An LC/MS-MS Screening Method for Synthetic Glucocorticoids Based on Pharmacological Structure-Activity Relationships
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(CD-P-PH/PHO) Report Classification/Justifica
COMMITTEE OF EXPERTS ON THE CLASSIFICATION OF MEDICINES AS REGARDS THEIR SUPPLY (CD-P-PH/PHO) Report classification/justification of medicines belonging to the ATC group D07A (Corticosteroids, Plain) Table of Contents Page INTRODUCTION 4 DISCLAIMER 6 GLOSSARY OF TERMS USED IN THIS DOCUMENT 7 ACTIVE SUBSTANCES Methylprednisolone (ATC: D07AA01) 8 Hydrocortisone (ATC: D07AA02) 9 Prednisolone (ATC: D07AA03) 11 Clobetasone (ATC: D07AB01) 13 Hydrocortisone butyrate (ATC: D07AB02) 16 Flumetasone (ATC: D07AB03) 18 Fluocortin (ATC: D07AB04) 21 Fluperolone (ATC: D07AB05) 22 Fluorometholone (ATC: D07AB06) 23 Fluprednidene (ATC: D07AB07) 24 Desonide (ATC: D07AB08) 25 Triamcinolone (ATC: D07AB09) 27 Alclometasone (ATC: D07AB10) 29 Hydrocortisone buteprate (ATC: D07AB11) 31 Dexamethasone (ATC: D07AB19) 32 Clocortolone (ATC: D07AB21) 34 Combinations of Corticosteroids (ATC: D07AB30) 35 Betamethasone (ATC: D07AC01) 36 Fluclorolone (ATC: D07AC02) 39 Desoximetasone (ATC: D07AC03) 40 Fluocinolone Acetonide (ATC: D07AC04) 43 Fluocortolone (ATC: D07AC05) 46 2 Diflucortolone (ATC: D07AC06) 47 Fludroxycortide (ATC: D07AC07) 50 Fluocinonide (ATC: D07AC08) 51 Budesonide (ATC: D07AC09) 54 Diflorasone (ATC: D07AC10) 55 Amcinonide (ATC: D07AC11) 56 Halometasone (ATC: D07AC12) 57 Mometasone (ATC: D07AC13) 58 Methylprednisolone Aceponate (ATC: D07AC14) 62 Beclometasone (ATC: D07AC15) 65 Hydrocortisone Aceponate (ATC: D07AC16) 68 Fluticasone (ATC: D07AC17) 69 Prednicarbate (ATC: D07AC18) 73 Difluprednate (ATC: D07AC19) 76 Ulobetasol (ATC: D07AC21) 77 Clobetasol (ATC: D07AD01) 78 Halcinonide (ATC: D07AD02) 81 LIST OF AUTHORS 82 3 INTRODUCTION The availability of medicines with or without a medical prescription has implications on patient safety, accessibility of medicines to patients and responsible management of healthcare expenditure. The decision on prescription status and related supply conditions is a core competency of national health authorities. -

Etats Rapides
List of European Pharmacopoeia Reference Standards Effective from 2015/12/24 Order Reference Standard Batch n° Quantity Sale Information Monograph Leaflet Storage Price Code per vial Unit Y0001756 Exemestane for system suitability 1 10 mg 1 2766 Yes +5°C ± 3°C 79 ! Y0001561 Abacavir sulfate 1 20 mg 1 2589 Yes +5°C ± 3°C 79 ! Y0001552 Abacavir for peak identification 1 10 mg 1 2589 Yes +5°C ± 3°C 79 ! Y0001551 Abacavir for system suitability 1 10 mg 1 2589 Yes +5°C ± 3°C 79 ! Y0000055 Acamprosate calcium - reference spectrum 1 n/a 1 1585 79 ! Y0000116 Acamprosate impurity A 1 50 mg 1 3-aminopropane-1-sulphonic acid 1585 Yes +5°C ± 3°C 79 ! Y0000500 Acarbose 3 100 mg 1 See leaflet ; Batch 2 is valid until 31 August 2015 2089 Yes +5°C ± 3°C 79 ! Y0000354 Acarbose for identification 1 10 mg 1 2089 Yes +5°C ± 3°C 79 ! Y0000427 Acarbose for peak identification 3 20 mg 1 Batch 2 is valid until 31 January 2015 2089 Yes +5°C ± 3°C 79 ! A0040000 Acebutolol hydrochloride 1 50 mg 1 0871 Yes +5°C ± 3°C 79 ! Y0000359 Acebutolol impurity B 2 10 mg 1 -[3-acetyl-4-[(2RS)-2-hydroxy-3-[(1-methylethyl)amino] propoxy]phenyl] 0871 Yes +5°C ± 3°C 79 ! acetamide (diacetolol) Y0000127 Acebutolol impurity C 1 20 mg 1 N-(3-acetyl-4-hydroxyphenyl)butanamide 0871 Yes +5°C ± 3°C 79 ! Y0000128 Acebutolol impurity I 2 0.004 mg 1 N-[3-acetyl-4-[(2RS)-3-(ethylamino)-2-hydroxypropoxy]phenyl] 0871 Yes +5°C ± 3°C 79 ! butanamide Y0000056 Aceclofenac - reference spectrum 1 n/a 1 1281 79 ! Y0000085 Aceclofenac impurity F 2 15 mg 1 benzyl[[[2-[(2,6-dichlorophenyl)amino]phenyl]acetyl]oxy]acetate -
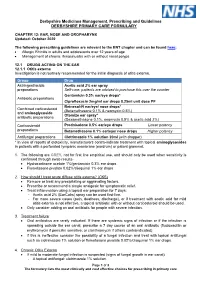
EAR, NOSE and OROPHARYNX Updated: October 2020
Derbyshire Medicines Management, Prescribing and Guidelines DERBYSHIRE PRIMARY CARE FORMULARY CHAPTER 12: EAR, NOSE AND OROPHARYNX Updated: October 2020 The following prescribing guidelines are relevant to the ENT chapter and can be found here: • Allergic Rhinitis in adults and adolescents over 12 years of age • Management of chronic rhinosinusitis with or without nasal polyps 12.1 DRUGS ACTING ON THE EAR 12.1.1 Otitis externa Investigation is not routinely recommended for the initial diagnosis of otitis externa. Group Drug Astringent/acidic Acetic acid 2% ear spray preparations Self-care: patients are advised to purchase this over the counter Gentamicin 0.3% ear/eye drops* Antibiotic preparations Ciprofloxacin 2mg/ml ear drops 0.25ml unit dose PF Betnesol-N ear/eye/ nose drops* Combined corticosteroid (Betamethasone 0.1% & neomycin 0.5%) and aminoglycoside Otomize ear spray* antibiotic preparations (Dexamethasone 0.1%, neomycin 0.5% & acetic acid 2%) Corticosteroid Prednisolone 0.5% ear/eye drops Lower potency preparations Betamethasone 0.1% ear/eye/ nose drops Higher potency Antifungal preparations Clotrimazole 1% solution 20ml (with dropper) * In view of reports of ototoxicity, manufacturers contra-indicate treatment with topical aminoglycosides in patients with a perforated tympanic membrane (eardrum) or patent grommet. 1. The following are GREY, not for first line empirical use, and should only be used when sensitivity is confirmed through swab results- • Hydrocortisone acetate 1%/gentamicin 0.3% ear drops • Flumetasone pivalate 0.02%/clioquinol 1% ear drops 2. How should I treat acute diffuse otitis externa? (CKS) • Remove or treat any precipitating or aggravating factors. • Prescribe or recommend a simple analgesic for symptomatic relief. -

Ear, Nose and Oral Cavity
NHS Borders Joint Prescribing Formulary Ear, nose, and oral cavity Black Text Drugs which may be prescribed by all prescribers Drugs which are either for specialist only prescription or for specialist Pink Text initiation, with prescribing transfer to GP Important Information: In addition to the disclaimer on NHS Borders website the following information is included confirming that the information contained in NHS Borders Joint Prescribing formulary is drawn from several sources, including BNF & BNF for children, product SPCs, local and national guidelines, local expert opinion, Lothian Joint Formulary and these are all gratefully acknowledged here. NHS Borders has done its utmost to ensure the information in the BJF is accurate and reliable, but NHS Borders cannot guarantee that the information is complete and accurate. Prescribers are referred to the SPCs, BNF and BNF for children to confirm prescribing information. June 2021 Contents Page Table of Contents 12.1 Drugs acting on the ear ................................................................................................ 3 Otitis externa ................................................................................................................ 3 Otitis media .................................................................................................................. 3 Removal of ear wax ..................................................................................................... 3 12.2 Drugs acting on the nose ............................................................................................ -

Parallel Import (PI) Licences Granted in May 2017
Parallel import (PI) licences granted in May 2017 PL Number Grant Date Licence Holder Licensed Name(s) Active Ingredient Quantity Units Legal Status* PLPI 15184/1699 03/05/2017 LEXON (UK) LIMITED TIMOPTOL UNIT DOSE 0.25% W/V EYE DROPS SOLUTION TIMOLOL 2.5 MILLIGRAMMES PER MILLILITRE POM PLPI 15184/1700 03/05/2017 LEXON (UK) LIMITED TIMOPTOL UNIT DOSE 0.5% W/V EYE DROPS SOLUTION TIMOLOL 0.5 MILLIGRAMMES PER MILLILITRE POM PLPI 16369/1716 03/05/2017 G-PHARMA LIMITED CELIPROLOL HYDROCHLORIDE 200MG TABLETS CELIPROLOL HYDROCHLORIDE 200.000 MILLIGRAMMES POM PLPI 21828/0717 03/05/2017 LANDMARK PHARMA LIMITED LEVOCARNITINE PAEDIATRIC 30% ORAL SOLUTION LEVOCARNITINE 30.00 PERCENT WEIGHT IN VOLUME POM PLPI 33532/0768 03/05/2017 MPT PHARMA LIMITED COLESTYRAMINE SUGAR FREE 4G-SACHET COLESTYRAMINE 4.000 GRAMMES POM PLPI 33532/0768 03/05/2017 MPT PHARMA LIMITED QUESTRAN LIGHT 4G-SACHET POWDER FOR ORAL SUSPENSION COLESTYRAMINE 4.000 GRAMMES POM PLPI 33532/0778 03/05/2017 MPT PHARMA LIMITED SERETIDE 500 ACCUHALER FLUTICASONE PROPIONATE 500.00 MICROGRAMMES POM PLPI 33532/0778 03/05/2017 MPT PHARMA LIMITED SERETIDE 500 ACCUHALER SALMETEROL XINAFOATE 0.0725 MILLIGRAMMES POM PLPI 33532/0779 03/05/2017 MPT PHARMA LIMITED TRIMIPRAMINE 25MG FILM-COATED TABLETS TRIMIPRAMINE MALEATE 34.9 MILLIGRAMMES POM PLPI 39352/0376 03/05/2017 KOSEI PHARMA UK LIMITED DESMOPRESSIN ACETATE 0.1MG TABLETS DESMOPRESSIN ACETATE 0.1 MILLIGRAMMES POM PLPI 39352/0377 03/05/2017 KOSEI PHARMA UK LIMITED FLUMETASONE PIVALATE/CLIOQUINOL 0.02% W/V / 1% W/V EAR DROPS SOLUTION CLIOQUINOL -

Medicines Formulary
MEDICINES FORMULARY Medicines formulary between MCHFT and Primary Care as agreed by the Joint Medicines Management Group Welcome to the MCHFT Medicines Formulary. The formulary includes medicines that have been approved by the Joint Medicines Management Group (JMMG) for prescribing within the trust. The purpose of the formulary is to ensure prescribing is evidence based and cost effective. All prescribing within the trust (i.e. inpatient, outpatient and FP10HNC prescribing) must comply with the formulary. This will be monitored on a regular basis. Some drugs may appear in more than one section. Information on prescribing in primary care is available via the Medicines Management Team website: http://www.centralandeasterncheshiremmt.nhs.uk This is a good point of reference to confirm the continuation of medicines in primary care after initiation at MCHFT. The formulary is arranged in sections corresponding to those in the British National Formulary (BNF) as below; INTRODUCTION .......................................................................................................................................... 2 UPDATES TO THE FORMULARY (LAST UPDATED MAY 2019)............................................................... 4 1. GASTRO-INTESTINAL SYSTEM ............................................................................................................. 7 2. CARDIOVASCULAR SYSTEM .............................................................................................................. 11 3. RESPIRATORY SYSTEM ..................................................................................................................... -

Connectivity Map-Based Discovery of Parbendazole Reveals Targetable Human Osteogenic Pathway
Connectivity Map-based discovery of parbendazole reveals targetable human osteogenic pathway Andrea M. Bruma, Jeroen van de Peppela, Cindy S. van der Leijea, Marijke Schreuders-Koedama, Marco Eijkenb, Bram C. J. van der Eerdena, and Johannes P. T. M. van Leeuwena,1 aDepartment of Internal Medicine, Erasmus MC, 3015 CN Rotterdam, The Netherlands; and bArcarios BV, 3015 CN Rotterdam, The Netherlands Edited by John T. Potts, Massachusetts General Hospital, Charlestown, MA, and approved September 4, 2015 (received for review January 26, 2015) Osteoporosis is a common skeletal disorder characterized by low molecules to a user’s selected gene signature of the phenotype bone mass leading to increased bone fragility and fracture suscepti- of interest using a pattern-matching algorithm with a high level bility. In this study, we have identified pathways that stimulate of resolution and specificity. The screening results in a list of differentiation of bone forming osteoblasts from human mesenchy- compounds with a highly correlating gene expression pattern to mal stromal cells (hMSCs). Gene expression profiling was performed that of the phenotype of interest, which has the potential to aid in hMSCs differentiated toward osteoblasts (at 6 h). Significantly in finding a novel treatment for a disease or to identify novel regulated genes were analyzed in silico, and the Connectivity Map pathways or genes involved in a complex biological process. To (CMap) was used to identify candidate bone stimulatory com- date, the CMap has been successfully used to identify compounds pounds. The signature of parbendazole matches the expression and combination therapies that show promise in the treatment of changes observed for osteogenic hMSCs. -

Vr Meds Ex01 3B 0825S Coding Manual Supplement Page 1
vr_meds_ex01_3b_0825s Coding Manual Supplement MEDNAME OTHER_CODE ATC_CODE SYSTEM THER_GP PHRM_GP CHEM_GP SODIUM FLUORIDE A12CD01 A01AA01 A A01 A01A A01AA SODIUM MONOFLUOROPHOSPHATE A12CD02 A01AA02 A A01 A01A A01AA HYDROGEN PEROXIDE D08AX01 A01AB02 A A01 A01A A01AB HYDROGEN PEROXIDE S02AA06 A01AB02 A A01 A01A A01AB CHLORHEXIDINE B05CA02 A01AB03 A A01 A01A A01AB CHLORHEXIDINE D08AC02 A01AB03 A A01 A01A A01AB CHLORHEXIDINE D09AA12 A01AB03 A A01 A01A A01AB CHLORHEXIDINE R02AA05 A01AB03 A A01 A01A A01AB CHLORHEXIDINE S01AX09 A01AB03 A A01 A01A A01AB CHLORHEXIDINE S02AA09 A01AB03 A A01 A01A A01AB CHLORHEXIDINE S03AA04 A01AB03 A A01 A01A A01AB AMPHOTERICIN B A07AA07 A01AB04 A A01 A01A A01AB AMPHOTERICIN B G01AA03 A01AB04 A A01 A01A A01AB AMPHOTERICIN B J02AA01 A01AB04 A A01 A01A A01AB POLYNOXYLIN D01AE05 A01AB05 A A01 A01A A01AB OXYQUINOLINE D08AH03 A01AB07 A A01 A01A A01AB OXYQUINOLINE G01AC30 A01AB07 A A01 A01A A01AB OXYQUINOLINE R02AA14 A01AB07 A A01 A01A A01AB NEOMYCIN A07AA01 A01AB08 A A01 A01A A01AB NEOMYCIN B05CA09 A01AB08 A A01 A01A A01AB NEOMYCIN D06AX04 A01AB08 A A01 A01A A01AB NEOMYCIN J01GB05 A01AB08 A A01 A01A A01AB NEOMYCIN R02AB01 A01AB08 A A01 A01A A01AB NEOMYCIN S01AA03 A01AB08 A A01 A01A A01AB NEOMYCIN S02AA07 A01AB08 A A01 A01A A01AB NEOMYCIN S03AA01 A01AB08 A A01 A01A A01AB MICONAZOLE A07AC01 A01AB09 A A01 A01A A01AB MICONAZOLE D01AC02 A01AB09 A A01 A01A A01AB MICONAZOLE G01AF04 A01AB09 A A01 A01A A01AB MICONAZOLE J02AB01 A01AB09 A A01 A01A A01AB MICONAZOLE S02AA13 A01AB09 A A01 A01A A01AB NATAMYCIN A07AA03 A01AB10 A A01 -

EUROPEAN PHARMACOPOEIA 10.0 Index 1. General Notices
EUROPEAN PHARMACOPOEIA 10.0 Index 1. General notices......................................................................... 3 2.2.66. Detection and measurement of radioactivity........... 119 2.1. Apparatus ............................................................................. 15 2.2.7. Optical rotation................................................................ 26 2.1.1. Droppers ........................................................................... 15 2.2.8. Viscosity ............................................................................ 27 2.1.2. Comparative table of porosity of sintered-glass filters.. 15 2.2.9. Capillary viscometer method ......................................... 27 2.1.3. Ultraviolet ray lamps for analytical purposes............... 15 2.3. Identification...................................................................... 129 2.1.4. Sieves ................................................................................. 16 2.3.1. Identification reactions of ions and functional 2.1.5. Tubes for comparative tests ............................................ 17 groups ...................................................................................... 129 2.1.6. Gas detector tubes............................................................ 17 2.3.2. Identification of fatty oils by thin-layer 2.2. Physical and physico-chemical methods.......................... 21 chromatography...................................................................... 132 2.2.1. Clarity and degree of opalescence of -

3.2.1 Safety of Antibiotic Ear Drops in Children with Grommets
Safety of antibiotic ear drops in children with grommets CONFIDENTIAL Medicines Adverse Reactions Committee Meeting date 8 June 2017 Agenda item 3.2.1 Title Safety of Antibiotic Ear Drops in children with Grommets Medsafe Pharmacovigilance Submitted by Paper type For advice Team Active constituent(s) Medicines Sponsors Clioquinol; Locorten-Vioform AFT Pharmaceuticals Flumetasone pivalate Locacorten-Viaform Ciprofloxacin; Pharmaco (NZ) Ltd Ciproxin HC Otic Ear drops Hydrocortisone Framycetin; Sanofi-aventis New Zealand limited Gramicidin; Sofradex Dexamethasone Framycetin Soframycin Sanofi-aventis New Zealand limited Neomycin; Pharmacy Retailing (NZ) Ltd t/a Gramicidin; Kenacomb Ear drops Healthcare Logistics Nystatin; Triamcinolone Funding Locorten-Vioform/Locacorten-Viaform; Kenacomb; Sofradex*; Soframycin*. *Part funded only Previous MARC None meetings International action None Prescriber Update None Schedule Prescription Advice sought The Committee is asked to advise whether: − there is evidence of a difference in the risk of ototoxicity between the antibiotic containing ear drops when used in children with grommets or in patients with a perforated tympanic membrane − the sponsor for Ciproxin HC (quinolone) ear drops should be given the opportunity to remove the contraindication for use in patients with a perforated tympanic membrane and replace it with a warning statement − the sponsor for Locorten-Vioform/Locacorten-Viaform (hydroxyquinolone) include information on the risk of ototoxicity − the sponsors for Sofradex, Soframycin and -

Atopic Dermatitis (1 of 13)
Atopic Dermatitis (1 of 13) 1 Patient presents w/ skin manifestations suggestive of atopic dermatitis 2 DIAGNOSIS No ALTERNATIVE Do history & physical exam DIAGNOSIS confirm atopic dermatitis? Yes Patient suff ers from acute fl are-up Patient suff ers from disease of pruritus & inflammation persistence or frequent recurrences ACUTE FLAREUP TREATMENT MAINTENANCE TREATMENT A Non-pharmacological therapy A Non-pharmacological therapy • Patient/caregiver education • Same as acute fl are-up • Avoidance of trigger factors • Investigate precipitating factors of each fl are-up • Skin care • Phototherapy* - Bathing B Pharmacological therapy - Moisturizers/emollients Start at earliest sign of local recurrence: - Wet dressing • Calcineurin inhibitor (topical) B Pharmacological therapy or Any one of the following agents: Long-term: • Corticosteroid (topical) • Calcineurin inhibitor (topical), combined w/ • Calcineurin inhibitor (topical) • Corticosteroids (topical), intermittent use If skin infection is present: If skin infection is present: • Appropriate antibiotics, antifungals, • Antibiotics, antifungals, antivirals (oral &/or topical) antivirals (oral &/or topical) Symptomatic relief of pruritus: Symptomatic relief of pruritus: • Antihistamine (oral) • Antihistamine (oral) MIMS • • Continue Expert referral is recommended • non- Psychotherapeutic/ pharmacological psychopharmacological options therapy may be combined w/ the therapies EVALUATION listed below • Discontinue Yes No Disease A topical Non-pharmacological therapy remission (Severe • Continue therapy above corticosteroid &/ Refractory • Phototherapy or calcineurin Atopic B inhibitor Dermatitis) Pharmacological therapy • Potent corticosteroids (topical) © • Systemic corticosteroids • Systemic immunosuppressants *May be considered in patients >6 years of age w/ Scoring of Atopic Dermatitis (SCORAD) score of 25-50. Not all products are available or approved for above use in all countries. Specifi c prescribing information may be found in the latest MIMS. -

Stembook 2018.Pdf
The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 WHO/EMP/RHT/TSN/2018.1 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances. Geneva: World Health Organization; 2018 (WHO/EMP/RHT/TSN/2018.1). Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data.