Research Article FEM Analysis of Mandibular Prosthetic Overdenture Supported by Dental Implants: Evaluation of Different Retention Methods
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Table of Contents
Table of Contents Welcome Message from the General Chair.......................................................... 2 M&N 2019 Organizers .......................................................................................... 3 Sponsors .............................................................................................................. 6 Patrons ................................................................................................................. 7 Exhibitors ............................................................................................................ 10 Monday, July 8 ....................................................................................................12 Tuesday, July 9 ................................................... ................................................19 Wednesday, July 10 ........................................................................................... 26 1 Welcome Message from the General Co-Chairs Dear colleagues and friends, On behalf of the entire Conference Committee, we are pleased to welcome you to the 5th IEEE International Symposium on Measurements and Networking (M&N 2019), which is held in Catania and hosted in Museo Diocesano in the heart of the city. The Symposium is mainly promoted by the IEEE IMS TC-37 Measurements and Networking, the IEEE IM Italy Chapter and by the IEEE Italy Section Systems Council Chapter. IEEE M&N is a privileged forum for the discussion of current and emerging trends on measurements, communications, computer science, -

67Th Economic Policy Panel
67th Economic Policy Panel Hosted by the Swiss National Bank Venue: Great Guild Hall, 2nd Floor, Zunfthaus zur Zimmerleuten Limmatquai 40, 8001 Zurich, Switzerland 12-13 April 2018 Programme Each session is 70 minutes in duration Author: 25 mins | Discussant: 15 mins (each) | Panel discussion: 15 mins * indicates presenting author Thursday 12 April 14:00 Registration and coffee on arrival 14:30 – 14:45 Opening Remarks Mr Thomas Moser, Alternate Member of the Governing Board, Swiss National Bank 14:45 – 15:55 Can Education Compensate the Effect of Population Aging on Macroeconomic Performance? Evidence from Panel Data Rainer Kotschy (LMU Munich) * Uwe Sunde (LMU Munich) Discussants: Francesco Drago (University of Messina) Pietro Biroli (University of Zurich) 15:55 – 17:05 Monetary Policy and Bank Profitability in a Low Interest Rate Environment * Carlo Altavilla (European Central Bank) Miguel Boucinha (European Central Bank) José-Luis Peydró (ICREA-UPF, CREI & BGSE) Discussants: Ralph De Haas (EBRD) Vasso Ioannidou (University of Lancaster) 17:05 – 17:20 coffee break 17:20 – 18:30 The Walking Dead?: Zombie Firms and Productivity Performance in OECD Countries Müge Adalet McGowan (OECD) Dan Andrews (OECD) * Valentine Millot (OECD) Discussants: Martin Brown (University of St.Gallen) Elena Carletti (Bocconi University) 20:00 Conference dinner at The Ballroom of the Savoy Hotel Baur en Ville Address: Poststrasse 12, 8001 Zurich Welcome address by Ms Andréa M. Maechler, Member of the Governing Board, Swiss National Bank Friday 13 April 08:30 – 09:40 Where Do People Get Their News? * Patrick Kennedy (Columbia University) Andrea Prat (Columbia University) Discussants: Roberto Galbiati (Sciences Po) David Hémous (University of Zurich) 09:40 – 10:50 Populism and Civil Society * Tito Boeri (Bocconi University) Prachi Mishra (IMF) Chris Papageorgiou (IMF) Antonio Spilimbergo (IMF) Discussants: Christina Gathmann (Heidelberg University) 10:50 – 11:10 Coffee break 11:10 – 12:20 The Gains from Economic Integration David Comerford (University of Strathclyde) * José V. -

MARILENA BAZZANO Educational Activity 2020-2021
CURRICULUM VITAE – MARILENA BAZZANO Educational Activity 2020-2021 - Lecturer in Veterinary Internal Medicine Practical Activities (1 CFU), School of Veterinary Medicine, University of Camerino (UNICAM). 2020-2021 – Lecturer in Veterinary Obstetric Techniques (5 CFU), Post-Graduate School of Animal Health, Breeding and Production, University of Camerino (UNICAM) 2020-2021 – Lecturer in Control of Diseases in Livestock Production Systems (5 CFU), Animal Production Science and Valorization of Animal Derived Food, University of Camerino (UNICAM). 2019-2020 – Lecturer in Control of Diseases in Livestock Production Systems (5 CFU), Animal Production Science and Valorization of Animal Derived Food, University of Camerino (UNICAM). 2019-2020 - Lecturer in Veterinary Internal Medicine Practical Activities (3 CFU), School of Veterinary Medicine, University of Camerino (UNICAM). 2019-2020 – Lecturer in Veterinary Obstetric Techniques (10 CFU), Post-Graduate School of Animal Health, Breeding and Production, University of Camerino (UNICAM) 2018-2019 – Lecturer in Veterinary Sport Medicine (3 CFU), School of Veterinary Medicine, University of Camerino (UNICAM). 2018-2019 – Lecturer in Veterinary Internal Medicine Practical Activities (3 CFU), School of Veterinary Medicine, University of Camerino (UNICAM). 2018-2019 – Lecturer in Veterinary Obstetric Techniques (10 CFU), Post-Graduate School of Animal Health, Breeding and Production, University of Camerino (UNICAM) Work Experience and Education 2019-2020 – Tutor UNICAM for Post-Graduate grant of Dr. Marta Florence David in cooperation With the School of Veterinary Medicine of the University of Liege. 2017-2019 – Co-Supervisor of PhD course in Life and Health Sciences: One Health. XXXI Cycle. School of Advanced Studies, university of Camerino. Thesis “Study of a neW formulation of functional food for dogs With chronic renal and cardiovascular diseases”, PhD student Dr. -
Print Special Issue Flyer
IMPACT FACTOR 5.076 an Open Access Journal by MDPI Graphene-Based Materials for Cancer Therapy Guest Editors: Message from the Guest Editors Prof. Dr. Daniela Iannazzo Dear Colleagues, Department of Engineering, University of Messina, Contrada Graphene-based nanomaterials such as fullerenes, carbon Di Dio, I-98166 Messina, Italy nanotubes, graphene oxide and graphene quantum dots [email protected] have shown great potential in nanomedicine and biotechnology. Their physical and chemical properties and Prof. Dr. Alessandro Pistone Department of Engineering, the presence of more reactive groups on the graphene University of Messina, Contrada surface, which allow the multimodal conjugation with Di Dio, I-98166 Messina, Italy different functional groups and biologically active [email protected] molecules, make them ideal candidates for cancer diagnosis and treatment. These nanomaterials have been conjugated with drugs and tumor-targeting ligands for a more efficient targeted delivery and have been also Deadline for manuscript submissions: investigated as imaging agents and biosensors for the 31 October 2021 identification of cancer bio-markers. “Graphene-based materials for cancer therapy” aims at collecting full papers communications and reviews that prominently demonstrate the continuous efforts in developing advanced, graphene-based nanomaterials for cancer treatment and diagnosis. Prof. Daniela Iannazzo Prof. Alessandro Pistone Guest Editors mdpi.com/si/23260 SpeciaIslsue IMPACT FACTOR 5.076 an Open Access Journal by MDPI Editor-in-Chief Message from the Editor-in-Chief Prof. Dr. Shirley Chiang Nanoscience and nanotechnology are exciting fields of Department of Physics, University research and development, with wide applications to of California Davis, One Shields electronic, optical, and magnetic devices, biology, Avenue, Davis, CA 95616-5270, USA medicine, energy, and defense. -

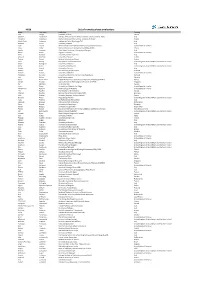
Reviewers 2020
AP&T Reviewers 2020 Highlighted reviewer denotes a top reviewer for 2020 Reviewer Last Name Reviewer First Name Reviewer Institution Reviewer Country/Region Abdel-Daim Mohamed Suez Canal University Egypt Abergel Armand Hôtel-Dieu France Abraham Neena Mayo Clinic Scottsdale United States Abraldes Juan University of Alberta Canada Afdal Nezam Beth Israel Deaconess Medical Center United States Afolabi Paul University of Soutjampton United Kingdom of Great Britain and Northern Ireland Afzal Nadeem Southampton University Hospital Trust United Kingdom of Great Britain and Northern Ireland Agardh Daniel Pediatrics Epidemiology Center United States Agarwal Banwari Royal Free Hospital United Kingdom of Great Britain and Northern Ireland Agarwal Kosh United Kingdom of Great Britain and Northern Ireland Aggarwal Rakesh Sanjay Gandhi Postgraduate Institute of Medical Sciences India Aghemo Alessio Istituto Clinico Humanitas Italy Agnholt Jørgen Aarhus University Hospital Denmark Ahmad Tariq Royal Devon and Exeter NHS Foundation Trust United Kingdom of Great Britain and Northern Ireland Ahuja Vineet All India Institute of Medical Sciences India Aithal Guruprasad University of Nottingham United Kingdom of Great Britain and Northern Ireland Alazawi William Barts and The London School of Medicine and Dentistry United Kingdom of Great Britain and Northern Ireland Alexopoulou Alexandra Greece Allez Matthieu Hôpital Saint-Louis France Allin Kristine Alpers David Washington Univ School of Medicine United States Amiot Aurélien Henri Mondor University Hospital -

Identification of a Novel Parvovirus in Domestic Cats
Veterinary Microbiology 228 (2019) 246–251 Contents lists available at ScienceDirect Veterinary Microbiology journal homepage: www.elsevier.com/locate/vetmic Identification of a novel parvovirus in domestic cats T Georgia Diakoudia, Gianvito Lanavea, Paolo Capozzaa, Federica Di Profiob, Irene Melegarib, Barbara Di Martinob, Maria Grazia Pennisic, Gabriella Eliaa, Alessandra Cavallia, ⁎ Maria Tempestaa, Michele Cameroa, Canio Buonavogliaa, Krisztián Bányaid, Vito Martellaa, a Department of Veterinary Medicine, University of Bari, Valenzano, Italy b Faculty of Veterinary Medicine, University of Teramo, Teramo, Italy c Department of Veterinary Science, University of Messina, Italy d Institute for Veterinary Medical Research, Centre for Agricultural Research, Hungarian Academy of Sciences, Budapest, Hungary ARTICLE INFO ABSTRACT Keywords: A novel protoparvovirus species was identified in domestic cats. The virus was distantly related to the well- Parvovirus known feline (feline panleukopenia virus) and canine (canine parvovirus type 2) parvoviruses, sharing low Protoparvovirus nucleotide identities in the capsid protein 2 (less than 43%). The virus was genetically similar (100% at the Bufavirus nucleotide level) to a newly identified canine protoparvovirus, genetically related to human bufaviruses. The Cat feline bufavirus appeared as a common element of the feline virome, especially in juvenile cats, with an overall Respiratory infections prevalence of 9.2%. The virus was more common in respiratory samples (9.5%–12.2%) than in enteric samples of cats (2.2%). The role of bufaviruses in the etiology of feline respiratory disease complex, either as a primary or a secondary agents, should be defined. 1. Introduction described in cats (Lau et al., 2012; Ng et al., 2014; Zhang et al., 2014) (Table 1). -

New Strategies for the Post-Marketing Monitoring of Medical Products
ISP E 201 1Mid-Year Meeting FFlloorreennccee,, ITALY > APRIL 9-11, 2011 JOINTLY SPONSORED BY ISPE • International Society for Pharmacoepidemiology SIF • Italian Society of Pharmacology SIMG • Italian College of General Practitioners PRELIMINARY Meeti ng V enue agenda Grand Hotel Baglioni Symposium April 9, 2011 ******** New Strategies for the Post-marketing Monitoring of Medical Products Piazza Unità Italiana, 6 07 :30 REGISTRATION AFTERNOON SESSION 1 16 :35 Federation of databases to evaluate the arrhythmogenic 50123 - Florence, Italy 09 :00 INTRODUCTION TO PROGRAM NEW APPROACHES IN DRUG SAFETY potential of drugs: Giampiero Mazzaglia, Program Co-Chair, Health Search, SIGNAL DETECTION The ARITMO project Italian College of General Practitioners, Italy Co-chairs Fabrizio De Ponti, Gianluca Trifirò, Program Co-Chair, Erasmus University Giovanni Corrao, University of Milan Bicocca, Italy University of Bologna, Italy Medical Center, The Netherlands & University of Messina, Italy Marie Lindqvist , WHO Collaborating WELCOME ADDRESSES Centre for International Drug Monitoring, Sweden 17 :00 A network of long-term care facilities: Scientific Committee Achille Caputi, Italian Society of Pharmacology Experience from Europe and USA Past-President , University of Messina, Italy 13 :30 From individual case report assessment to Giovanni Gambassi, Sacro Cuore University CO -CHAIR Claudio Cricelli, Italian College of General Practitioners quantitative signal detection using spontaneous of Rome, Italy Giampiero Mazzaglia President , Italy ADR reporting: What -

Does Paternal Unemployment Affect Young Adult Offspring's Personality
Does Paternal Unemployment Affect Young Adult Offspring’s Personality? Viola Angelini∗ Marco Bertoniy Luca Corazziniz Abstract Using longitudinal data from the German Socio-Economic Panel (SOEP), we analyse the impact of paternal unemployment on the \Big 5" personality traits of young adult offspring aged 17 to 25. Results from longitudinal value-added models for personality show that paternal unemployment makes offspring significantly more conscientious and less neurotic. The uncovered effects are robust to the presence of selection on unobservables and of correlation between the error term and the lagged outcome. We also discuss the potential mechanisms behind our findings. JEL classification: J24, J13, J64, C33. Keywords: personality traits, unemployment, household behaviour, SOEP. ∗Department of Economics, Econometrics and Finance, University of Groningen, PO Box 800, Groningen, 9700 AV, The Netherlands, and Netspar, PO Box 90153, Tilburg, 5000 LE, The Netherlands. Email: [email protected] yCorresponding author. Department of Economics and Management, University of Padova, via del Santo, 33, 35123 Padova, Italy. Phone: +49-049-8274050. Email: [email protected] zDepartment of Economics, University of Messina, P. zza XX Settembre, 4, 98122, Messina, Italy and ISLA, Bocconi University, via R¨ontgen, 1, Milan 20136, Italy. Email: [email protected] 1 1 Introduction Recent empirical evidence both in economics and in psychology shows that personality traits have strong predictive power for a wide range of socio-economic outcomes (Alm- lund et al., 2011, Borghans et al., 2008, Brunello and Schlotter, 2011, Bucciol et al., 2015). Personality matters for job performances and wages (Barrick and Mount, 1991, Hogan and Holland, 2003, Nyhus and Pons, 2005, Salgado, 1997), educational attain- ment (Borghans et al., 2008, Duncan et al., 2007, Goldberg et al., 1998, Poropat, 2009), longevity (Friedman et al., 2010, Roberts et al., 2007, Savelyev, 2014), health-related behaviours (Hampson et al., 2007) and criminal behaviours (John et al., 1994, O'Gorman and Baxter, 2002). -

Università Degli Studi Di Messina
Università degli Studi di Messina PUBLIC COMPETITION, BY QUALIFICATIONS AND EXAMINATIONS, FOR ADMISSION TO PHD COURSES ACTIVATED AT THE UNIVERSITY OF MESSINA 36TH CYCLE THE RECTOR IN VIEW OF the Law No. 476 of 13th August 1984 "Regulations on scholarships and PhD course in Universities" and subsequent amendments; IN VIEW OF the Law No. 168 of 9th May 1989, that established the Ministry of University and Scientific and Technological Research; IN VIEW OF the Law No. 241 of 2nd August 1990, containing "Rules on administrative procedure and right of access to administrative documents" and subsequent amendments and additions; IN VIEW OF the Law No. 210 of 3rd July 1998, with particular reference to art. 4 and subsequent amendments; IN VIEW OF the European Union Regulation No. 679 of 27th April 2016, regarding the protection of personal data (G.D.P.R.); IN VIEW OF the Ministerial Decree No. 270 of 22nd October 2004, with particular reference to articles 3 and 6 and subsequent amendments; IN VIEW OF the electronic Bulletin No. 14, 23rd-24thJanuary 2008 of the CUN relating to the assignment of master's degrees to the CUN Areas; IN VIEW OF the art. 19 paragraph 1 of the Law No. 240 of 30th December 2010, which modified art. 4 of the Law No. 210 of 3rdJuly 1998, containing rules on the PhD courses; IN VIEW OF the articles 7 and 8 of EU Regulation 1304/2013 on promoting equality between men and women, increasing the sustainable participation and progress of women in the employment sector, combating the feminization of poverty; IN VIEW OF the University Statute, issued with D.R. -

Dear International Student, Welcome to the University of Messina. Your Time Here Will Be Both Challenging and Exciting
Dear International Student, Welcome to the University of Messina. Your time here will be both challenging and exciting. As you know, academic mobility is vital to enhance European competitiveness. Mobility contributes to building up a knowledge-based society where awareness of cultural diversity and traditions is an incentive, rather than an obstacle, to innovation and international cooperation. This Handbook is designed to assist you while you are preparing to study in Messina and to advise you on how to organize your stay. MESSINA Several times destroyed, several times rebuilt, the ancient Zancle, later called Messanion, has been stubbornly reconstructed on the same site. Wars and earthquakes have changed its appearance but have not affected the perseverance of its inhabitants. One of its historical buildings the courtly Palazzata, facing the port, was razed to the ground by two devastating earthquakes, the first in 1783 and the second in 1908 when more than a hundred thousand people died. The new Messina was subsequently rebuilt with anti-seismic systems and a modern urban design. Nowadays very little remains of its architectural heritage: the Cathedral’s original facade dating back to the 12th century; one of Montorsoli’s masterpieces, Orion’s Fountain, which is in the Cathedral square; other historical monuments located in the city centre include the Church of the Catalans, a Byzantine construction with Arabic influences, and the 19th century Vittorio Emanuele Gallery. The statue of the Virgin of the Letter, placed at the entrance to Messina’s harbour, bears testimony to local religious traditions. She blesses Messina and all visitors arriving or departing from the City of the Strait. -

UH CV (September 6, 2014)
University of Houston, Liberal Studies Program, 232 McElhinney Bldg., 4800 Calhoun Road, Houston, TX 77204–5020 713–743–3987 [email protected] www.uh.edu/class/ccs/people/luca-oliva/index.php LUCA OLIVA September 6, 2014 APPOINTMENTS 2015 University of Bergamo, Visiting Professor 2014–present University of Houston, Instructional Assistant Professor 2012–2014 University of Houston, Adjunct Professor 2011, 2014 University of St. Thomas Houston, Adjunct Professor 2010–11 Salem State University, Visiting Professor 2008–11 Boston College, Adjunct Professor 2005–07 State University of Milan, Adjunct Professor 1998–2005 State University of Milan, Teaching Assistant AREAS OF SPECIALIZATION Philosophy of Mathematics, Ethical Theories, Kantian Philosophy AREAS OF COMPETENCE Ethics and Applied Ethics, History of Philosophy (especially the Modern), Logic (including Critical Reasoning), Philosophy of Mathematics EDUCATION Ph.D. Philosophy, State University of Milan (2006) B.A. Philosophy, State University of Milan (Summa cum Laude, 2001) SELECTED PUBLICATIONS “On Kantian Intuitions”, in P. Muchnik and O. Thorndike (ed.s), Rethinking Kant, Volume 5. Cambridge Scholars Publishing, 2015. “Kant and the Neo-Kantians on Mathematics”, in N. De Warren and A. Staiti (ed.s), The Legacy of NeoKantianism. New York: Cambridge University Press, 2015, 406–47. “SullʼEpistemologia Rickertiana”, in L. Oliva (ed.), Heinrich Rickert – L’Uno, l’Unità e il Numero Uno. Osservazioni sulla Logica del Concetto di Numero. Milano: Cusl, 2008, 5–31. “Analisi e Pluralismo nell’Ontologia di Rickert”, in R. Lazzari (ed.), Studi in Onore di Alfredo Marini. Milano: Mimesis, 2008, 167–185. “Il Senso dei Valori nell’Etica Rickertiana”, Idee 67 (2008): 85–102. La Validità come Funzione dell’Oggetto. -
List of Remote Phase Evaluators
HR20 List of remote phase evaluators Name Last name Institution Country Alan Altraja University of Tartu Estonia Martine Ammassari National Research council (CNR) and Santa Lucia Foundation, Roma Italy Evangelos Andreakos Biomedical Research Foundation, Academy of Athens Greece Maria Grazia Andreassi Institute of Clinical Physiology-CNR Italy Beatrice Arosio University of Milan Italy Aarti Asnani Beth Israel Deaconess Medical Center/Harvard Medical School United States of America Anne Astier Centre National de la Recherche Scientifique (CNRS) France Alessio Avenanti Alma Mater Studiorum - University of Bologna Italy Babak Baban Augusta University United States of America Fabio Babiloni University of Rome Sapienza Italy Manuela Baccarini University of Vienna Austria Tomasz Baczek Medical University of Gdansk Poland Udai Banerji The Institute of Cancer Research United Kingdom of Great Britain and Northern Ireland Mario Barbagallo University of Palermo Italy Barbu Barbu University of Portsmouth United Kingdom of Great Britain and Northern Ireland Valeria Barresi University of Verona Italy Markus Barth The University of Queensland Australia Susanta Behura University of Missouri United States of America Theodora Benedek University of Medicine and Pharmacy Tirgu Mures Romania Ales Berlec Jozef Stefan Institute Slovenia Sonia Berrih-Aknin Institut National de la Santé Et de la Recherche Médicale (INSERM) France Kishore Bhakoo Agency for Science Technology and Research (A*STAR) Singapore Per Björkman Lund University Sweden Armin Blesch University