3.2.1 Safety of Antibiotic Ear Drops in Children with Grommets
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(CD-P-PH/PHO) Report Classification/Justifica
COMMITTEE OF EXPERTS ON THE CLASSIFICATION OF MEDICINES AS REGARDS THEIR SUPPLY (CD-P-PH/PHO) Report classification/justification of medicines belonging to the ATC group D07A (Corticosteroids, Plain) Table of Contents Page INTRODUCTION 4 DISCLAIMER 6 GLOSSARY OF TERMS USED IN THIS DOCUMENT 7 ACTIVE SUBSTANCES Methylprednisolone (ATC: D07AA01) 8 Hydrocortisone (ATC: D07AA02) 9 Prednisolone (ATC: D07AA03) 11 Clobetasone (ATC: D07AB01) 13 Hydrocortisone butyrate (ATC: D07AB02) 16 Flumetasone (ATC: D07AB03) 18 Fluocortin (ATC: D07AB04) 21 Fluperolone (ATC: D07AB05) 22 Fluorometholone (ATC: D07AB06) 23 Fluprednidene (ATC: D07AB07) 24 Desonide (ATC: D07AB08) 25 Triamcinolone (ATC: D07AB09) 27 Alclometasone (ATC: D07AB10) 29 Hydrocortisone buteprate (ATC: D07AB11) 31 Dexamethasone (ATC: D07AB19) 32 Clocortolone (ATC: D07AB21) 34 Combinations of Corticosteroids (ATC: D07AB30) 35 Betamethasone (ATC: D07AC01) 36 Fluclorolone (ATC: D07AC02) 39 Desoximetasone (ATC: D07AC03) 40 Fluocinolone Acetonide (ATC: D07AC04) 43 Fluocortolone (ATC: D07AC05) 46 2 Diflucortolone (ATC: D07AC06) 47 Fludroxycortide (ATC: D07AC07) 50 Fluocinonide (ATC: D07AC08) 51 Budesonide (ATC: D07AC09) 54 Diflorasone (ATC: D07AC10) 55 Amcinonide (ATC: D07AC11) 56 Halometasone (ATC: D07AC12) 57 Mometasone (ATC: D07AC13) 58 Methylprednisolone Aceponate (ATC: D07AC14) 62 Beclometasone (ATC: D07AC15) 65 Hydrocortisone Aceponate (ATC: D07AC16) 68 Fluticasone (ATC: D07AC17) 69 Prednicarbate (ATC: D07AC18) 73 Difluprednate (ATC: D07AC19) 76 Ulobetasol (ATC: D07AC21) 77 Clobetasol (ATC: D07AD01) 78 Halcinonide (ATC: D07AD02) 81 LIST OF AUTHORS 82 3 INTRODUCTION The availability of medicines with or without a medical prescription has implications on patient safety, accessibility of medicines to patients and responsible management of healthcare expenditure. The decision on prescription status and related supply conditions is a core competency of national health authorities. -
Instruction Sheet: Otitis Externa
University of North Carolina Wilmington Abrons Student Health Center INSTRUCTION SHEET: OTITIS EXTERNA The Student Health Provider has diagnosed otitis externa, also known as external ear infection, or swimmer's ear. Otitis externa is a bacterial/fungal infection in the ear canal (the ear canal goes from the outside opening of the ear to the eardrum). Water in the ear, from swimming or bathing, makes the ear canal prone to infection. Hot and humid weather also predisposes to infection. Symptoms of otitis externa include: ear pain, fullness or itching in the ear, ear drainage, and temporary loss of hearing. These symptoms are similar to those caused by otitis media (middle ear infection). To differentiate between external ear infection and middle ear infection, the provider looks in the ear with an instrument called an otoscope. It is important to distinguish between the two infections, as they are treated differently: External otitis is treated with drops in the ear canal, while middle ear infection is sometimes treated with an antibiotic by mouth. MEASURES YOU SHOULD TAKE TO HELP TREAT EXTERNAL EAR INFECTION: 1. Use the ear drops regularly, as directed on the prescription. 2. The key to treatment is getting the drops down into the canal and keeping the medicine there. To accomplish this: Lie on your side, with the unaffected ear down. Put three to four drops in the infected ear canal, then gently pull the outer ear back and forth several times, working the medicine deeper into the ear canal. Remain still, good-ear-side-down for about 15 minutes. -

Objective Measures of Ototoxicity
The following article appeared in the September 2005 issue (Vol. 9, No. 1, pp. 10-16) of the Division 6 publication Perspectives on Hearing and Hearing Disorders: Research and Diagnostics. To learn more about Division 6, contact the ASHA Action Center at 1-800-498-2071 or visit the division’s Web page at www.asha.org/about/membership-certification/divs/div_6.htm. Objective Measures of Ototoxicity Elizabeth Leigh-Paffenroth Veterans Affairs Rehabilitation Research and Development Service, National Center for Rehabilitative Auditory Research, VA Medical Center Portland, OR Department of Otolaryngology, Oregon Health & Science University Portland, OR Kelly M. Reavis, Jane S. Gordon, Kathleen T. Dunckley Veterans Affairs Rehabilitation Research and Development Service, National Center for Rehabilitative Auditory Research, VA Medical Center Portland, OR Stephen A. Fausti and Dawn Konrad-Martin Veterans Affairs Rehabilitation Research and Development Service, National Center for Rehabilitative Auditory Research, VA Medical Center Portland, OR Department of Otolaryngology, Oregon Health & Science University, Portland, OR A leading cause of preventable sensorineural hear- of patients who are unable to provide reliable re- ing loss is therapeutic treatment with medications that sponses; subsequently, many of these patients do not are toxic to inner ear tissues, including certain drugs receive monitoring for ototoxic-induced changes in used to fight cancer and life-threatening infectious dis- their hearing. The development of objective measures eases. Ototoxic-induced hearing loss typically begins that do not require patient cooperation is necessary to in the high frequencies and progresses to lower fre- monitor all patients receiving ototoxic drugs. quencies as drug administration continues (Campbell Two objective measures offer promise in their abil- & Durrant, 1993; Campbell et al., 2003; Macdonald, ity to detect and to monitor hearing changes caused by Harrison, Wake, Bliss, & Macdonald, 1994). -

ICD-9 Diseases of the Ear and Mastoid Process 380-389
DISEASES OF THE EAR AND MASTOID PROCESS (380-389) 380 Disorders of external ear 380.0 Perichondritis of pinna Perichondritis of auricle 380.00 Perichondritis of pinna, unspecified 380.01 Acute perichondritis of pinna 380.02 Chronic perichondritis of pinna 380.1 Infective otitis externa 380.10 Infective otitis externa, unspecified Otitis externa (acute): NOS circumscribed diffuse hemorrhagica infective NOS 380.11 Acute infection of pinna Excludes: furuncular otitis externa (680.0) 380.12 Acute swimmers' ear Beach ear Tank ear 380.13 Other acute infections of external ear Code first underlying disease, as: erysipelas (035) impetigo (684) seborrheic dermatitis (690.10-690.18) Excludes: herpes simplex (054.73) herpes zoster (053.71) 380.14 Malignant otitis externa 380.15 Chronic mycotic otitis externa Code first underlying disease, as: aspergillosis (117.3) otomycosis NOS (111.9) Excludes: candidal otitis externa (112.82) 380.16 Other chronic infective otitis externa Chronic infective otitis externa NOS 380.2 Other otitis externa 380.21 Cholesteatoma of external ear Keratosis obturans of external ear (canal) Excludes: cholesteatoma NOS (385.30-385.35) postmastoidectomy (383.32) 380.22 Other acute otitis externa Excerpted from “Dtab04.RTF” downloaded from website regarding ICD-9-CM 1 of 11 Acute otitis externa: actinic chemical contact eczematoid reactive 380.23 Other chronic otitis externa Chronic otitis externa NOS 380.3 Noninfectious disorders of pinna 380.30 Disorder of pinna, unspecified 380.31 Hematoma of auricle or pinna 380.32 Acquired -

Etats Rapides
List of European Pharmacopoeia Reference Standards Effective from 2015/12/24 Order Reference Standard Batch n° Quantity Sale Information Monograph Leaflet Storage Price Code per vial Unit Y0001756 Exemestane for system suitability 1 10 mg 1 2766 Yes +5°C ± 3°C 79 ! Y0001561 Abacavir sulfate 1 20 mg 1 2589 Yes +5°C ± 3°C 79 ! Y0001552 Abacavir for peak identification 1 10 mg 1 2589 Yes +5°C ± 3°C 79 ! Y0001551 Abacavir for system suitability 1 10 mg 1 2589 Yes +5°C ± 3°C 79 ! Y0000055 Acamprosate calcium - reference spectrum 1 n/a 1 1585 79 ! Y0000116 Acamprosate impurity A 1 50 mg 1 3-aminopropane-1-sulphonic acid 1585 Yes +5°C ± 3°C 79 ! Y0000500 Acarbose 3 100 mg 1 See leaflet ; Batch 2 is valid until 31 August 2015 2089 Yes +5°C ± 3°C 79 ! Y0000354 Acarbose for identification 1 10 mg 1 2089 Yes +5°C ± 3°C 79 ! Y0000427 Acarbose for peak identification 3 20 mg 1 Batch 2 is valid until 31 January 2015 2089 Yes +5°C ± 3°C 79 ! A0040000 Acebutolol hydrochloride 1 50 mg 1 0871 Yes +5°C ± 3°C 79 ! Y0000359 Acebutolol impurity B 2 10 mg 1 -[3-acetyl-4-[(2RS)-2-hydroxy-3-[(1-methylethyl)amino] propoxy]phenyl] 0871 Yes +5°C ± 3°C 79 ! acetamide (diacetolol) Y0000127 Acebutolol impurity C 1 20 mg 1 N-(3-acetyl-4-hydroxyphenyl)butanamide 0871 Yes +5°C ± 3°C 79 ! Y0000128 Acebutolol impurity I 2 0.004 mg 1 N-[3-acetyl-4-[(2RS)-3-(ethylamino)-2-hydroxypropoxy]phenyl] 0871 Yes +5°C ± 3°C 79 ! butanamide Y0000056 Aceclofenac - reference spectrum 1 n/a 1 1281 79 ! Y0000085 Aceclofenac impurity F 2 15 mg 1 benzyl[[[2-[(2,6-dichlorophenyl)amino]phenyl]acetyl]oxy]acetate -
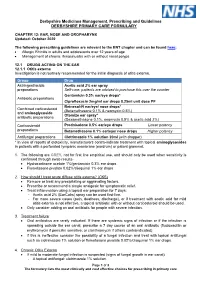
EAR, NOSE and OROPHARYNX Updated: October 2020
Derbyshire Medicines Management, Prescribing and Guidelines DERBYSHIRE PRIMARY CARE FORMULARY CHAPTER 12: EAR, NOSE AND OROPHARYNX Updated: October 2020 The following prescribing guidelines are relevant to the ENT chapter and can be found here: • Allergic Rhinitis in adults and adolescents over 12 years of age • Management of chronic rhinosinusitis with or without nasal polyps 12.1 DRUGS ACTING ON THE EAR 12.1.1 Otitis externa Investigation is not routinely recommended for the initial diagnosis of otitis externa. Group Drug Astringent/acidic Acetic acid 2% ear spray preparations Self-care: patients are advised to purchase this over the counter Gentamicin 0.3% ear/eye drops* Antibiotic preparations Ciprofloxacin 2mg/ml ear drops 0.25ml unit dose PF Betnesol-N ear/eye/ nose drops* Combined corticosteroid (Betamethasone 0.1% & neomycin 0.5%) and aminoglycoside Otomize ear spray* antibiotic preparations (Dexamethasone 0.1%, neomycin 0.5% & acetic acid 2%) Corticosteroid Prednisolone 0.5% ear/eye drops Lower potency preparations Betamethasone 0.1% ear/eye/ nose drops Higher potency Antifungal preparations Clotrimazole 1% solution 20ml (with dropper) * In view of reports of ototoxicity, manufacturers contra-indicate treatment with topical aminoglycosides in patients with a perforated tympanic membrane (eardrum) or patent grommet. 1. The following are GREY, not for first line empirical use, and should only be used when sensitivity is confirmed through swab results- • Hydrocortisone acetate 1%/gentamicin 0.3% ear drops • Flumetasone pivalate 0.02%/clioquinol 1% ear drops 2. How should I treat acute diffuse otitis externa? (CKS) • Remove or treat any precipitating or aggravating factors. • Prescribe or recommend a simple analgesic for symptomatic relief. -

Ear, Nose and Oral Cavity
NHS Borders Joint Prescribing Formulary Ear, nose, and oral cavity Black Text Drugs which may be prescribed by all prescribers Drugs which are either for specialist only prescription or for specialist Pink Text initiation, with prescribing transfer to GP Important Information: In addition to the disclaimer on NHS Borders website the following information is included confirming that the information contained in NHS Borders Joint Prescribing formulary is drawn from several sources, including BNF & BNF for children, product SPCs, local and national guidelines, local expert opinion, Lothian Joint Formulary and these are all gratefully acknowledged here. NHS Borders has done its utmost to ensure the information in the BJF is accurate and reliable, but NHS Borders cannot guarantee that the information is complete and accurate. Prescribers are referred to the SPCs, BNF and BNF for children to confirm prescribing information. June 2021 Contents Page Table of Contents 12.1 Drugs acting on the ear ................................................................................................ 3 Otitis externa ................................................................................................................ 3 Otitis media .................................................................................................................. 3 Removal of ear wax ..................................................................................................... 3 12.2 Drugs acting on the nose ............................................................................................ -

Preventing Hearing Loss Caused by Chemical (Ototoxicity) and Noise Exposure
Preventing Hearing Loss Caused by Chemical (Ototoxicity) and Noise Exposure Safety and Health Information Bulletin SHIB 03-08-2018 DHHS (NIOSH) Publication No. 2018-124 Introduction Millions of workers are exposed to noise in the workplace every day and when uncontrolled, noise exposure may cause permanent hearing loss. Research demonstrates exposure to certain chemicals, called ototoxicants, may cause hearing loss or balance problems, regardless of noise exposure. Substances including certain pesticides, solvents, and pharmaceuticals that contain ototoxicants can negatively affect how the ear functions, causing hearing loss, and/or affect balance. Source/Copyright: OSHA The risk of hearing loss is increased when workers are exposed to these chemicals while working around elevated noise levels. This combination often results in hearing loss that can be temporary or permanent, depending on the level of noise, the dose of the chemical, and the duration of the exposure. This hearing impairment affects many occupations and industries, from machinists to firefighters. Effects on Hearing Harmful exposure to ototoxicants may occur through inhalation, ingestion, or skin absorption. Health effects caused by ototoxic chemicals vary based on exposure frequency, intensity, duration, workplace exposure to other hazards, and individual factors such as age. Effects may be temporary or permanent, can affect hearing sensitivity and result in a standard threshold shift. Since chemicals can affect central portions of the auditory system (e.g., nerves or nuclei in the central nervous system, the pathways to the brain or in the brain itself), not only do sounds need to be louder to be detected, but also they lose clarity. Specifically, speech discrimination dysfunction, the ability to hear voices separately from background noise, may occur and involve: . -

Differential Diagnosis and Treatment of Hearing Loss JON E
Differential Diagnosis and Treatment of Hearing Loss JON E. ISAACSON, M.D., and NEIL M. VORA, M.D., Milton S. Hershey Medical Center, Hershey, Pennsylvania Hearing loss is a common problem that can occur at any age and makes verbal communication difficult. The ear is divided anatomically into three sections (external, middle, and inner), and pathology contributing to hearing loss may strike one or more sections. Hearing loss can be cat- egorized as conductive, sensorineural, or both. Leading causes of conductive hearing loss include cerumen impaction, otitis media, and otosclerosis. Leading causes of sensorineural hear- ing loss include inherited disorders, noise exposure, and presbycusis. An understanding of the indications for medical management, surgical treatment, and amplification can help the family physician provide more effective care for these patients. (Am Fam Physician 2003;68:1125-32. Copyright© 2003 American Academy of Family Physicians) ore than 28 million Amer- tive, the sound will be heard best in the icans have some degree of affected ear. If the loss is sensorineural, the hearing impairment. The sound will be heard best in the normal ear. differential diagnosis of The sound remains midline in patients with hearing loss can be sim- normal hearing. Mplified by considering the three major cate- The Rinne test compares air conduction gories of loss. Conductive hearing loss occurs with bone conduction. The tuning fork is when sound conduction is impeded through struck softly and placed on the mastoid bone the external ear, the middle ear, or both. Sen- (bone conduction). When the patient no sorineural hearing loss occurs when there is a longer can hear the sound, the tuning fork is problem within the cochlea or the neural placed adjacent to the ear canal (air conduc- pathway to the auditory cortex. -

Parallel Import (PI) Licences Granted in May 2017
Parallel import (PI) licences granted in May 2017 PL Number Grant Date Licence Holder Licensed Name(s) Active Ingredient Quantity Units Legal Status* PLPI 15184/1699 03/05/2017 LEXON (UK) LIMITED TIMOPTOL UNIT DOSE 0.25% W/V EYE DROPS SOLUTION TIMOLOL 2.5 MILLIGRAMMES PER MILLILITRE POM PLPI 15184/1700 03/05/2017 LEXON (UK) LIMITED TIMOPTOL UNIT DOSE 0.5% W/V EYE DROPS SOLUTION TIMOLOL 0.5 MILLIGRAMMES PER MILLILITRE POM PLPI 16369/1716 03/05/2017 G-PHARMA LIMITED CELIPROLOL HYDROCHLORIDE 200MG TABLETS CELIPROLOL HYDROCHLORIDE 200.000 MILLIGRAMMES POM PLPI 21828/0717 03/05/2017 LANDMARK PHARMA LIMITED LEVOCARNITINE PAEDIATRIC 30% ORAL SOLUTION LEVOCARNITINE 30.00 PERCENT WEIGHT IN VOLUME POM PLPI 33532/0768 03/05/2017 MPT PHARMA LIMITED COLESTYRAMINE SUGAR FREE 4G-SACHET COLESTYRAMINE 4.000 GRAMMES POM PLPI 33532/0768 03/05/2017 MPT PHARMA LIMITED QUESTRAN LIGHT 4G-SACHET POWDER FOR ORAL SUSPENSION COLESTYRAMINE 4.000 GRAMMES POM PLPI 33532/0778 03/05/2017 MPT PHARMA LIMITED SERETIDE 500 ACCUHALER FLUTICASONE PROPIONATE 500.00 MICROGRAMMES POM PLPI 33532/0778 03/05/2017 MPT PHARMA LIMITED SERETIDE 500 ACCUHALER SALMETEROL XINAFOATE 0.0725 MILLIGRAMMES POM PLPI 33532/0779 03/05/2017 MPT PHARMA LIMITED TRIMIPRAMINE 25MG FILM-COATED TABLETS TRIMIPRAMINE MALEATE 34.9 MILLIGRAMMES POM PLPI 39352/0376 03/05/2017 KOSEI PHARMA UK LIMITED DESMOPRESSIN ACETATE 0.1MG TABLETS DESMOPRESSIN ACETATE 0.1 MILLIGRAMMES POM PLPI 39352/0377 03/05/2017 KOSEI PHARMA UK LIMITED FLUMETASONE PIVALATE/CLIOQUINOL 0.02% W/V / 1% W/V EAR DROPS SOLUTION CLIOQUINOL -

Medicines Formulary
MEDICINES FORMULARY Medicines formulary between MCHFT and Primary Care as agreed by the Joint Medicines Management Group Welcome to the MCHFT Medicines Formulary. The formulary includes medicines that have been approved by the Joint Medicines Management Group (JMMG) for prescribing within the trust. The purpose of the formulary is to ensure prescribing is evidence based and cost effective. All prescribing within the trust (i.e. inpatient, outpatient and FP10HNC prescribing) must comply with the formulary. This will be monitored on a regular basis. Some drugs may appear in more than one section. Information on prescribing in primary care is available via the Medicines Management Team website: http://www.centralandeasterncheshiremmt.nhs.uk This is a good point of reference to confirm the continuation of medicines in primary care after initiation at MCHFT. The formulary is arranged in sections corresponding to those in the British National Formulary (BNF) as below; INTRODUCTION .......................................................................................................................................... 2 UPDATES TO THE FORMULARY (LAST UPDATED MAY 2019)............................................................... 4 1. GASTRO-INTESTINAL SYSTEM ............................................................................................................. 7 2. CARDIOVASCULAR SYSTEM .............................................................................................................. 11 3. RESPIRATORY SYSTEM ..................................................................................................................... -

Why Is Drug-Induced Ototoxicity Still Not Preventable Nor Is It Treatable in 2019? - a Literature Review of Aminoglycoside and Cisplatin Ototoxicity Cherrabi Kaoutar*
Review Article iMedPub Journals Archives of Medicine 2020 www.imedpub.com Vol.12 No.2:3 ISSN 1989-5216 DOI: 10.36648/1989-5216.12.2.304 Why is Drug-Induced Ototoxicity Still Not Preventable nor is it Treatable in 2019? - A Literature Review of Aminoglycoside and Cisplatin Ototoxicity Cherrabi Kaoutar* Department of Oto-Rhino-Laryngology and Cervico-Facial Studies, Fez, Morocco *Corresponding author: Cherrabi Kaoutar, Resident, Department of Oto-Rhino-Laryngology and Cervico-Facial Studies, Fez, Morocco, Tel: 0679382957; E-mail: [email protected] Received date: October 17, 2019; Accepted date: March 02, 2019; Published date: March 09, 2020 Citation: Cherrabi K (2020) Why is Drug-Induced Ototoxicity Still Not Preventable nor is it Treatable in 2019? - A Literature Review of Aminoglycoside and Cisplatin Ototoxicity. Arch Med Vol: 12 Iss: 2:3 Copyright: ©2020 Cherrabi K. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. The thorough exploration of inner ear proteome, transcriptome, and genome in physiological and Abstract pathological contexts as potential biomarkers of early stages of cell lesions: The clinical application would not Oto-toxicity is defined by cochlear and or vestibular only allow a more specific understanding of different cellular lesions due to the use of drugs. The difference in mechanisms of iatrogenic oto-toxicity, but also allow new specific mechanisms, the great semi logical variability, the insights into targeted protective and post-lesional heterogeneity of incriminated drugs, the inaccessibility to therapies.