Systems of Classification in Premodern Medical Cultures; Sickness
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Periodontology – the Historical Outline from Ancient Times Until the 20Th Century Istorijski Razvoj Parodontologije Zlata Brkić*†, Verica Pavli懧
Vojnosanit Pregl 2017; 74(2): 193–199. VOJNOSANITETSKI PREGLED Page 193 UDC: 616.31(091) HISTORY OF MEDICINE DOI: 10.2298/VSP150612169B Periodontology – the historical outline from ancient times until the 20th century Istorijski razvoj parodontologije Zlata Brkić*†, Verica Pavli懧 *Clinic for Dentistry, Military Medical Academy, Belgrade, Serbia; †Faculty of Medicine of the Military Medical Academy, University of Defence, Belgrade, Serbia; ‡Department of Periodontology and Oral Medicine, Institute of Dentistry, Banja Luka, Bosnia and Herzegovina; Department of Periodontology and Oral Medicine, §Faculty of Medicine, University of Banja Luka, Banja Luka, Bosnia and Herzegovina Introduction cations 1–3. This finding was further confirmed by decorated gold toothpicks founded in the exavations at the Nigel Tem- The diseases of the periodontium are considered as old as ple, Ur in Mesopotamia 2. 1–3 the recorded history of mankind . The historical evaluation of Almost all of our knowledge of Babylonian and pathology and therapeutics can be traced through the variety of Assyrian medicine comes from the clay tablets of the great sources: anatomical findings from more or less well-preserved library of Ashurbanipal (king of Assyria), that includes a skeletal parts, detailes observed in mummies, instruments and number of remedies for periodontal disease, such as “if a equipments collected during archaelogical investigations and man's teeth are loose and itch a mixture of myrrh, asafetida evidence from engravings and various manuscripts 2. Studies in and opopanax, as well as pine-turpentine shall be rubbed on paleopathology have indicated that a destructive periodontal di- his teeth until blood comes forth and he shall recover” 2. -

Joyful in Thebes Egyptological Studies in Honor of Betsy M
JOYFUL IN THEBES EGYPTOLOGICAL STUDIES IN HONOR OF BETSY M. BRYAN MATERIAL AND VISUAL CULTURE OF ANCIENT EGYPT Editors X xxxxx, X xxxx NUMBER ONE JOYFUL IN THEBES EGYPTOLOGICAL STUDIES IN HONOR OF BETSY M. BRYAN JOYFUL IN THEBES EGYPTOLOGICAL STUDIES IN HONOR OF BETSY M. BRYAN Edited by Richard Jasnow and Kathlyn M. Cooney With the assistance of Katherine E. Davis LOCKWOOD PRESS ATLANTA, GEORGIA JOYFUL IN THEBES EGYPTOLOGICAL STUDIES IN HONOR OF BETSY M. BRYAN Copyright © 2015 by Lockwood Press All rights reserved. No part of this work may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying and recording, or by means of any information storage or retrieval system, except as may be expressly permitted by the 1976 Copyright Act or in writing from the publisher. Requests for permission should be addressed in writing to Lockwood Press, PO Box 133289, Atlanta, GA 30333 USA. Library of Congress Control Number: 2015944276 ISBN: 978-1-937040-40-6 Cover design by Deborah Shieh, adapted by Susanne Wilhelm. Cover image: Amenhotep III in the Blue Crown (detail), ca. 1390–1352 BCE. Quartzite, Ht. 35 cm. Face only: ht. 12.8 cm; w. 12.6 cm. Rogers Fund, 1956 (56.138). Image copyright © the Metropolitan Museum of Art. Image source: Art Resource, NY. is paper meets the requirements of ANSI/NISO Z39.48-1992 (Permanence of Paper). CONTENTS Acknowledgments ix Introduction xi Abbreviations xvii Bibliography of Betsy M. Bryan xxiv Tabula Gratulatoria xxviii T A. BÁCS Some Aspects of Tomb Reuse during the Twentieth Dynasty 1 Y BARBASH e Lion-Headed Goddess and Her Lost Cat: Brooklyn Museum 37.1379E 11 H BASSIR On the Historical Implications of Payeftjauemawyneith’s Self-Presentation on Louvre A 93 21 L M. -

Practicing Medicine in Ancient Egypt
Practicing Medicine in Ancient Egypt Michael R. Zimmerman March 28, 2017 Michael Zimmerman is Adjunct Professor of Biology at Villanova University, Lecturer in Anthropology at the University of Pennsylvania, and Visiting Professor at the University of Manchester (UK) KNH Centre for Biomedical Egyptology. et us start by imagining what Albert Einstein called a “thought experiment.” It is the year 5015 CE L and an excavation of an ancient hospital, ca. 2016 CE, uncovers an ancient book, written on paper rather than on the current electronic device. Although the book is in poor condition there is a partial hieroglyphic title, transcribed by an Egyptologist and a paleopathologist as Merck Manual. The book seems to be a compilation of disease descriptions and treatments by a long forgotten Dr. Merck. The diseases are difficult to decipher in an era when humans live to the age of 150 and die only when aged organs fail. It appears that the body could be attacked by minute parasitic organisms, visible only with an ancient tool called a “microscope.” Some cells appear to have taken on a life of their own, destroying the body by causing diseases known by a variety of poorly preserved terms such as “cancer” or “neoplasm.” The task of our future paleopathologist is analogous to that of the difficult undertaking of deciphering ancient Egyptian medical papyri. There are a number of surviving papyri, in various degrees of completeness, which have been studied by physicians and Egyptologists. They have done remarkably well, particularly in that the writing is mostly in the difficult hieratic rather than hieroglyphic text. -

Joyful in Thebes an International Group of Scholars Have Contributed to Joyful Egypto Logical Studies in Honor of Betsy M
Joyful in Thebes An international group of scholars have contributed to Joyful Egypto in Thebes, a Festschrift for the distinguished Egyptologist Betsy M. Bryan. The forty-two articles deal with topics of art history, archaeology, history, and philology, representing virtually the entire span of ancient Egyptian civilization. logical Studies in Honor of Betsy M. Bryan These diverse studies, which often present unpublished material or new interpretations of specific issues in Egyptian history, literature, and art history, well reflect the broad research interests of the honoree. Abundantly illustrated with photographs and line drawings, the volume also includes a comprehensive bibliography of Bryan’s publications through 2015. Richard Jasnow is professor of Kathlyn M. Cooney is Egyptological Studies in Honor of Egyptology at Johns Hopkins University. associate professor of Egyptian He has authored A Late Period Hieratic Art and Architecture at UCLA. She Betsy M. Bryan Wisdom Text (P. Brooklyn 47.218.135) is author of The Cost of Death: (The Oriental Institute of the University The Social and Economic Value of of Chicago, 1992) and The Ancient Ancient Egyptian Funerary Art in Egyptian Book of Thoth (Harrassowitz, the Ramesside Period (Nederlands 2005; with Karl-Theodor Zauzich). Instituut voor het Nabije Oosten, 2007) Jasnow’s research focuses on Demotic and The Woman Who Would Be King: texts of the Graeco-Roman period. Hatshepsut’s Rise to Power in Ancient Egypt (Crown, 2014). Her research Kathlyn M. Cooney Katherine E. Davis is a focuses on craft specialization, Richard Jasnow graduate student in Egyptology ancient economics, funerary material at Johns Hopkins University. culture, and social crisis. -
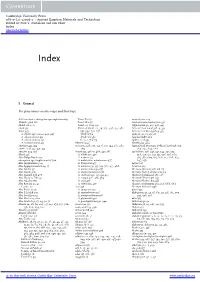
I General for Place Names See Also Maps and Their Keys
Cambridge University Press 978-0-521-12098-2 - Ancient Egyptian Materials and Technology Edited by Paul T. Nicholson and Ian Shaw Index More information Index I General For place names see also maps and their keys. AAS see atomic absorption specrophotometry Tomb E21 52 aerenchyma 229 Abbad region 161 Tomb W2 315 Aeschynomene elaphroxylon 336 Abdel ‘AI, 1. 51 Tomb 113 A’09 332 Afghanistan 39, 435, 436, 443 abesh 591 Umm el-Qa’ab, 63, 79, 363, 496, 577, 582, African black wood 338–9, 339 Abies 445 591, 594, 631, 637 African iron wood 338–9, 339 A. cilicica 348, 431–2, 443, 447 Tomb Q 62 agate 15, 21, 25, 26, 27 A. cilicica cilicica 431 Tomb U-j 582 Agatharchides 162 A. cilicica isaurica 431 Cemetery U 79 agathic acid 453 A. nordmanniana 431 Abyssinia 46 Agathis 453, 464 abietane 445, 454 acacia 91, 148, 305, 335–6, 335, 344, 367, 487, Agricultural Museum, Dokki (Cairo) 558, 559, abietic acid 445, 450, 453 489 564, 632, 634, 666 abrasive 329, 356 Acacia 335, 476–7, 488, 491, 586 agriculture 228, 247, 341, 344, 391, 505, Abrak 148 A. albida 335, 477 506, 510, 515, 517, 521, 526, 528, 569, Abri-Delgo Reach 323 A. arabica 477 583, 584, 609, 615, 616, 617, 628, 637, absorption spectrophotometry 500 A. arabica var. adansoniana 477 647, 656 Abu (Elephantine) 323 A. farnesiana 477 agrimi 327 Abu Aggag formation 54, 55 A. nilotica 279, 335, 354, 367, 477, 488 A Group 323 Abu Ghalib 541 A. nilotica leiocarpa 477 Ahmose (Amarna oªcial) 115 Abu Gurob 410 A. -

Le Papyrus Hiératique Iatromagique N°47.218.2 Du Musée De Brooklyn Ivan Guermeur
Le papyrus hiératique iatromagique n°47.218.2 du musée de Brooklyn Ivan Guermeur To cite this version: Ivan Guermeur. Le papyrus hiératique iatromagique n°47.218.2 du musée de Brooklyn. Bulletin de la Societe française d’egyptologie, Société française d’égyptologie 2016, pp.10-28. halshs-02127003 HAL Id: halshs-02127003 https://halshs.archives-ouvertes.fr/halshs-02127003 Submitted on 29 Jul 2020 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Copyright nos 193-194 Novembre 2015-Mars 2016 193-194 os n | Novembre 2015-Mars 2016 Le Bulletin de la Société française d’égyptologie, qui paraît depuis 1949, fait le compte rendu des réunions organisées régulièrement par cette association, et livre le texte complet des communications qui y sont faites par des chercheurs spécialisés dans les différentes facettes de la recherche en archéologie égyptienne. Il s’adresse aux personnes qui s’intéressent à l’étude de l’Égypte, de ses origines à la période copto-byzantine, et les informe sur les derniers développements des travaux en cours, notamment sur le terrain. Il permet de mettre en relation des professionnels avec un public féru d’égyptologie, tant en France qu’à l’étranger. -

Of the Temple of Mentuhotep II at Deir Al-Bahari Luc Gabolde
The “Kernbau” of the Temple of Mentuhotep II at Deir al-Bahari Luc Gabolde To cite this version: Luc Gabolde. The “Kernbau” of the Temple of Mentuhotep II at Deir al-Bahari: A Monumental Sun Altar ?. Richard Jasnow (University of Chicago); Kathlyn M. Cooney (UCLA). Joyful in Thebes, Egyptological Studies in Honor of Betsy M. Bryan, 1, Lockwood Press, pp.145-154, 2015, Material and Visual Culture of Ancient Egypt, 9781937040406. hal-01895079 HAL Id: hal-01895079 https://hal.archives-ouvertes.fr/hal-01895079 Submitted on 13 Oct 2018 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Copyright JOYFUL IN THEBES EGYPTOLOGICAL STUDIES IN HONOR OF BETSY M. BRYAN MATERIAL AND VISUAL CULTURE OF ANCIENT EGYPT Editors X xxxxx, X xxxx NUMBER ONE JOYFUL IN THEBES EGYPTOLOGICAL STUDIES IN HONOR OF BETSY M. BRYAN JOYFUL IN THEBES EGYPTOLOGICAL STUDIES IN HONOR OF BETSY M. BRYAN Edited by Richard Jasnow and Kathlyn M. Cooney With the assistance of Katherine E. Davis LOCKWOOD PRESS ATLANTA, GEORGIA JOYFUL IN THEBES EGYPTOLOGICAL STUDIES IN HONOR OF BETSY M. BRYAN Copyright © 2015 by Lockwood Press All rights reserved. No part of this work may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying and recording, or by means of any information storage or retrieval system, except as may be expressly permitted by the 1976 Copyright Act or in writing from the publisher. -

Medicine and Society in Ptolemaic Egypt Studies in Ancient Medicine
Medicine and Society in Ptolemaic Egypt Studies in Ancient Medicine Edited by John Scarborough Philip J. van der Eijk Ann Ellis Hanson Joseph Ziegler VOLUME 41 The titles published in this series are listed at brill.com/sam Medicine and Society in Ptolemaic Egypt By Philippa Lang LEIDEN • BOSTON 2013 Cover illustration: Cippus of Horus, 322–280BCE. Image © The Metropolitan Museum of Art/Art Resource NY. Library of Congress Cataloging-in-Publication Data Lang, Philippa, 1974- Medicine and society in Ptolemaic Egypt / by Philippa Lang. p. cm. – (Studies in ancient medicine, ISSN 0925-1421 ; v. 41) Includes bibliographical references and index. ISBN 978-90-04-21858-1 (hardback : alk. paper) – ISBN 978-90-04-23551-9 (e-book) 1. Medicine, Egyptian. 2. Medicine, Ancient. 3. Medicine, Greek and Roman. 4. Human body–Egypt. 5. Medical logic–History. 6. Physicians–Egypt–History. 7. Medicine–Egypt–Alexandria–History. I. Title. R137.L36 2012 610.938–dc23 2012026425 This publication has been typeset in the multilingual “Brill” typeface. With over 5,100 characters covering Latin, IPA, Greek, and Cyrillic, this typeface is especially suitable for use in the humanities. For more information, please see www.brill.com/brill-typeface. ISSN 0925-1421 ISBN 978-90-04-21858-1 (hardback) ISBN 978-90-04-23551-9 (e-book) Copyright 2013 by Koninklijke Brill NV, Leiden, The Netherlands. Koninklijke Brill NV incorporates the imprints Brill, Global Oriental, Hotei Publishing, IDC Publishers, Martinus Nijhof Publishers and VSP. All rights reserved. No part of this publication may be reproduced, translated, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, without prior written permission from the publisher. -

International Journal of Tourism and Hospitality Management Volume 1, No
International Journal of Tourism and Hospitality Management Volume 1, No. 1, June 2018 ___________________________________________________________ ROLE OF THE HAIR IN ANCIENT EGYPT ___________________________________________________________ HODA ABD ALLAH KANDIL FACULTY OF TOURISM AND HOTELS, SADAT CITY UNIVERSITY, EGYPT MAHMOUD EL-MOHAMDY ABDELHADY SALAMA MANSOURA UNIVERSITY, EGYPT ABSTRACT The main aim of this research is to study the role of the hair in Ancient Egypt, as the hair was generally a symbol of mourning. In this regard, the study is divided into two (6) major parts as follows: Introduction, The hair care in ancient Egypt, The Hair as Symbol of Mourning, Diseases of Hair and their Treatment, The result, and the catalog of the hair styles in ancient Egypt. KEYWORDS: Ancient Egypt, Diseases, Hair, Mourning, Treatment. INTRODUCTION The presence and absence of hairstyle were all of great importance to the ancient Egyptians, not only as a matter of personal appearance, but also as symbols or indications of status. The act of ritual humiliation and subjection was demonstrated by the king’s action of seizing his enemies by the hair before smiting them. The ancient Egyptians took great care of their hair, and were concerned with avoiding grayness and baldness, judging from the survival of texts including remedies for these conditions, none of which seems likely to have been very effective. Nevertheless, the hair was usually washed and scented, and wealthy individuals employed hairdressers. Children wore their hair at the side of the head sometimes as one or two tresses or as a braid; and it was otherwise shaven. This characteristic side lock of youth was regularly depicted, even in the portrayals of deities such as the infant Horus (Hippocrates). -

DTTK 3 09 Materie.Indd 5 07-09-2009 13:35:22 6 Jens Bruun Kofoed
INTRODUKTION Mod en skandinavisk missional ekklesiologi 3 ARTIKLER Missional ekklesiologi En teologihistorisk analyse af en ekklesiologisk tradition 5 Missional kirke i Danmark 23 Missional folkekirke: En kirke med egenart? 39 Det bedste fra to verdener Missional kirke i spændingsfeltet mellem danske kulturer 56 Missional kirke: En marginal kirke? Mod en post-kristen ekklesiologi 77 Missional kirke: En kirke sendt til det danske folk 97 Dansk Dansk T idsskrift for INDHOLD T eologi og INTRODUKTION K Forord fra gæsteredaktøren irke Jens Bruun Kofoed 3 03 ARTIKLER Prolegomena til Israels historie Jens Bruun Kofoed 5 Virkelig verden – eller? Dansk Tidsskrift for Teologi og Kirke / 2009 / 03 / 36. årgang Om historisk troværdighed for patriarkfortællingen i Genesis Hans-Ole Bækgaard 25 ISRAELS HISTORIE I DET GAMLE TESTAMENTE: Jens Bruun Kofoed / Hans-Ole Bækgaard / Carsten Vang / Nicolai Winther-Nielsen / Tremper Longman / Kurt E. Larsen Exodus – teologisk myte eller historisk begivenhed? Carsten Vang 47 Israels bosættelse – om generobring af en historisk forpost Nicolai Winther-Nielsen 69 Statsdannelsen I DET GAMLE TESTAMENTE ISRAELS HISTORIE Jens Bruun Kofoed 91 Eksilet og tiden efter Tremper Longman 113 ANMELDELSER Når det regner på præsten Kurt E. Larsen 142 Hal Koch – en biografi Kurt E. Larsen 143 Dansk Tidsskrift for Teologi og Kirke - Menighedsfakultetet - Katrinebjergvej 75 - DK-8200 Århus N 200 kr KURSUS SEKULARISERING Redaktør Jeppe B. Nikolajsen Redaktion Leif Andersen, Peter Thise, OG RELIGIØS VITALITET Morten H. Jensen, Andreas Ø. Nielsen, Klaus Vibe og Per D. Pedersen - Kristendom i Danmark Redaktionssekretær Henrik H. Hansen i det 21. århundrede Regnskabsfører Walther P. Hansen Layout og sats Graphic Care Mange kirkefolk ser sekularisering som tidens Trykkeri Handy-Print største udfordring – men hvad ved vi, og hvad Oplag 500 tror vi på? Nye interviews med danskere fra ISSN 1903-6523 alle samfundslag giver udtryk for kristendom i Hjemmeside www.teologisk-tidsskrift.dk Copyright Forfatterne og Dansk Tids- sammenblanding med stort set hvad som helst. -

The Decree of Saïs
Underwater Egypt in Region Canopic the in Archaeology OCMA Underwater Archaeology in the Canopic Region in Egypt The Decree of Saïs The Decree of Saïs of Decree The The cover illustrations show the perfectly preserved stele of Thonis-Heracleion, intact after having spent over 1000 years at the bottom of the sea. It is the second known stele containing the text of the decree promulgated by Nectanebo I,founder of the thirtieth dynasty, and announces a permanent donation to the goddess Neith, ‘Mistress of the Floods’, out of the customs dues received in the town of Thonis- Heracleion and out of the taxes on Greek trade in the town of Naukratis. ISBN 978-1-905905-23-2 Published by the Oxford Centre for Maritime Archaeology at the School of Archaeology, University of Oxford Anne-Sophie von Bomhard The Decree of Saïs The Stelae of Thonis-Heracleion and Naukratis Oxford Centre for Maritime Archaeology Monograph Series Series editors: Franck Goddio and Damian Robinson 1 Topography and Excavation of Heracleion-Thonis and East Canopus (1996–2006) by Franck Goddio 2 Geoarchaeology by Jean-Daniel Stanley et al 3 The Naos of the Decades by Anne-Sophie von Bomhard 4 La stèle de Ptolémée VIII Évergète II à Héracléion by Christophe Thiers 5 Alexandria and the North-Western Delta edited by Damian Robinson and Andrew Wilson 6 Maritime Archaeology and Ancient Trade in the Mediterranean edited by Damian Robinson and Andrew Wilson The Underwater Archaeology of the Canopic Region in Egypt The Decree of Saïs The Stelae of Thonis-Heracleion and Naukratis by Anne-Sophie von Bomhard Oxford Centre for Maritime Archaeology: Monograph 7 School of Archaeology, University of Oxford 2012 All rights reserved. -

Dentists, Dentistry and Dental Diseases in Ancient Egypt
DENTISTS, DENTISTRY AND DENTAL DISEASES IN ANCIENT EGYPT by CASPARUS JOHANNES GREEFF Submitted in accordance with the requirements for the degree of MASTER OF ARTS in the subject ANCIENT AND NEAR EASTERN STUDIES at the UNIVERSITY OF SOUTH AFRICA SUPERVISOR: PROFESSOR P S VERMAAK JULY 2013 DEDICATION I wish to dedicate this work to special people who have been instrumental in making my life what it is today and who are no longer with me. In loving memory then to: My mother (1920- 1962) who instilled love in me; My father (1910-1999) who instilled the love of books in me which ultimately also became my life; My only sister Marié (1939-2010) who showed me what a life of pure altruism is; My only son Willem (1976-2003) whose untimely death underlined the transience of life. I miss them all and I so wish them to have shared some special moments of my life with me, but alas, too late. To the living: I dedicate this dissertation to my three daughters (Tanya, Brittani & Romi) whose respect and unrelenting love I humbly relish. To three grandchildren (JP, Demi & Alexa-Jade) who are God’s gift to the elder: it will be the coolest thing ever if I could inspire them to ever explore the deep well of unconscious cerebration (Henry James 1843 - 1916). Lastly, I take pleasure to also dedicate this work to my previous promoters; Professors W S Boshoff and M le Roux, who squarely put me on the endless road of acquiring knowledge – the more you know, the more you know how little you know.