Vol 17 Issue 01
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Celiac Disease
Original Article DEPRESSION IN HEMODIALYSIS PATIENTS Muhammad Anees1, Haris Barki2, Mahrukh Masood3, Muhammad Ibrahim4, Asim Mumtaz5 ABSTRACT Objective: To measure the frequency of depression and its risk factors in patients under going hemodialysis. Methodology: It is a cross-sectional prospective study conducted at Hemodialysis unit of Shalamar Hospital and Shaikh Zayed Hospital, Lahore from 1st January 2006 to 30th April 2006. All patients getting regular hemodialysis for more than three months were included. Beck’s Depression Inventory- II (BDI-II; adapted in Urdu) was administered on all the patients who were able to read or understand it. Blood sample were drawn at the same time for routine hematological, biochemical parameters and viral markers (Anti HCV and HbsAg). Diagnosis was made as per Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM IV) for correlation of psychological variables with clinical, hematological and biochemical parameters. Results: Eighty nine patients were enrolled which included fifty two (58.4%) were male and seventy seven (86.5%) were married. Major causes of renal failure were diabetes, hypertension and chronic glomerulonephrotis. Duration of dialysis was from 03 to 49 months with mean of 19.64 ± 11.7 months. Severity of depression was categorized in to mild, moderate and severe on the basis of BDI score. Majority of the patients fifty (56.1%) were moderately to severely depressed and there was no gender difference in the prevalence of depression. Conclusions: Majority of patients undergoing hemodialysis were depressed. Major risk factors for depression were marital status, illiteracy, number of children, socioeconomic factors, gender, hypertension and hypoalbuminemia. Patients with anemia, hyponatremia and hyperkalemia had suicidal tendency. -

Shia Target Killing Report
PAKISTAN 31/12/2012 Shaheed Detail in January 2012 Name Date City Reason Nisar Ahmed s/o Sardar Muhammad 18-Jan-12 Quetta Gun Shot Ghulam Muhammad s/o Ghulam Ali 16-Jan-12 Karachi Gun Shot Ghulam Raza 15-Jan-12 Karachi Gun Shot S. Mushtaq Zaidi 12-Jan-12 Karachi Gun Shot Kalb-e-Abbas Rizvi 9-Jan-12 Karachi Gun Shot Dr Jamal 7-Jan-12 Peshawar Gun Shot ASI Ghullam Abbas 5-Jan-12 Quetta Target killing Mushkoor Hussain 5-Jan-12 Lahore Target killing DSP Ibrahim 4-Jan-12 Gilgit Target killing Ghulam Abbas 15-Jan-12 Khanpur Bome Blast Faiz Hussain 15-Jan-12 Khanpur Bome Blast Abad Hussain 15-Jan-12 Khanpur Bome Blast Zahid Abbas 15-Jan-12 Khanpur Bome Blast Asad Abbas 15-Jan-12 Khanpur Bome Blast Mureed Hussain 15-Jan-12 Khanpur Bome Blast Akhter Hussain 15-Jan-12 Khanpur Bome Blast Mohammed Ashaq 15-Jan-12 Khanpur Bome Blast Khezhar Hayat 15-Jan-12 Khanpur Bome Blast Amjad Hussain 15-Jan-12 Khanpur Bome Blast Sadam Hussain 15-Jan-12 Khanpur Bome Blast Abad Hussain 15-Jan-12 Khanpur Bome Blast Aatif 15-Jan-12 Khanpur Bome Blast Adnan 15-Jan-12 Khanpur Bome Blast Faisal Hayat 15-Jan-12 Khanpur Bome Blast Tahir Abbas 15-Jan-12 Khanpur Bome Blast Syed Hussain 15-Jan-12 Khanpur Bome Blast Qurban Hussian 15-Jan-12 Khanpur Bome Blast Ghulam Qadir 17-Jan-12 Khanpur Bome Blast Shahnawaz 17-Jan-12 Khanpur Bome Blast Ali Hussain s/o Muzaffar Abbas 22-Jan-12 Karachi Target killing Asghar Karrar 19-Jan-12 Karachi Target killing Dr. -

Health Bulletin July.Pdf
July, 2014 - Volume: 2, Issue: 7 IN THIS BULLETIN HIGHLIGHTS: Polio spread feared over mass displacement 02 English News 2-7 Dengue: Mosquito larva still exists in Pindi 02 Lack of coordination hampering vaccination of NWA children 02 Polio Cases Recorded 8 Delayed security nods affect polio drives in city 02 Combating dengue: Fumigation carried out in rural areas 03 Health Profile: 9-11 U.A.E. polio campaign vaccinates 2.5 million children in 21 areas in Pakistan 03 District Multan Children suffer as Pakistan battles measles epidemic 03 Health dept starts registering IDPs to halt polio spread 04 CDA readies for dengue fever season 05 Maps 12,14,16 Ulema declare polio immunization Islamic 05 Polio virus detected in Quetta linked to Sukkur 05 Articles 13,15 Deaths from vaccine: Health minister suspends 17 officials for negligence 05 Polio vaccinators return to Bara, Pakistan, after five years 06 Urdu News 17-21 Sewage samples polio positive 06 Six children die at a private hospital 06 06 Health Directory 22-35 Another health scare: Two children infected with Rubella virus in Jalozai Camp Norwegian funding for polio eradication increased 07 MULTAN HEALTH FACILITIES ADULT HEALTH AND CARE - PUNJAB MAPS PATIENTS TREATED IN MULTAN DIVISION MULTAN HEALTH FACILITIES 71°26'40"E 71°27'30"E 71°28'20"E 71°29'10"E 71°30'0"E 71°30'50"E BUZDAR CLINIC TAYYABA BISMILLAH JILANI Rd CLINIC AMNA FAMILY il BLOOD CLINIC HOSPITAL Ja d M BANK R FATEH MEDICAL MEDICAL NISHTER DENTAL Legend l D DENTAL & ORAL SURGEON a & DENTAL STORE MEDICAL COLLEGE A RABBANI n COMMUNITY AND HOSPITAL a CLINIC R HOSPITALT C HEALTH GULZAR HOSPITAL u "' Basic Health Unit d g CENTER NAFEES MEDICARE AL MINHAJ FAMILY MULTAN BURN UNIT PSYCHIATRIC h UL QURAN la MATERNITY HOME CLINIC ZAFAR q op Blood Bank N BLOOD BANK r ishta NIAZ CLINIC R i r a Rd X-RAY SIYAL CLINIC d d d SHAHAB k a Saddiqia n R LABORATORY FAROOQ k ÷Ó o Children Hospital d DECENT NISHTAR a . -
1F35e3e1-Thisday-Jul
NNPC Awards Oil Swap Contracts to 34 Firms Ejiofor Alike with agency contracts to exchange crude the deals said. Barbedos/Petrogas/Rainoil; referred to as offshore crude supplies crude oil to selected reports oil for imported fuel. The winning groups include: UTM/Levene/Matrix/Petra oil processing agreements local and international oil Under the new contract that BP/Aym Shafa; Vitol/Varo; Atlantic; TOTSA; Duke Oil; (OPAs) and crude-for-products traders and refineries in The Nigerian National will take effect this month, a Trafigura/AA Rano; MRS; Sahara; Gunvor/Maikifi; exchange arrangements, are exchange for petrol and diesel. Petroleum Corporation total of 15 groupings, with at Oando/Cepsa; Bono/ Litasco /Brittania-U; and now known as Direct Sale- NNPC had in May 2017, (NNPC) yesterday issued least 34 companies in total, Akleen/Amazon/Eterna; Mocoh/Mocoh Nigeria. Direct Purchase Agreements signed the deals with local award letters to oil firms received award letters, four Eyrie/Masters/Cassiva/ NNPC’s crude swap deals, (DSDP). for the highly sought-after sources with knowledge of Asean Group; Mercuria/ which were previously Under the deals, the NNPC Continued on page 8 Lower Commodity Prices Weaken Inflation to 11.22%... Page 8 Tuesday 16 July, 2019 Vol 24. No 8863 Price: N250 www.thisdaylive.com T RU N TH & REASO Oyo Governor Publicly Declares Assets Worth over N48bn... Page 9 Obasanjo Calls for National Confab, Says Nigeria is on the Precipice Writes Buhari PDP, Afenifere, Ohanaeze, Southern, Middle Belt leaders back former president Yakassai faults content of letter By Our Correspondents plunging into an abyss of before Nigeria witnesses the varied reactions from some aligned with Obasanjo’s Forum (ACF), Alhaji Tanko insecurity. -

Assessment of Adherence to the Core Elements of Hospital Antibiotic Stewardship Programs: a Survey of the Tertiary Care Hospitals in Punjab, Pakistan
antibiotics Article Assessment of Adherence to the Core Elements of Hospital Antibiotic Stewardship Programs: A Survey of the Tertiary Care Hospitals in Punjab, Pakistan Naeem Mubarak 1,* , Asma Sarwar Khan 1, Taheer Zahid 1 , Umm e Barirah Ijaz 1, Muhammad Majid Aziz 1, Rabeel Khan 1, Khalid Mahmood 2 , Nasira Saif-ur-Rehman 1,* and Che Suraya Zin 3,* 1 Department of Pharmacy Practice, Lahore Medical & Dental College, University of Health Sciences, Lahore 54600, Pakistan; [email protected] (A.S.K.); [email protected] (T.Z.); [email protected] (U.e.B.I.); [email protected] (M.M.A.); [email protected] (R.K.) 2 Institute of Information Management, University of the Punjab, Lahore 54000, Pakistan; [email protected] 3 Kulliyyah of Pharmacy, International Islamic University Malaysia, Kuantan 25200, Malaysia * Correspondence: [email protected] (N.M.); [email protected] (N.S.-u.-R.); [email protected] (C.S.Z.) Abstract: Background: To restrain antibiotic resistance, the Centers for Disease Control and Preven- tion (CDC), United States of America, urges all hospital settings to implement the Core Elements of Hospital Antibiotic Stewardship Programs (CEHASP). However, the concept of hospital-based antibiotic stewardship programs is relatively new in Low- and Middle-Income Countries. Aim: To Citation: Mubarak, N.; Khan, A.S.; appraise the adherence of the tertiary care hospitals to seven CEHASPs. Design and Setting: A cross- Zahid, T.; Ijaz, U.e.B.; Aziz, M.M.; sectional study in the tertiary care hospitals in Punjab, Pakistan. Method: CEHASP assessment tool, Khan, R.; Mahmood, K.; (a checklist) was used to collect data from the eligible hospitals based on purposive sampling. -
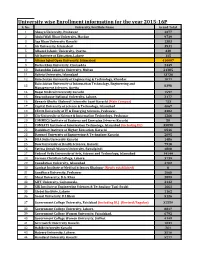
University Wise Enrollment Information for the Year 2015-16P S
University wise Enrollment information for the year 2015-16P S. No. University/Institute Name Grand Total 1 Abasyn University, Peshawar 4377 2 Abdul Wali Khan University, Mardan 9739 3 Aga Khan University Karachi 1383 4 Air University, Islamabad 3531 5 Alhamd Islamic University, Quetta. 338 6 Ali Institute of Education, Lahore 115 8 Allama Iqbal Open University, Islamabad 416607 9 Bacha Khan University, Charsadda 2449 10 Bahauddin Zakariya University, Multan 21385 11 Bahria University, Islamabad 13736 12 Balochistan University of Engineering & Technology, Khuzdar 1071 Balochistan University of Information Technology, Engineering and 13 8398 Management Sciences, Quetta 14 Baqai Medical University Karachi 1597 15 Beaconhouse National University, Lahore. 2177 16 Benazir Bhutto Shaheed University Lyari Karachi (Main Campus) 753 17 Capital University of Science & Technology, Islamabad 4067 18 CECOS University of IT & Emerging Sciences, Peshawar. 3382 19 City University of Science & Information Technology, Peshawar 1266 20 COMMECS Institute of Business and Emerging Sciences Karachi 50 21 COMSATS Institute of Information Technology, Islamabad (including DL) 35890 22 Dadabhoy Institute of Higher Education, Karachi 6546 23 Dawood University of Engineering & Technology Karachi 2095 24 DHA Suffa University Karachi 1486 25 Dow University of Health Sciences, Karachi 7918 26 Fatima Jinnah Women University, Rawalpindi 4808 27 Federal Urdu University of Arts, Science and Technology, Islamabad 14144 28 Forman Christian College, Lahore. 3739 29 Foundation University, Islamabad 4702 30 Gambat Institute of Medical Sciences Khairpur (Newly established) 0 31 Gandhara University, Peshawar 1068 32 Ghazi University, D.G. Khan 2899 33 GIFT University, Gujranwala. 2132 34 GIK Institute of Engineering Sciences & Technology Topi-Swabi 1661 35 Global Institute, Lahore 1162 36 Gomal University, D.I.Khan 5126 37 Government College University, Faislabad (including DL) (Revised/Regular) 32559 38 Government College University, Lahore. -

HEC RECOGNIZED LOCAL JOURNALS (Languages, Arts & Humanities)
HEC RECOGNIZED LOCAL JOURNALS (Languages, Arts & Humanities). The HEC is not responsible for the content of external internet sites. Y' CATEGORY JOURNALS: Acceptable for Tenure Track System, BPS appointments, HEC Approved Supervisor and Publication of research of Ph.D. work until 30th June 2016 S. No. Journal Name ISSN University Editor/Contact Person Subject w.e.f. Tel/Mob No. Fax No. E-mail Website The Iqbal review Iqbal Academy, 6th Floor, Aiwan-i- 1 0021-0773 Muhammad Suheyl Umar Iqbal Studies Jun-05 42-6314510 42-6314496 [email protected] http://www.allamaiqbal.com/ – A quarterly Journal Iqbal, Egerton Road, Lahore Department of English, University of May,12 2 Kashmir Journal of Language Research 1028-6640 Azad Jammu & Kashmir, Dr. Raja Nasim Akhter Language (in category 'Z' from Sep,08 99243131 Ext 2278 www.ajku.edu.pk Muzaffarabad till Apr,11) Journal of Research (Urdu) Formerly February 2015 (In 'Z' Department of Urdu Bahauddin 3 Journal of Research (Languages & Islamic 1726-9067 Dr.Rubina Tareen Urdu Category from Dec, 08 till 061-9210117 061-9210108 [email protected] http://www.bzu.edu.pk/jrlanguages/defalt.htm Zakariya University, Multan Studies) January 2015) February 2015 (In 'Z' Department of Urdu, Shah Abdul 4 Almas 1818-9296 Dr.M. Yusuf Khushk Urdu Category from Jun, 05 till 0243-9280291 0243-9280291 [email protected] http://www.salu.edu.pk/research/publication/journals/urdu/almas/ Latif University, Khairpur January 2015) February 2015 (In 'Z' Department of Urdu, Government 5 Tahqeeq Nama 1997-7611 Dr.M. Haroon Qadir Urdu Category from June 2005 042-99213339 - [email protected] http://gcu.edu.pk/TehqNama.htm College University, Lahore till January 2015) Gurmani Centre for Languages and February 2015 (In 'Z' 6 Bunyad 2225-5083 Literature, Lahore University of Dr. -

Presentations by National Speakers
PRESENTATIONS By National Speakers Pak J Med Sci 2016 www.pjms.com.pk Special Supplement Abstract Book IDEC August 2016 49 34- Shall we be treating all women with HRT? Hormone replacement therapies, Metabolic and cardiovascular effects. Prof. A.H. Aamir Consultant Endocrinologist, Professor of Medicines, Head of Department of Endocrinology, Hayatabad Medical Complex, Peshawar. Menopause affects every woman and it usually occurs at a median age of 51 years. As large number of women is reaching midlife, it is likely that physicians will come across a stage where HRT may need to be considered for their patient. Menopause has Physical, Psychological, Uro-genital tract, Cardiovascular, Skeletal effects. Estrogens also have effects on carbohydrate homeostasis, fatty liver and atherosclerosis. Postmenopausal women with hyper-androgenemia have elevated risks for NIDDM-Risk and CHD. Most of these effects are reversible with replacement of Estrogens. Women health initiative study (WHI) initially showed an increased cardiovascular risk with HRT increased risk of VTE, stroke, MI Risk appears to be higher in initial years of treatment, followed by decline in risk. Recent re-analyses of WHI results suggested that the association between HRT and cardiovascular risk is influenced by factors such as age and time since menopause • Reduced CV risk in women <10 years post-menopause. • WHI population included older women with other CV risk factors. Risks of stroke should be balanced against benefits, such as decreased risk of hip fracture. Treatment with HRT needs to be individualized in the light of recent International menopausal society recommendations. 50 Pak J Med Sci 2016 www.pjms.com.pk Special Supplement Abstract Book IDEC August 2016 35- Characteristics of Fasting and Ramadan-specific diabetes education trends in people with diabetes (CARE) Prof. -

General Merit List of Reserved Seats for P.U Teachers for Admission to Pharm.D 1St Professional Morning Class Session 2020-2025
PUNJAB UNIVERSITY COLLEGE OF PHARMACY UNIVERSITY OF THE PUNJAB, LAHORE. General Merit list of Reserved seats for P.U Teachers for Admission to Pharm.D 1st Professional Morning class session 2020-2025. Note: Any Candidate who has submitted the complete admission form on college admission portal, i.e., admissionpucp.edu.pk or pucp.edu.pk with fullfilling all requirements, but his/her name is not inculde in the General merit list should report to the college admission office before 03-11-2020. No complaint will be entertained after 03-11-2020. The University Reserves the Right to correct any Typographical Error, Ommision etc. Sr. Year of % Merit Late Year Final Merit Form ID Name of Student Father name Status No. Passing Marks Deduction Marks 1 DB5866 MUHAMMAD HAMZA SHOAIB HAJI MUHAMMAD SHOAIB KHAN 2020 94.655 0 94.655 Son 2 DB11359 HAFIZA SARA HASSAN HAFIZ HASAN MADNI 2020 94.255 0 94.255 Daughter 3 DB6061 KHANSA IJAZ MUHAMMAD IJAZ 2020 91.236 0 91.236 Daughter 4 DB7458 IZZA ALMATEEN SOHAIL SOHAIL AFZAL TAHIR 2020 90.273 0 90.273 Daughter Daughter 5 DB10100 AYESHA KHALIL KHALIL AHMAD 2020 88.836 0 88.836 Letter Required 6 DB5267 AZQA AHMAD AHMAD ISLAM 2020 88.764 0 88.764 Daughter 7 DB6048 MUSFIRA FATIMA MALIK AHMED SHER AWAN 2020 87.400 0 87.400 Daughter 8 DB8059 AREEBA AMER SYED AMER MAHMOOD 2020 86.182 0 86.182 Daughter 9 DB5799 SHEHROZE RAUF SHAKOORI ABDUL RAUF SHAKOORI 2020 83.132 0 83.132 Son Daughter 10 DB8639 AYESHA SOHAIL BUTT 2019 83.436 2 81.436 Letter Required 11 DB12029 UM E ABIHA SIKANDARR SIKANDAR HAYAT KHAN 2017 80.582 6 -

Serum 25-Hydroxy Vitamin D Level in Preeclamptic and Normotensive
ORIGINAL ARTICLE Serum 25-Hydroxy Vitamin D Level in Preeclamptic and Normotensive Pregnancies Naima Umar1, Ambreen Tauseef2, Fazeela Shahzad*, Sana Sabir3, Shumaela Kanwal4, Ayesha Akmal2 and Sibgha Zulfiqar5 ABSTRACT Objective: To compare serum 25-hydroxy vitamin D level between preeclamptic and normotensive pregnancies. Study Design: Cross-sectional analytical study. Place and Duration of Study: Department of Physiology, Federal Postgraduate Medical Institute, Shaikh Zayed Hospital, Lahore, in collaboration with Sir Ganga Ram Hospital and Lady Willingdon Hospital, Lahore, from March 2012 to April 2012. Methodology: Thirty registered preeclamptic patients with systolic and diastolic blood pressure > 140/90 mm Hg on more than two occasions, 6 hours apart, and proteinuria at least 300 mg in 24-hour urine collection; and 30 normotensive uncomplicated pregnant women matched for age, gestational age, parity and BMI were included by convenient sampling technique. Vitamin D levels of less than 50 n mol/l (< 20 ng/ml) was the cutoff point. Spearman's rank correlation of vitamin D with systolic blood pressure and arterial pressure in both preeclamptic and normotensive pregnant women was presented in a tabulated form. Results: Vitamin D deficiency was found in 95% of preeclamptic and normotensive pregnant women. The difference of vitamin D level between the two groups was not found significant. Although there was an inverse correlation between serum vitamin D and systolic blood pressure and arterial pressure in preeclamptic group, but this was not statistically significant. Conclusion: Vitamin D deficiency does not seem to be affected by the state of preeclamptic and normotensive pregnancy. The correlation of systolic blood pressure and arterial pressure and vitamin D needs to be explored further by increasing the sample size. -

Professional Resume
Address: Phone: Suit #104,TMKN property Mobile: +971564837368 building , near Infinity showroom, E-mail: Najda Street, Abu Dhabi, [email protected] UAE [email protected] Umar Mehmood I am working as “Biomedical Service Manager” in a U.A.E based organization, dealing in Diagnostic Electro-medical Equipment and they are exclusive distributor of HITACHI MEDICAL SYSTEMS, VARIAN MEDICAL, PROTEC, AGFA HEALTH CARE, LODOX, STEPHANIX, IMAGING DYNAMICS, MALVESTIO, NIPRO AND ABBOT in U.A.E. Objective To work in a dynamic and challenging work environment and explore the opportunities for personal learning, professional growth and organizational development. Work Experience Al-Razi Pharmacy Company,(Hitachi Medical Equipment) UAE Working as Biomedical Service Manage from October 2014 to till now My Responsibilities are as under: 1- Installation, Demonstration and Repair of Hitachi CT, MRI, X-ray, Flouro and Ultrasound equipments. 2- Installation, Demonstration and Repair of Protec X-rays. 3- Maintenance and Repair of Stephanix X-ray and Fluoroscopy equipments 4- Communication with our foreign principles 5- Team Leader/Customer service support 6- Management work/Control turnkey projects 7- Application training for CT, MRI, Xray, Flouro and Ultrasound . 8- Get service/maintenance contract from customers. 9- Conduct product trainings for the new employees. 10- Support Sales team as product specialist in sale process. Ittefaq Sons (Hitachi Medical System), Lahore Worked as Manager Technical from January 2013 to September 2014. Installation, Maintenance and demonstration of CT scan, X- rays, C-arm, Fluoroscopy, Color Doppler etc. MEDEQUIPS (Toshiba Medical Systems), Lahore Worked as Senior Engineer from August 2004 to December 2012 1- Installation, Maintenance and Demonstration of ECGs , Central Monitoring System, Defibrillator, EEG Machines, EMG Machines, Cardiac Monitors, Patients Monitors, TELEMETRY Central Monitoring System and Stress test System, of NIHON KOHDEN, JAPAN 2- Installation, Maintenance and demonstration of X-ray machines. -

List of Gold Medal Winners
LIST OF GOLD MEDAL WINNERS FIRST POSITION IN PAKISTAN S. NO. ROLL NO. STUDENT NAME FATHER NAME CLASS INSTITUTION ADDRESS CITY/DISTRICT STREET NO. 18, BLOCK-B, KAZIMABAD, 1 16-021-00372-1-011-E AAYAN BASHIR KAMRAN BASHIR 1 BEACON ASKARI O LEVEL SCHOOL KARACHI MODEL COLONY THE CITY SCHOOL HAYATABAD HOUSE NO. 33-34, STREET NO. 01, 2 16-91-00763-1-033-E ABBAS ALI KHAN WALI KHAN 1 PESHAWAR JUNIOR SECTOR K - 5, PHASE - 3, HAYATABAD 3 16-42-00816-1-008-E ABDUL HAYEE SHAHZAD RAO SHAHZAD QAMAR 1 BEACONHOUSE SCHOOL SYSTEM HOUSE NO. 41 - A1, PECO ROAD LAHORE HEAVY INDUSTORIES TAXILA 4 16-51-00703-1-021-E ABDUL REHMAN MUHAMMAD RIAZ 1 HITEC PRE SCHOOL RAWALPINDI EDUCATION CITY, KHANPUR ROAD 5 16-41-00186-1-004-E ABDUL SAMAD BILAL BILAL QAYYUM PURI 1 LEARNING ALLIANCE 1 - AMIR TOWN EAST CANAL ROAD FAISALABAD THE CITY SCHOOL HAYATABAD HOUSE NO. 33-34, STREET NO. 01, 6 16-91-00763-1-036-E ABDULLAH MUHAMMAD NISAR MUHAMMAD 1 PESHAWAR JUNIOR SECTOR K - 5, PHASE - 3, HAYATABAD THE CITY SCHOOL RISALPUR HOUSE NO. 3/10, MEHMOOD ROAD, 7 16-923-00652-1-001-E ABDULLAH SHAHID SHAHID RIAZ 1 NOWSHERA CAMPUS RISALPUR CANTT DEFENCE HOUSING AUTHORITY 8 16-42-20026-1-005-E ABDULLAH ZAHEER ZAHEER ALI 1 970-K, SECTOR-Z, PHASE-3, DHA CANTT LAHORE JUNIOR CAMPUS STREET NO. 18, BLOCK-B, KAZIMABAD, 9 16-021-00372-1-063-E ABEERA ASIF ASIF PERVEZ 1 BEACON ASKARI O LEVEL SCHOOL KARACHI MODEL COLONY THE CITY SCHOOL WAPDA TOWN 10 16-42-00613-1-004-E ABEERA NASIR NASIR HAMEED 1 HOUSE NO.