Atopic Dermatitis (1 of 13)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(CD-P-PH/PHO) Report Classification/Justifica
COMMITTEE OF EXPERTS ON THE CLASSIFICATION OF MEDICINES AS REGARDS THEIR SUPPLY (CD-P-PH/PHO) Report classification/justification of medicines belonging to the ATC group D07A (Corticosteroids, Plain) Table of Contents Page INTRODUCTION 4 DISCLAIMER 6 GLOSSARY OF TERMS USED IN THIS DOCUMENT 7 ACTIVE SUBSTANCES Methylprednisolone (ATC: D07AA01) 8 Hydrocortisone (ATC: D07AA02) 9 Prednisolone (ATC: D07AA03) 11 Clobetasone (ATC: D07AB01) 13 Hydrocortisone butyrate (ATC: D07AB02) 16 Flumetasone (ATC: D07AB03) 18 Fluocortin (ATC: D07AB04) 21 Fluperolone (ATC: D07AB05) 22 Fluorometholone (ATC: D07AB06) 23 Fluprednidene (ATC: D07AB07) 24 Desonide (ATC: D07AB08) 25 Triamcinolone (ATC: D07AB09) 27 Alclometasone (ATC: D07AB10) 29 Hydrocortisone buteprate (ATC: D07AB11) 31 Dexamethasone (ATC: D07AB19) 32 Clocortolone (ATC: D07AB21) 34 Combinations of Corticosteroids (ATC: D07AB30) 35 Betamethasone (ATC: D07AC01) 36 Fluclorolone (ATC: D07AC02) 39 Desoximetasone (ATC: D07AC03) 40 Fluocinolone Acetonide (ATC: D07AC04) 43 Fluocortolone (ATC: D07AC05) 46 2 Diflucortolone (ATC: D07AC06) 47 Fludroxycortide (ATC: D07AC07) 50 Fluocinonide (ATC: D07AC08) 51 Budesonide (ATC: D07AC09) 54 Diflorasone (ATC: D07AC10) 55 Amcinonide (ATC: D07AC11) 56 Halometasone (ATC: D07AC12) 57 Mometasone (ATC: D07AC13) 58 Methylprednisolone Aceponate (ATC: D07AC14) 62 Beclometasone (ATC: D07AC15) 65 Hydrocortisone Aceponate (ATC: D07AC16) 68 Fluticasone (ATC: D07AC17) 69 Prednicarbate (ATC: D07AC18) 73 Difluprednate (ATC: D07AC19) 76 Ulobetasol (ATC: D07AC21) 77 Clobetasol (ATC: D07AD01) 78 Halcinonide (ATC: D07AD02) 81 LIST OF AUTHORS 82 3 INTRODUCTION The availability of medicines with or without a medical prescription has implications on patient safety, accessibility of medicines to patients and responsible management of healthcare expenditure. The decision on prescription status and related supply conditions is a core competency of national health authorities. -

PRODUCT MONOGRAPH MYLAN-CLOBETASOL SCALP APPLICATION (Clobetasol 17-Propionate 0.05% W/W in Aqueous-Alcohol Base) (60 Ml Bottles
PRODUCT MONOGRAPH MYLAN-CLOBETASOL SCALP APPLICATION (Clobetasol 17-propionate 0.05% w/w in aqueous-alcohol base) (60 ml bottles) Topical Corticosteroid Mylan Pharmaceuticals ULC DATE OF PREPARATION: 85 Advance Road Etobicoke, June 5, 2009 Ontario M8Z 2S6 DATE OF REVISION: Control#: 129665 NAME OF DRUG MYLAN-CLOBETASOL SCALP APPLICATION (Clobetasol 17-propionate 0.05 %w/w) (60 mL bottles) THERAPEUTIC CLASSIFICATION Topical Corticosteroid ACTIONS AND CLINICAL PHARMACOLOGY MYLAN-CLOBETASOL SCALP APPLICATION (Clobetasol 17-propionate) is a very potent topical corticosteroid with anti-inflammatory, antipruritic, and vasoconstrictive actions. Pharmacokinetics In man, the extent of percutaneous absorption of topical corticosteroids, including clobetasol 17-propionate, is determined by many factors, including the vehicle, the integrity of the epidermal barrier, and the use of occlusive dressing. As with all topical corticosteroids, clobetasol 17-propionate can be absorbed from normal intact skin. Inflammation and/or other disease processes in the skin may increase percutaneous absorption. Occlusive dressings substantially increase the percutaneous absorption of topical corticosteroids. 2 Once absorbed through the skin, topical corticosteroids enter pharmacokinetic pathways similar to systemically administered corticosteroids. Corticosteroids are bound to plasma proteins in varying degrees. Corticosteroids are metabolized primarily in the liver and are then excreted by the kidneys. Some of the topical corticosteroids, including clobetasol 17-propionate and its metabolites, are also excreted in the bile. Bioavailability The relative potency of corticosteroids is usually assayed by the vasoconstriction test which reflects the potency of the steroid molecule, its topical activity as well as its bioavailaility from the particular formulation. The vascoconstrictor response of MYLAN-CLOBETASOL SCALP APPLICATION was compared with Dermovate Scalp Application as well as a placebo in a randomised and double blind study involving twelve healthy subjects. -

Etats Rapides
List of European Pharmacopoeia Reference Standards Effective from 2015/12/24 Order Reference Standard Batch n° Quantity Sale Information Monograph Leaflet Storage Price Code per vial Unit Y0001756 Exemestane for system suitability 1 10 mg 1 2766 Yes +5°C ± 3°C 79 ! Y0001561 Abacavir sulfate 1 20 mg 1 2589 Yes +5°C ± 3°C 79 ! Y0001552 Abacavir for peak identification 1 10 mg 1 2589 Yes +5°C ± 3°C 79 ! Y0001551 Abacavir for system suitability 1 10 mg 1 2589 Yes +5°C ± 3°C 79 ! Y0000055 Acamprosate calcium - reference spectrum 1 n/a 1 1585 79 ! Y0000116 Acamprosate impurity A 1 50 mg 1 3-aminopropane-1-sulphonic acid 1585 Yes +5°C ± 3°C 79 ! Y0000500 Acarbose 3 100 mg 1 See leaflet ; Batch 2 is valid until 31 August 2015 2089 Yes +5°C ± 3°C 79 ! Y0000354 Acarbose for identification 1 10 mg 1 2089 Yes +5°C ± 3°C 79 ! Y0000427 Acarbose for peak identification 3 20 mg 1 Batch 2 is valid until 31 January 2015 2089 Yes +5°C ± 3°C 79 ! A0040000 Acebutolol hydrochloride 1 50 mg 1 0871 Yes +5°C ± 3°C 79 ! Y0000359 Acebutolol impurity B 2 10 mg 1 -[3-acetyl-4-[(2RS)-2-hydroxy-3-[(1-methylethyl)amino] propoxy]phenyl] 0871 Yes +5°C ± 3°C 79 ! acetamide (diacetolol) Y0000127 Acebutolol impurity C 1 20 mg 1 N-(3-acetyl-4-hydroxyphenyl)butanamide 0871 Yes +5°C ± 3°C 79 ! Y0000128 Acebutolol impurity I 2 0.004 mg 1 N-[3-acetyl-4-[(2RS)-3-(ethylamino)-2-hydroxypropoxy]phenyl] 0871 Yes +5°C ± 3°C 79 ! butanamide Y0000056 Aceclofenac - reference spectrum 1 n/a 1 1281 79 ! Y0000085 Aceclofenac impurity F 2 15 mg 1 benzyl[[[2-[(2,6-dichlorophenyl)amino]phenyl]acetyl]oxy]acetate -
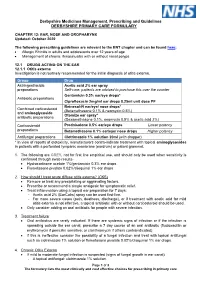
EAR, NOSE and OROPHARYNX Updated: October 2020
Derbyshire Medicines Management, Prescribing and Guidelines DERBYSHIRE PRIMARY CARE FORMULARY CHAPTER 12: EAR, NOSE AND OROPHARYNX Updated: October 2020 The following prescribing guidelines are relevant to the ENT chapter and can be found here: • Allergic Rhinitis in adults and adolescents over 12 years of age • Management of chronic rhinosinusitis with or without nasal polyps 12.1 DRUGS ACTING ON THE EAR 12.1.1 Otitis externa Investigation is not routinely recommended for the initial diagnosis of otitis externa. Group Drug Astringent/acidic Acetic acid 2% ear spray preparations Self-care: patients are advised to purchase this over the counter Gentamicin 0.3% ear/eye drops* Antibiotic preparations Ciprofloxacin 2mg/ml ear drops 0.25ml unit dose PF Betnesol-N ear/eye/ nose drops* Combined corticosteroid (Betamethasone 0.1% & neomycin 0.5%) and aminoglycoside Otomize ear spray* antibiotic preparations (Dexamethasone 0.1%, neomycin 0.5% & acetic acid 2%) Corticosteroid Prednisolone 0.5% ear/eye drops Lower potency preparations Betamethasone 0.1% ear/eye/ nose drops Higher potency Antifungal preparations Clotrimazole 1% solution 20ml (with dropper) * In view of reports of ototoxicity, manufacturers contra-indicate treatment with topical aminoglycosides in patients with a perforated tympanic membrane (eardrum) or patent grommet. 1. The following are GREY, not for first line empirical use, and should only be used when sensitivity is confirmed through swab results- • Hydrocortisone acetate 1%/gentamicin 0.3% ear drops • Flumetasone pivalate 0.02%/clioquinol 1% ear drops 2. How should I treat acute diffuse otitis externa? (CKS) • Remove or treat any precipitating or aggravating factors. • Prescribe or recommend a simple analgesic for symptomatic relief. -

Ear, Nose and Oral Cavity
NHS Borders Joint Prescribing Formulary Ear, nose, and oral cavity Black Text Drugs which may be prescribed by all prescribers Drugs which are either for specialist only prescription or for specialist Pink Text initiation, with prescribing transfer to GP Important Information: In addition to the disclaimer on NHS Borders website the following information is included confirming that the information contained in NHS Borders Joint Prescribing formulary is drawn from several sources, including BNF & BNF for children, product SPCs, local and national guidelines, local expert opinion, Lothian Joint Formulary and these are all gratefully acknowledged here. NHS Borders has done its utmost to ensure the information in the BJF is accurate and reliable, but NHS Borders cannot guarantee that the information is complete and accurate. Prescribers are referred to the SPCs, BNF and BNF for children to confirm prescribing information. June 2021 Contents Page Table of Contents 12.1 Drugs acting on the ear ................................................................................................ 3 Otitis externa ................................................................................................................ 3 Otitis media .................................................................................................................. 3 Removal of ear wax ..................................................................................................... 3 12.2 Drugs acting on the nose ............................................................................................ -

Parallel Import (PI) Licences Granted in May 2017
Parallel import (PI) licences granted in May 2017 PL Number Grant Date Licence Holder Licensed Name(s) Active Ingredient Quantity Units Legal Status* PLPI 15184/1699 03/05/2017 LEXON (UK) LIMITED TIMOPTOL UNIT DOSE 0.25% W/V EYE DROPS SOLUTION TIMOLOL 2.5 MILLIGRAMMES PER MILLILITRE POM PLPI 15184/1700 03/05/2017 LEXON (UK) LIMITED TIMOPTOL UNIT DOSE 0.5% W/V EYE DROPS SOLUTION TIMOLOL 0.5 MILLIGRAMMES PER MILLILITRE POM PLPI 16369/1716 03/05/2017 G-PHARMA LIMITED CELIPROLOL HYDROCHLORIDE 200MG TABLETS CELIPROLOL HYDROCHLORIDE 200.000 MILLIGRAMMES POM PLPI 21828/0717 03/05/2017 LANDMARK PHARMA LIMITED LEVOCARNITINE PAEDIATRIC 30% ORAL SOLUTION LEVOCARNITINE 30.00 PERCENT WEIGHT IN VOLUME POM PLPI 33532/0768 03/05/2017 MPT PHARMA LIMITED COLESTYRAMINE SUGAR FREE 4G-SACHET COLESTYRAMINE 4.000 GRAMMES POM PLPI 33532/0768 03/05/2017 MPT PHARMA LIMITED QUESTRAN LIGHT 4G-SACHET POWDER FOR ORAL SUSPENSION COLESTYRAMINE 4.000 GRAMMES POM PLPI 33532/0778 03/05/2017 MPT PHARMA LIMITED SERETIDE 500 ACCUHALER FLUTICASONE PROPIONATE 500.00 MICROGRAMMES POM PLPI 33532/0778 03/05/2017 MPT PHARMA LIMITED SERETIDE 500 ACCUHALER SALMETEROL XINAFOATE 0.0725 MILLIGRAMMES POM PLPI 33532/0779 03/05/2017 MPT PHARMA LIMITED TRIMIPRAMINE 25MG FILM-COATED TABLETS TRIMIPRAMINE MALEATE 34.9 MILLIGRAMMES POM PLPI 39352/0376 03/05/2017 KOSEI PHARMA UK LIMITED DESMOPRESSIN ACETATE 0.1MG TABLETS DESMOPRESSIN ACETATE 0.1 MILLIGRAMMES POM PLPI 39352/0377 03/05/2017 KOSEI PHARMA UK LIMITED FLUMETASONE PIVALATE/CLIOQUINOL 0.02% W/V / 1% W/V EAR DROPS SOLUTION CLIOQUINOL -

Medicines Formulary
MEDICINES FORMULARY Medicines formulary between MCHFT and Primary Care as agreed by the Joint Medicines Management Group Welcome to the MCHFT Medicines Formulary. The formulary includes medicines that have been approved by the Joint Medicines Management Group (JMMG) for prescribing within the trust. The purpose of the formulary is to ensure prescribing is evidence based and cost effective. All prescribing within the trust (i.e. inpatient, outpatient and FP10HNC prescribing) must comply with the formulary. This will be monitored on a regular basis. Some drugs may appear in more than one section. Information on prescribing in primary care is available via the Medicines Management Team website: http://www.centralandeasterncheshiremmt.nhs.uk This is a good point of reference to confirm the continuation of medicines in primary care after initiation at MCHFT. The formulary is arranged in sections corresponding to those in the British National Formulary (BNF) as below; INTRODUCTION .......................................................................................................................................... 2 UPDATES TO THE FORMULARY (LAST UPDATED MAY 2019)............................................................... 4 1. GASTRO-INTESTINAL SYSTEM ............................................................................................................. 7 2. CARDIOVASCULAR SYSTEM .............................................................................................................. 11 3. RESPIRATORY SYSTEM ..................................................................................................................... -

An LC/MS-MS Screening Method for Synthetic Glucocorticoids Based on Pharmacological Structure-Activity Relationships
In: W Schänzer, H Geyer, A Gotzmann, U Mareck (eds.) Recent Advances In Doping Analysis (14). Sport und Buch Strauß - Köln 2006 Monica Mazzarino, Maria Cristina Braganò, Francesco Botrè An LC/MS-MS screening method for synthetic glucocorticoids based on pharmacological structure-activity relationships Laboratorio Antidoping, Federazione Medico-Sportiva Italiana, Roma, Italy INTRODUCTION The last few years have shown a remarkable evolution of the approach utilized at an international level to control the abuse of drugs in sport. A series of preventive actions have been put in place by the World Anti-Doping Agency (WADA) to deter the illicit use of performance-enhancing agents. These actions are complementary to the traditional activity of the anti-doping laboratories, which remains a key component of any effective anti-doping policy. At the same time, there has been recent discovery of “designer steroids” [1-2] and, more generally, other previously unknown substances endowed with pharmacologically properties, specifically designed and synthesized with the aim of improving sport performance without the risk of being caught through anti-doping control. This has resulted in a more or less pronounced revision of analytical screening protocols to allow also the detection of those novel “designer drugs”. These compounds were not originally included in the WADA prohibited list, the international reference document detailing all the substances and methods forbidden for use by athletes [3]. This situation has led to the development of alternative analytical methods capable of detecting the presence of one or more drugs in human urine belonging to the same class of congeners, based on the recognition of common portions of the molecular structure. -

Efficacy and Safety of Halometasone Cream to Treat Chronic Generalized Eczema and the Effects of Halometasone Cream on Serum Cortisol Levels
Hindawi BioMed Research International Volume 2017, Article ID 3265024, 7 pages https://doi.org/10.1155/2017/3265024 Clinical Study Efficacy and Safety of Halometasone Cream to Treat Chronic Generalized Eczema and the Effects of Halometasone Cream on Serum Cortisol Levels Yan Li, Wei Xu, and Linfeng Li Department of Dermatology, Beijing Friendship Hospital, Capital Medical University, Beijing 100050, China Correspondence should be addressed to Wei Xu; [email protected] Received 19 August 2017; Accepted 19 October 2017; Published 9 November 2017 Academic Editor: Fabio Sonvico Copyright © 2017 Yan Li et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. The aim of the study was to investigate the efficacy and safety ofhalometasone cream to treat chronic generalized eczema and the effects of halometasone cream on serum cortisol (COR) levels. Sixty consecutive outpatients diagnosed with chronic generalized eczema between January and April 2017 were included and divided into groups A, B, and C with a lesion area of 30%–40%, 41%–50%, and51%–60%,respectively.GroupsA,B,andCweretreatedwithhalometasonecreamwithadailydoseof15g,20g,and30gfor 7–14 days, respectively. Ten patients were randomly selected from each group for serum COR measurement at days 0, 7, and 14. On day 14, group B had significantly higher cure rate (47.1%)than groups A (17.9%)and C (13.3%) and significantly higher effectiveness rate (82.4%) than group C (40.0%) (all < 0.05). Serum COR levels were not affected in group A but were reduced significantly in groups B and C on days 7 and 14 (all < 0.05). -

BODY LOTIONS/CREAMS and HOMOEOPATHY © Dr
BODY LOTIONS/CREAMS AND HOMOEOPATHY © Dr. Rajneesh Kumar Sharma M.D. (Homoeopathy) Homoeo Cure & Research Centre P. Ltd. NH 74, Moradabad Road, Kashipur (Uttaranchal) INDIA, Pin- 244713 Ph. 05947- 260327, 9897618594 [email protected], [email protected] Definition There are two types of body lotions and creams- 1- Moisturizers, lubricants or softening ones. 2- Cleansing ones. 1- Body lotions and creams are the cosmetic emollient substances, which when applied to skin, protect it from loss of moisture, lubricating and softening dead keratin, thereby lowering the rate at which water evaporates from the skin surface, acting similarly to the natural sebum, secreted by sebaceous glands of the skin. 2- Cleansing creams and lotions are detergent-based or emulsified oil systems that are designed primarily for the removal of surface oil, pollutants, or cellular debris along with makeup. History Perfumed oils About 3100–2907 BC, during the First empire of Egypt, men and women used perfumed oils, stored in unguent jars made of alabaster and marble, to maintain soft, supple, and unwrinkled skin. Face pack By the middle of the first century AD, Romans used a face pack of barley-bean flour, egg, and mashed narcissus bulbs to promote smooth skin. Cold cream A Greek physician of the second century AD invented cold cream containing water, beeswax, and olive oil. When rubbed on the face, the water evaporated, cooling the skin. (Cold cream formulations of the 1920s were of similar composition.) Oiled packs By 1700, smooth skin was in fashion and women applied oiled cloths on their foreheads and wore gloves in bed to prevent wrinkles. -
EL 04-85-GC1 a Study to Define a Set of Requirements for Cleansing Agents for Use in the Space Station Whole Body Shower
FINAL REPORT NAS 9-17428 - EL 04-85-GC1 A Study To Define A Set of Requirements For Cleansing Agents For Use in the Space Station Whole Body Shower. October 29, 1985 _ , MT.X \t> )> C ^ ^>'- N86-16903 S final Unclas 05 ml HC A05/WF A01 ECONOMICS LABORATORY. INC. Osborn Building St. Paul, Minnesota 55102 INDEX CONTENTS PAGE Introduction Final Report 1-26 Table #1 - Foam Test Results Table #2 - Shampoo Ingredient Comparisons Appendix A - Database References Appendix B - Dermal Sensitization Study Appendix C - Eye Irritation Study Appendix D - Protocol For Comparing Shampoos Appendix E - Detergent Filming Build Up Study Figure 1 - Whole Body Portable Shower Head Unit Page 2 October 25, 1985 NAS 9-17428 - EL 04-85-GC1 INTRODUCTION The purpose of this contract is to assist NASA engineers in defining a set of requirements for a whole body cleansing agent to be used in the Space Station Whole Body Shower System. In addition, cleansing agent candidates are to be identified that are likely to satisfy requirements defined in the first part of the study. It is understood that the main reason for having a Whole Body Shower is to satisfy the physiological, psychological and social needs of the crew throughout the duration of duty in ^ the Space Station. The cleansing agent must also be compatible with the vortex water/gas separator and the water reclamation system. To accomplish these goals the study was divided into six tasks. These tasks are as follows: 1. Task One: Survey literature and unpublished information to ascertain state-of-the-art in Whole Body Shower cleansing and the potential impacts of extended use of WBS cleansing agents in a mic'rogravity environment. -

Dermatological Conditions
18 Dermatological Conditions JAMES E. LESSENGER Key words: predisposing factors, patch testing, wood’s light, urticarian, dermatitis Skin problems in worldwide agricultural workers are very common. Among California grape and tomato harvesters, pustular eruptions such as acne and fol- liculitis were present in 30% of studied workers. Irritant or allergic contact der- matitis was present in 2%. In Iowa, 9.6% of male farmers and 14.4% of wives of farmers reported dermatitis during the previous 12-month period. In Washington State, researchers studied 7445 claims for occupational skin disorders filed over a 5-year period. Medical bills totaled $1.22 million, and lost time payments were $1.23 million. The highest rates of occupational skin disorder claims were seen in agriculture with 2.8 claims per 10,000 full-time equivalent employee years. Most of these skin disorders were due to chemical and vegetation exposures (1–4). Among northern Ecuadorian potato farm workers, high rates of dermatitis and pigmentation disorders were attributable to the use of pesticides and fungi- cides. Among California farm workers, skin disease rates were found in tomato workers (6.2%), citrus (10.8%), and vineyard workers (21.0%). Factors found to contribute to dermatitis in farm workers included the specific type of crop cul- tivated, specific job activity, use of personal protective measures, field and home sanitation, environmental conditions of heat and humidity, personal hygiene, allergic history (including atopy), and ethnicity. Several pesticides were shown to cause irritant and allergic contact dermatitis. Causes were found to include pes- ticides, naturally occurring plant substances, heat, sunlight and humidity, atopy, and infectious fungal and bacterial agents (5,6).