GETZ-Guidelines Suppl
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Shia Target Killing Report
PAKISTAN 31/12/2012 Shaheed Detail in January 2012 Name Date City Reason Nisar Ahmed s/o Sardar Muhammad 18-Jan-12 Quetta Gun Shot Ghulam Muhammad s/o Ghulam Ali 16-Jan-12 Karachi Gun Shot Ghulam Raza 15-Jan-12 Karachi Gun Shot S. Mushtaq Zaidi 12-Jan-12 Karachi Gun Shot Kalb-e-Abbas Rizvi 9-Jan-12 Karachi Gun Shot Dr Jamal 7-Jan-12 Peshawar Gun Shot ASI Ghullam Abbas 5-Jan-12 Quetta Target killing Mushkoor Hussain 5-Jan-12 Lahore Target killing DSP Ibrahim 4-Jan-12 Gilgit Target killing Ghulam Abbas 15-Jan-12 Khanpur Bome Blast Faiz Hussain 15-Jan-12 Khanpur Bome Blast Abad Hussain 15-Jan-12 Khanpur Bome Blast Zahid Abbas 15-Jan-12 Khanpur Bome Blast Asad Abbas 15-Jan-12 Khanpur Bome Blast Mureed Hussain 15-Jan-12 Khanpur Bome Blast Akhter Hussain 15-Jan-12 Khanpur Bome Blast Mohammed Ashaq 15-Jan-12 Khanpur Bome Blast Khezhar Hayat 15-Jan-12 Khanpur Bome Blast Amjad Hussain 15-Jan-12 Khanpur Bome Blast Sadam Hussain 15-Jan-12 Khanpur Bome Blast Abad Hussain 15-Jan-12 Khanpur Bome Blast Aatif 15-Jan-12 Khanpur Bome Blast Adnan 15-Jan-12 Khanpur Bome Blast Faisal Hayat 15-Jan-12 Khanpur Bome Blast Tahir Abbas 15-Jan-12 Khanpur Bome Blast Syed Hussain 15-Jan-12 Khanpur Bome Blast Qurban Hussian 15-Jan-12 Khanpur Bome Blast Ghulam Qadir 17-Jan-12 Khanpur Bome Blast Shahnawaz 17-Jan-12 Khanpur Bome Blast Ali Hussain s/o Muzaffar Abbas 22-Jan-12 Karachi Target killing Asghar Karrar 19-Jan-12 Karachi Target killing Dr. -

Presentations by National Speakers
PRESENTATIONS By National Speakers Pak J Med Sci 2016 www.pjms.com.pk Special Supplement Abstract Book IDEC August 2016 49 34- Shall we be treating all women with HRT? Hormone replacement therapies, Metabolic and cardiovascular effects. Prof. A.H. Aamir Consultant Endocrinologist, Professor of Medicines, Head of Department of Endocrinology, Hayatabad Medical Complex, Peshawar. Menopause affects every woman and it usually occurs at a median age of 51 years. As large number of women is reaching midlife, it is likely that physicians will come across a stage where HRT may need to be considered for their patient. Menopause has Physical, Psychological, Uro-genital tract, Cardiovascular, Skeletal effects. Estrogens also have effects on carbohydrate homeostasis, fatty liver and atherosclerosis. Postmenopausal women with hyper-androgenemia have elevated risks for NIDDM-Risk and CHD. Most of these effects are reversible with replacement of Estrogens. Women health initiative study (WHI) initially showed an increased cardiovascular risk with HRT increased risk of VTE, stroke, MI Risk appears to be higher in initial years of treatment, followed by decline in risk. Recent re-analyses of WHI results suggested that the association between HRT and cardiovascular risk is influenced by factors such as age and time since menopause • Reduced CV risk in women <10 years post-menopause. • WHI population included older women with other CV risk factors. Risks of stroke should be balanced against benefits, such as decreased risk of hip fracture. Treatment with HRT needs to be individualized in the light of recent International menopausal society recommendations. 50 Pak J Med Sci 2016 www.pjms.com.pk Special Supplement Abstract Book IDEC August 2016 35- Characteristics of Fasting and Ramadan-specific diabetes education trends in people with diabetes (CARE) Prof. -

List of Gold Medal Winners
LIST OF GOLD MEDAL WINNERS FIRST POSITION IN PAKISTAN S. NO. ROLL NO. STUDENT NAME FATHER NAME CLASS INSTITUTION ADDRESS CITY/DISTRICT STREET NO. 18, BLOCK-B, KAZIMABAD, 1 16-021-00372-1-011-E AAYAN BASHIR KAMRAN BASHIR 1 BEACON ASKARI O LEVEL SCHOOL KARACHI MODEL COLONY THE CITY SCHOOL HAYATABAD HOUSE NO. 33-34, STREET NO. 01, 2 16-91-00763-1-033-E ABBAS ALI KHAN WALI KHAN 1 PESHAWAR JUNIOR SECTOR K - 5, PHASE - 3, HAYATABAD 3 16-42-00816-1-008-E ABDUL HAYEE SHAHZAD RAO SHAHZAD QAMAR 1 BEACONHOUSE SCHOOL SYSTEM HOUSE NO. 41 - A1, PECO ROAD LAHORE HEAVY INDUSTORIES TAXILA 4 16-51-00703-1-021-E ABDUL REHMAN MUHAMMAD RIAZ 1 HITEC PRE SCHOOL RAWALPINDI EDUCATION CITY, KHANPUR ROAD 5 16-41-00186-1-004-E ABDUL SAMAD BILAL BILAL QAYYUM PURI 1 LEARNING ALLIANCE 1 - AMIR TOWN EAST CANAL ROAD FAISALABAD THE CITY SCHOOL HAYATABAD HOUSE NO. 33-34, STREET NO. 01, 6 16-91-00763-1-036-E ABDULLAH MUHAMMAD NISAR MUHAMMAD 1 PESHAWAR JUNIOR SECTOR K - 5, PHASE - 3, HAYATABAD THE CITY SCHOOL RISALPUR HOUSE NO. 3/10, MEHMOOD ROAD, 7 16-923-00652-1-001-E ABDULLAH SHAHID SHAHID RIAZ 1 NOWSHERA CAMPUS RISALPUR CANTT DEFENCE HOUSING AUTHORITY 8 16-42-20026-1-005-E ABDULLAH ZAHEER ZAHEER ALI 1 970-K, SECTOR-Z, PHASE-3, DHA CANTT LAHORE JUNIOR CAMPUS STREET NO. 18, BLOCK-B, KAZIMABAD, 9 16-021-00372-1-063-E ABEERA ASIF ASIF PERVEZ 1 BEACON ASKARI O LEVEL SCHOOL KARACHI MODEL COLONY THE CITY SCHOOL WAPDA TOWN 10 16-42-00613-1-004-E ABEERA NASIR NASIR HAMEED 1 HOUSE NO. -

Winter-Mtg-Jounral-2017-Online.Pdf
Civic Engagement Through Community Service APPNA Association of Physicians of Pakistani Descent of North America 6414 South Cass Avenue, Westmont, IL 60559-3209, USA APPNA Winter Meeting 2017 December 21-23, 2017 Lahore, Pakistan Editorial This year we are celebrating 40th anniversary of APPNA, in these last 40 years our association has morphed into one of the largest ethnic professional society of North America representing over 18000 Pakistan-decent medical graduates from its small humble beginning with just a handful members attending its first meeting in 1976. With every passing year, with every new challenge, opportunity or adversity APPNA has developed even more resilience just like our nation when it comes to dealing with these challenges. Over the years APPNA has taken upon several daunting tasks depending upon the need of the time and strategic vision of its leader. However, no matter who is leading the organization, what kind of political environment or government exit, whenever a calamity hit, APPNA with all the collective strength of its member is always at the forefront of fighting the adversity, regardless if it is in our motherland or adoptive home. Some of the recent examples of excellent relief work APPNA and its members did include help of Tsunami victims in Southeast Asia (2004), Katrina victims in New Orleans, USA and earthquake victims in Pakistan (2005), victims of Sindh Floods (2007) and Pakistan Flood (2010), Thur water well project, Several Free clinics throughout United States, National Health Care Day, Corneal transplants, Fistula surgeries and Cleft Palate surgeries. As a Pakistani medical graduate immigrating to USA, one APPNA characteristic I cherish the most is the platform it has provided to people like myself who want to give back to our motherland and serve their adopted communities. -

S. No. Folio No. Security Holder Name Father's/Husband's Name Address
Askari Bank Limited List of Shareholders without / invalid CNIC # as of 31-12-2019 S. Folio No. Security Holder Name Father's/Husband's Name Address No. of No. Securities 1 9 MR. MOHAMMAD SAEED KHAN S/O MR. MOHAMMAD WAZIR KHAN 65, SCHOOL ROAD, F-7/4, ISLAMABAD. 336 2 10 MR. SHAHID HAFIZ AZMI S/O MR. MOHD ABDUL HAFEEZ 17/1 6TH GIZRI LANE, DEFENCE HOUSING AUTHORITY, PHASE-4, KARACHI. 3,280 3 15 MR. SALEEM MIAN S/O MURTUZA MIAN 344/7, ROSHAN MANSION, THATHAI COMPOUND, M.A. JINNAH ROAD, KARACHI. 439 4 21 MS. HINA SHEHZAD MR. HAMID HUSSAIN C/O MUHAMMAD ASIF THE BUREWALA TEXTILE MILLS LTD 1ST FLOOR, DAWOOD CENTRE, M.T. KHAN ROAD, P.O. 10426, KARACHI. 470 5 42 MR. M. RAFIQUE S/O A. RAHIM B.R.1/27, 1ST FLOOR, JAFFRY CHOWK, KHARADHAR, KARACHI. 9,382 6 49 MR. JAN MOHAMMED S/O GHULAM QADDIR KHAN H.NO. M.B.6-1728/733, RASHIDABAD, BILDIA TOWN, MAHAJIR CAMP, KARACHI. 557 7 55 MR. RAFIQ UR REHMAN S/O MOHD NASRULLAH KHAN PSIB PRIVATE LIMITED, 17-B, PAK CHAMBERS, WEST WHARF ROAD, KARACHI. 305 8 57 MR. MUHAMMAD SHUAIB AKHUNZADA S/O FAZAL-I-MAHMOOD 262, SHAMI ROAD, PESHAWAR CANTT. 1,919 9 64 MR. TAUHEED JAN S/O ABDUR REHMAN KHAN ROOM NO.435, BLOCK-A, PAK SECRETARIAT, ISLAMABAD. 8,530 10 66 MS. NAUREEN FAROOQ KHAN SARDAR M. FAROOQ IBRAHIM 90, MARGALA ROAD, F-8/2, ISLAMABAD. 5,945 11 67 MR. ERSHAD AHMED JAN S/O KH. -

15.04.2021 Seniority List of Bs-20 Officers of The
SENIORITY LIST OF BS-20 OFFICERS OF THE PAKISTAN AUDIT AND ACCOUNTS SERVICE AS ON 15.04.2021 15.04.2021 Date of entry Present Date of Superannua In PA&AS In present S # Name CTP Domicile in govt. Present Posting Station Posting Birth tion /B-17 scale. service w.e.f 1 Muhammad Ajmal Gondal 14 Punjab 10-Oct-61 10-Oct-21 14-Nov-87 14-Nov-87 29-Oct-20 Member (Finance), PAEC Islamabad 02.11.2020 2 Farrukh Ahmad Hamidi 14 Sindh (U) 30-May-62 30-May-22 01-Nov-86 01-Nov-86 09-Dec-19 Controller General of Accounts, Islamabad Islamabad 05-Mar-21 Secretary, National Food Security & Research Division, 3 Abdul Ghufran Memon 15 Sindh (R) 11-Jun-65 11-Jun-25 14-Nov-87 14-Nov-87 16-Jul-20 Islamabad 11-Nov-20 Islamabad 4 Ghulam Muhammad Memon 15 Sindh (R) 26-Mar-63 26-Mar-23 13-Jan-88 25-Jul-95 18-Aug-20 Additional AGP-I, AGP Office Islamabad 11-Mar-21 1 Shahid Gul Qureshi 13 Punjab 17-May-61 17-May-21 22-Oct-85 22-Oct-85 25-Feb-17 Member (Finance), NESCOM Islamabad 29-Oct-18 Deputy Auditor General (Defence Audit), AGP Office, 2 Abdul Hameed Pasha 15 KP 20-Feb-62 20-Feb-22 03-May-86 14-Nov-87 28-Jan-19 Islamabad 15-Sep-20 Islamabad 3 Niaz Ahmad Sheikh 15 Sindh (R) 25-Oct-63 25-Oct-23 06-Jun-88 31-Oct-92 26-Jun-19 Deputy Auditor General (South) Karachi 22-Aug-19 4 Sajid Ali Nadeem 16 Punjab 15-Apr-66 15-Apr-26 01-Nov-88 01-Nov-88 29-Jan-19 Deputy Auditor General (Central), Lahore Lahore 22-Feb-21 5 Muhammad Nasir Ali 16 Punjab 13-May-64 13-May-24 07-Dec-87 01-Nov-88 28-Jan-19 Rector, PAAA, Lahore Lahore 19-Feb-21 6 Masood Akhtar Sherwanee 16 Punjab 14-Dec-61 14-Dec-21 01-Nov-88 01-Nov-88 28-Jan-19 Deputy Auditor General (Policy), AGP Office, Islamabad Islamabad 01-Mar-21 7 Fareed Mahmood Ch. -
Telephone Numbers of the Audit & Accounts Offices.Pdf
TELEPHONE NUMBERS OF AUDIT & ACCOUNTS OFFICES AS ON 17-07-2019 Compiled by: Muhammad Saleem, SPS to AGP [email protected] AUDITOR-GENERAL OF PAKISTAN Audit House, Constitution Avenue, G-5/2 Sector, Islamabad Web Site : www.agp.gov.pk EXCH : 9224150-65 Email : [email protected] M/s NAME DESIGNATION I.No. OFFICE RES. FAX Javaid Jehangir Auditor-General of 301 9224080 9216688 9225243 Pakistan 9212527 FAX Muhammad Saleem SPS to Auditor-General 337 9224080 0300 – 5065832 9225243 Shan Afsar APS 338 9212254 0312 – 5611675 Nasir Hayat CA to Auditor General 338 9212254 0333 – 1583333 Abdul Moiz Rao Protocol Officer to AGP 366 9221401 0333 – 5382908 Muhammad Kashif Dir to AGP 405 9216632 0300 – 6351466 Muhammad Aasim PA to Dir 354 9216632 0331 – 5479042 Naeem Nasir AAO to Dir 354 9216632 0332 – 5306095 Farrukh Ahmad Hamidi Addl. Auditor-General – I 305 9219161 0300-9493901 9207924 Abbasi sb SPS to Addl. AGP-I 352 9219161 0345-5241988 9207924 Jehanzeb PA 352 9219161 0345-2009113 Muhammad Jamil Addl. Auditor General – II 312 9224082 0345-5036770 9214530 Afaqi Aziz ur Rehman SPS to Addl.AGP-II 351 9224082 0333-5387537 9214530 Waqar Ali Channer APS 0333-5077653 Mahfooz Ahmed Bhatti Focal Person / Official 339 9215955 0300-2188091 Spokesperson of DAGP Dr. Arshad Mahmood Addl.FS(Expenditure) / 9202576 External Auditor on AGP Administration & Coordination Wing Dost Ali Shah Dy. Ar. General 303 9224081 0334-6641818 9201678 Gulzar Ahmed Bhutta SPS to DAG (A&C) 340 9224081 0303-5143304 -- Hasnain APS 0333-5254208 Zulfiqar Khan Dir (Admin) 423 9224083 0336-5079561 9212134- Ehsan Ellahi APS to Dir (Admin) 374 9224083 0334-7227068 Musaddiq Shah APS to Dir (Admin) 0301-8767707 Andrew John Cooper AO (Confidential) 353 9219682 0333-5612347 Fahad Rehman Khan AO (Confidential) 402 9203511 0344-5900030 Anees Ahmed AAO (Confidential) 402 9203511 0334-5033022 Khawar Abbas AO (Confidential) 353 9219682 0334-1548909 9219682 Muhammad Safeer AAO (Confidential) 353 9219682 Asim Naeem AAO (Confidential) 353 9203511 0312-5252542 M. -
Texas Medical Board
Texas Medical Board TOTAL APPLICANTS FOR CONSIDERATION FOR BOARD MEETING OF JUNE 1, 2010 PERMANENT LICENSURE M.D.'S D.O.'S UK TOTAL GRADUATES OF: TEXAS MEDICAL SCHOOLS 185 22 0 207 CANADIAN MEDICAL SCHOOLS 1 0 0 1 OUT-OF-STATE MEDICAL 282 39 0 321 SCHOOLS FOREIGN MEDICAL SCHOOLS 166 0 0 166 GRAND TOTAL 633 61 695 LICENSE TYPE AND METHOD: ADMINISTRATIVE MEDICINE REGULAR 0 0 0 0 RELICENSURE 0 0 0 0 REINSTATEMENT 0 0 0 0 TOTAL: 0 0 0 0 CONCEDED EMINENCE REGULAR 0 0 0 0 RELICENSURE 0 0 0 0 REINSTATEMENT 0 0 0 0 TOTAL: 0 0 0 0 FULL REGULAR 611 59 0 670 RELICENSURE 9 1 0 10 REINSTATEMENT 1 0 0 1 TOTAL: 620 60 0 681 PUBLIC HEALTH REGULAR 0 0 0 0 RELICENSURE 0 0 0 0 REINSTATEMENT 0 0 0 0 TOTAL: 0 0 0 0 TELEMEDICINE REGULAR 13 1 0 14 RELICENSURE 0 0 0 0 REINSTATEMENT 0 0 0 0 TOTAL: 13 1 0 14 GRAND TOTAL 634 61 695 Note See agenda Item 2a and 2b for 3 other applicants granted unrestricted licenses and 1 applicant granted a telemedicine license, and 2c for 7 orders offered by the ED and accepted . New Total 705 TEXAS MEDICAL BOARD FULL LICENSURE APPLICANTS FOR CONSIDERATION AT JUNE, 2010 BOARD MEETING 1. AL-HINDI, AHMAD MD FULL-REG (548762) SCHOOL: JORDAN UNIV OF SCIENCE & TECHNOLOGY, FACULTY OF MEDICINE, IRBID-1991 2. ABDELFATTAH, KAREEM REDA MD FULL-REG (527145) SCHOOL: UNIV OF SOUTH FLORIDA COLL OF MED, TAMPA-2007 3. -
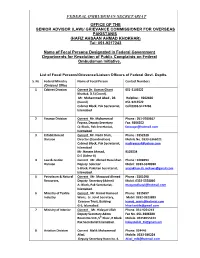
List of Focal Persons Appointed in Pakistan Missions for Instant Resolution of Public Complaints Against Federal
FEDERAL OMBUDSMAN SECRETARIAT OFFICE OF THE SENIOR ADVISOR (LAW)/ GRIEVANCE COMMISSIONER FOR OVERSEAS PAKISTANIS (HAFIZ AHSAAN AHMAD KHOKHAR) Tel: 051-9217243 Name of Focal Persons Designated in Federal Government Departments for Resolution of Public Complaints on Federal Ombudsman Initiative. List of Focal Persons/Grievance/Liaison Officers of Federal Govt. Deptts. S. No Federal Ministry Name of Focal Person Contact Numbers /Division/ Office 1 Cabinet Division Current Dr. Usman Ghani 051-9103522 Khattak, D.S (Coord). Mr. Muhammad Ahad , DS Helpline : 9202666 (Coord) 051-9213522 Cabinet Block, Pak Secretariat, Cell:0333-5172266 Islamabad 2 Finance Division Current Mr. Mohammad Phone : 051-9209567 Fayyaz, Deputy Secretary Fax. 9206552 Q- Block, Pak Secretariat, [email protected] Islamabad 3 Establishment Current Mr. Nadir Shah, Phone : 9252328 Division Director (Coordination) Mobile No. 0333-5366021 Cabinet Block, Pak Secretariat, [email protected] Islamabad Mr. Naseer Ahmad, 9103534 D.S (Admn-II) 4 Law & Justice Current Mr. Ahmed Raza khan Phone : 9208994 Division Deputy Solicitor Mobil: 0333-5528030 S-Block, Pakistan Secretariat, [email protected] Islamabad. 5 Petroleum & Natural Current Mr. Maqsood Ahmed Phone : 9201098 Resources, Deputy Secretary (Admn) Mobil: 0333-5558866 A- Block, Pak Secretariat, [email protected] Islamabad. 6 Ministry of Textile Current Mr. Hamid Hameed Phone: 9215657 Industry Waris, Sr. Joint Secretary, Mobil: 0332-0323889 Evacuee Trust, Building [email protected] G-5, Islamabad. [email protected] 7 Ministry of Interior Current Mr. Hidayat Ullah Phone. 051-9201213 Deputy Secretary Admn Fax No. 051-9206380 Room No.514 ,5th Floor, R Block Mobile. 03458555224 Pak Secretariat Islamabad. [email protected] 8 Aviation Division Current Malik Muhammad Phone: 924446 Afzal, Mobile: 0333-560224 Deputy Secretary Room No. -

Dr. Rajwali Khan
DR. RAJWALI KHAN Designation: Assistant Professor, Department of Livestock Management, Breeding and Genetics, The University of Agriculture Peshawar Pakistan, Cell No. 0092 300 901 8065; [email protected] Domicile: Peshawar Nationality: Pakistani Religion: Islam CNIC # 17301-7717418-1 Passport # BM4134182 Marital status: Married Date of birth: April 1985 Current post: Assistant Professor BPS-19 Employer: The University of Agriculture Peshawar-Pakistan Permanent address: Village Choli Payan P.O Dag Distt: Peshawar Professional qualification: Degree University Passing Year Field of Study Ph. D Northwest A&F University, Yangling, 2020 Animal Science Shaanxi, China M. Sc (Hons) The University of Agriculture Peshawar 2010 Animal Science Gold Medal Pakistan DVM Sind Agriculture University, Tando 2008 Animal Husbandry Jam. &Veterinary Sciences WORKING EXPERIENCE Designation Department From To Assistant Professor Department of Livestock Management, Animal Breeding Sep2017 Till date and Genetics, The University of Agriculture Peshawar Lecturer BPS-18 Department of Livestock Management, Animal Breeding June2014 Sep2017 and Genetics, The University of Agriculture Peshawar Research Livestock & Dairy Development (Research Wing) Aug2011 June2014 Officer/Assistant Government of Khyber Pakhtunkhwa Director (P&D) Research Officer Livestock Research and Development Station Surezai June2009 July2011 Peshawar Veterinary Officer Veterinary Research and Disease investigation Center Aug2008 June2009 (Research) Swat CURRENT ACTIVITIES Teaching A. Teaching following courses to the DVM and M.Sc (Hons) students 1. Dairy Herd Health (Med/Epi.511) to DVM Students of 6th semester 2. Beef Production (LM. 511) to DVM Students of 6th semester 3. Meat Hygiene and Public Health (Path. 601) to DVM students of 7th semester st 4. Livestock Industry (LM) M.Sc (Hons) of 1 semester Research Student’s research supervised a. -

CDRS Report 2014-2018
COMPREHENSIVE DISASTER RESPONSE SERVICES HELPING PEOPLE IN TIMES OF NEED SINCE 2005 Includes organizational profile, current projects Report to Donors accomplishments and 2014-2018 statistics CDRS Sarish Khan Umair Jaswal Ahmed Nawaz Fauzia Shah CDRS AMBASSADOR CDRS AMBASSADOR CDRS AMBASSADOR CDRS AMBASSADOR FOR FOR WOMEN'S FOR WATER & FOR PEACE OVERSEAS PAKISTANI EMPOWERMENT THE ENVIRONMENT COMMUNITIES Nida Jamal Hira Khan Faran Tahir Saima Durrani CDRS AMBASSADOR CDRS AMBASSADOR CDRS AMBASSADOR CDRS AMBASSADOR FOR FOR CHILDREN’S FOR EDUCATION FOR VOLUNTEERISM ANIMAL WELFARE HEALTH & SAFETY AMBASSADORS Isfundiar Mansoor Khadija Seeme Gull Kasuri Mehmood Siddiqui Khan Hasan CHAIRPERSON OF THE CDRS AMBASSADOR CDRS AMBASSADOR CHAIRPERSON OF THE CDRS YOUTH FOR LAW FOR JUSTICE CDRS ADVISORY BOARD ADVISORY BOARD Todd Shea Founder & CEO MESSAGE DEAR CDRS FAMILY, Without You, my team and I simply could not do all the great work we do for less fortunate families. We are so busy with our many eorts which are made possible by you, we wish we had more time to properly express our gratitude personally to each one of you. I want you to know that all of you are in our prayers and we love you for giving us the opportunity to fulfill our purpose in life, which is simply to use as much of our time and experience as possible to serve Human Beings in their time of need, replacing their fear and sadness with hope and smiles, and a chance for a better future. This report focuses on the last five years of CDRS operations in Pakistan, our current projects, and key all-time statistics. -

Vol 17 Issue 01
PATRON JAIMC Prof. Arif Tajammal Principal The Journal of Allama Iqbal Medical College Allama Iqbal Medical College/ Jinnah Hospital Jan - March, 2019, Volume 17, Issue 01 CHIEF EDITOR Rakhshanda Farid A Stitch in Time Saves Nine – Analytic Review of 66 Cases of Chest Trauma 1 ASSOCIATE EDITOR Ghulam Shabbir Pervez, Syed Saqib Raza Bokhari, Saima Sultan, Ahsen Nazeer Hamid Mehmood Butt Ahmad, Muhammad Mohsin Gillani, Ahmad Abutalib Aftab Mohsin Antimicrobial Resistance Pattern of Clinical Isolates of Infected Wounds 6 Farhat Naz Khalil ur Rehman, Faizan Rasool, Anas Rafiq, Saima Anwar, Rafiq Ahmad Rashid Zia Shahid, Aasim Tahir, Muhammad Asif MANAGING EDITOR Muhammad Imran Association of Hypovitaminosis D with Preterm Delivery in Females Presenting 10 STATISTICAL EDITOR for Delivery in Tertiary Care Hospital Mamoon Akbar Qureshi Aiesha Iftikhar Shah, Sunbal Khalid, Sumaira Fatima Sabir DESIGNING & COMPOSING Skin Adnexal Tumors- An Institutional Study of Clinicopathological Features 14 Talal Publishers Tabish S, Mazhar S, Afsar M, Imran E, Ashraf A, Anwar A Shoaib Khan (Finland) Efficacy of Endoscopic Dilation Sessions Time Span in Terms of Resolution of 19 Saad Usmani (USA) Symptoms and Complications Bilal Ayub (USA) Jibran Umar Ayub, Samina Saeed, Khalid Mahmud Khan, Umar Ayub, Romana M. Hassan Majeed (USA) Inaam, Emaan Salam, Ayeslia Qaiser Adnan Agha (Saudi Arabia) 25 Zeeshan Tariq (USA) Infection of Acinetobacter Baumannii and It's Resistant Pattern in a Tertiary Umar Farooq (USA) Care Hospital of Lahore; Pakistan Hina Bukhari, Amna