BEmONC (Basic Emergency Obstetric and New Born Care) centre however presently 12 PHCs are providing emergency obstetric care while 3 PHCs are being targeted to make functional in this year (2012-13), the delivery cases are referred to District Hospital from where there obstetric facilities are not available. 37% of the total institutional deliveries take place in the PHCs. In 2010-2011 New Born Care Corners (NBCCs) were established in 19 PHCs to provide
10
care to the sick new-borns. 33 PHCs are having labour room facility. 28 PHCs have one medical officer.
Human Resource in PHCs
Table 7 - Status of Human Resource in Primary Health Centres as on August 20124
- Positions filled
- Positions
vacant
% of vacant positions
Posts Name
MO – Allopathy MO – AYUSH
San.
51
Aval.
- 33
- 18
23
65
- 26
- 31
- 8
Pharmacist Staff Nurse
35
4
19
1
16
3
54 25
ANM/HW (Female)
LHV
56 34
56 28
06
100
82
Health Worker (Male) Health Asst. (Male)
Lab Technician
25
10
-46
214
0
80 60
- Total
- 228
- 155
(68%)
73
(32%)
In PHCs total 73 (32%) staff positions are laying vacant, in which 35% positions of Medical Officer allopathic, 74% MO AYUSH, 46% pharmacist and 40% Laboratory Technicians post are vacant. Regular and Contractual both type posts are vacant, 69% regular post are vacant while 43% contractual posts are vacant in PHCs. It is suggested that the key positions like Medical Officer, ANM, Lab Technician and pharmacist should not be vacant.
2.4 Sub Health Centre (SHC)
Table 8 Status of the Sub Health Centres
Number of SHCs
Required as per population norms Functional SHCs
- 2009-10
- 2010-11
- 2011-12
- 272
- 230
192
230
- 192
- 192
- Functioning from Government Building
- 73
- 93
- 93