Diagnosis and Treatment of Digoxin Toxicity
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Drug Interactions of Some Commonly Used Drugs in Dermatology
Table Drug interactions of some commonly used drugs in dermatology M. J. Cyriac Department of Dermatology and Venereology, Medical College, Kottayam, India. Address for correspondence: Dr. M. J. Cyriac, Professor and Head, Department of Dermatology and Venereology, Medical College, Kottayam, India. E-mail: [email protected] Drug interactions leading to serious adverse effects are alternative medicines or food should also be borne in to be cautiously watched for when multiple drugs are mind.2 Increased risk of drug induced toxicity or used simultaneously.1 It is important for the physician therapeutic failure can occur when a new drug is added to be aware of these interactions. Although in many to a treatment regimen. It is impossible to remember instances the adverse interaction does not reach a all possible drug interactions. A ready to refer checklist magnitude of recognizable clinical expression, rarely is useful as a handy reference. it can result in a serious adverse outcome. Some of the commonly used drugs in dermatology and Adverse drug interactions may lead to increased their interactions, resultant clinical effect and possible toxicity, decreased efficacy or both. The possibility of underlying mechanisms are given in Table 1. Table 2 lists interaction with non-prescription drugs, herbal or the drugs with their relative risk for inducing interactions. Table 1: Drug interactions of some commonly used drugs Drug Interacting drug Adverse effect Remarks Erythromycin/Clarithromycin Theophylline Theophylline toxicity Precipitates -

The Pharmacology of Amiodarone and Digoxin As Antiarrhythmic Agents
Part I Anaesthesia Refresher Course – 2017 University of Cape Town The Pharmacology of Amiodarone and Digoxin as Antiarrhythmic Agents Dr Adri Vorster UCT Department of Anaesthesia & Perioperative Medicine The heart contains pacemaker, conduction and contractile tissue. Cardiac arrhythmias are caused by either enhancement or depression of cardiac action potential generation by pacemaker cells, or by abnormal conduction of the action potential. The pharmacological treatment of arrhythmias aims to achieve restoration of a normal rhythm and rate. The resting membrane potential of myocytes is around -90 mV, with the inside of the membrane more negative than the outside. The main extracellular ions are Na+ and Cl−, with K+ the main intracellular ion. The cardiac action potential involves a change in voltage across the cell membrane of myocytes, caused by movement of charged ions across the membrane. This voltage change is triggered by pacemaker cells. The action potential is divided into 5 phases (figure 1). Phase 0: Rapid depolarisation Duration < 2ms Threshold potential must be reached (-70 mV) for propagation to occur Rapid positive charge achieved as a result of increased Na+ conductance through voltage-gated Na+ channels in the cell membrane Phase 1: Partial repolarisation Closure of Na+ channels K+ channels open and close, resulting in brief outflow of K+ and a more negative membrane potential Phase 2: Plateau Duration up to 150 ms Absolute refractory period – prevents further depolarisation and myocardial tetany Result of Ca++ influx -

Dabigatran Amoxicillin Clavulanate IV Treatment in the Community
BEST PRACTICE 38 SEPTEMBER 2011 Dabigatran Amoxicillin clavulanate bpac nz IV treatment in the community better medicin e Editor-in-chief We would like to acknowledge the following people for Professor Murray Tilyard their guidance and expertise in developing this edition: Professor Carl Burgess, Wellington Editor Dr Gerry Devlin, Hamilton Rebecca Harris Dr John Fink, Christchurch Dr Lisa Houghton, Dunedin Programme Development Dr Rosemary Ikram, Christchurch Mark Caswell Dr Sisira Jayathissa, Wellington Rachael Clarke Kate Laidlow, Rotorua Peter Ellison Dr Hywel Lloyd, GP Reviewer, Dunedin Julie Knight Associate Professor Stewart Mann, Wellington Noni Richards Dr Richard Medlicott, Wellington Dr AnneMarie Tangney Dr Alan Panting, Nelson Dr Sharyn Willis Dr Helen Patterson, Dunedin Dave Woods David Rankin, Wellington Report Development Dr Ralph Stewart, Auckland Justine Broadley Dr Neil Whittaker, GP Reviewer, Nelson Tim Powell Dr Howard Wilson, Akaroa Design Michael Crawford Best Practice Journal (BPJ) ISSN 1177-5645 Web BPJ, Issue 38, September 2011 Gordon Smith BPJ is published and owned by bpacnz Ltd Management and Administration Level 8, 10 George Street, Dunedin, New Zealand. Jaala Baldwin Bpacnz Ltd is an independent organisation that promotes health Kaye Baldwin care interventions which meet patients’ needs and are evidence Tony Fraser based, cost effective and suitable for the New Zealand context. Kyla Letman We develop and distribute evidence based resources which describe, facilitate and help overcome the barriers to best Clinical Advisory Group practice. Clive Cannons nz Michele Cray Bpac Ltd is currently funded through contracts with PHARMAC and DHBNZ. Margaret Gibbs nz Dr Rosemary Ikram Bpac Ltd has five shareholders: Procare Health, South Link Health, General Practice NZ, the University of Otago and Pegasus Dr Cam Kyle Health. -

DRI® Digoxin Assay
DRI® Digoxin Assay For In Vitro Diagnostic Use 1669 (25 mL, 8 mL Kit) 1669-A (25 mL, 8 mL Kit) Intended Use Reagent Preparation and Storage The DRI® Digoxin Assay is intended for the quantitative determination of digoxin in human The reagents are ready for use. No reagent preparation is required. All assay components, serum or plasma. when stored properly at 2-8°C, are stable until the expiration date indicated on the label. Summary and Explanation of the Test Specimen Collection and Handling Digitalis is known to have the ability to increase the force and velocity of myocardial Pharmacokinetic factors, such as dosage form, mode of administration, concomitant drug therapy contraction.1 Digoxin is one of the most commonly used forms of digitalis in the treatment as well as the patient’s clinical condition may influence the correct time of sample collection.2,3 For of congestive heart failure and arrhythmia such as atrial fibrillation and atrial flutter. The reliable interpretation of results, a serum specimen should be collected 6 to 8 hours following therapeutic range of digoxin is narrow. Futhermore, individual differences in drug absorption, the last oral dose of digoxin. Either serum or heparin and EDTA treated plasma samples can distribution, metabolism, and excretion as well as factors such as concurrent use of other drugs be used with the assay. Samples may be stored refrigerated at 2-8°C for up to 7 days or frozen and illness can also alter the serum concentration in response to a given dosage. Monitoring (-20°C) for up to 6 months. -

Report on the National Seminar on Radioimmunoassays Radiation Medicine Centre, B.A.R.C
REPORT ON THE NATIONAL SEMINAR ON RADIOIMMUNOASSAYS JANUARY 16-20, 1978 RADIATION MEDICINE CENTRE, B.A.R.C. DEPARTMENT OF ATOMIC ENERGY AND WORLD HEALTH ORGANISATION REPORT ON THE NATIONAL SEMINAR ON RADIOIMMUNOASSAYS JANUARY 16—20, 1978 RADIATION MEDICINE CENTRE, BARC TATA MEMORIAL HOSPITAL ANNEXE JERBAI WADIA ROAD, PAREL BOMBAY 400 012 ORGANISED UNDER THE AUSPICES OF THE DEPARTMENT OF ATOMIC ENERGY & WORLD HEALTH ORGANISATION CONTENTS Page Preface .. .. .. .. .. .. .. 3 Administrative Responsibilities .. .. .. .. 6 List of Participants 7 Programme .. .. .. .. .. .. .. 11 Basic Requirements of RIA in India .. .. .. 14 a. Radioisotopes for RIA's .. .. .. .. .. 15 b. Kits for RIA 17 c. Availability of Antibodies 19 d. National Pituitary Agency .. .. .. .. 20 e. Well-counter for RIA 21 f. Radiation Protection Aspects of RIA 23 Review of Discussion following the Session .. .. 26 State of Art of RIA's in India 28 Trigger Sessions 36 a. Quality Control of RIA's 37 b. Usefulness and limitations of RIA's in clinical diagnosis 39 c. RIA's in tropical diseases •. .. .. .. .. 42 d. Centralised assay services .. .. .. .. 44 Recommendations and Guidelines .. .. .. .. 46 Backword 51 Bibliography . .. .. .. .. .. .. 53 PREFACE This National Seminar on Radioimmunoassays was the second National Seminar jointly sponsored by Department of Atomic Energy and World Health Organisation and organised at Radiation Medicine Centre. The first one on 'Nuclear Medicine in India' was held in December 1976. The present Seminar on Radioimmunoassays was distinguished by the participation of Dr. Rosalyn Yalow, Nobel Laureate in Medicine for 1977. She, along with Dr. Solomon A. Berson, discovered the technique of Radioimmunoassay and nurtured it through the early years with hard and meticulous work to establish its usefulness in medical science. -
Full Prescribing Information Warning: Suicidal Thoughts
tablets (SR) BUPROPION hydrochloride extended-release HIGHLIGHTS OF PRESCRIBING INFORMATION anxiety, and panic, as well as suicidal ideation, suicide attempt, and completed suicide. Observe hydrochloride extended-release tablets (SR) was reported. However, the symptoms persisted in some Table 3. Adverse Reactions Reported by at Least 1% of Subjects on Active Treatment and at a tablets (SR) may be necessary when coadministered with ritonavir, lopinavir, or efavirenz [see Clinical These highlights do not include all the information needed to use bupropion hydrochloride patients attempting to quit smoking with Bupropion hydrochloride extended-release tablets, USP cases; therefore, ongoing monitoring and supportive care should be provided until symptoms resolve. Greater Frequency than Placebo in the Comparator Trial Pharmacology (12.3)] but should not exceed the maximum recommended dose. extended-release tablets (SR) safely and effectively. See full prescribing information for (SR) for the occurrence of such symptoms and instruct them to discontinue Bupropion hydrochloride Carbamazepine, Phenobarbital, Phenytoin: While not systematically studied, these drugs extended-release tablets, USP (SR) and contact a healthcare provider if they experience such adverse The neuropsychiatric safety of Bupropion hydrochloride extended-release tablets (SR) was evaluated in Bupropion Bupropion may induce the metabolism of bupropion and may decrease bupropion exposure [see Clinical bupropion hydrochloride extended-release tablets (SR). Nicotine events. (5.2) a randomized, double-blind, active-and placebo-controlled study that included patients without a history Hydrochloride Hydrochloride Pharmacology (12.3)]. If bupropion is used concomitantly with a CYP inducer, it may be necessary Transdermal BUPROPION hydrochloride extended-release tablets (SR), for oral use • Seizure risk: The risk is dose-related. -

Spectrum of Digoxin-Induced Ocular Toxicity: a Case Report and Literature Review Delphine Renard1*, Eve Rubli2, Nathalie Voide3, François‑Xavier Borruat3 and Laura E
Renard et al. BMC Res Notes (2015) 8:368 DOI 10.1186/s13104-015-1367-6 CASE REPORT Open Access Spectrum of digoxin-induced ocular toxicity: a case report and literature review Delphine Renard1*, Eve Rubli2, Nathalie Voide3, François‑Xavier Borruat3 and Laura E. Rothuizen1 Abstract Background: Digoxin intoxication results in predominantly digestive, cardiac and neurological symptoms. This case is outstanding in that the intoxication occurred in a nonagenarian and induced severe, extensively documented visual symptoms as well as dysphagia and proprioceptive illusions. Moreover, it went undiagnosed for a whole month despite close medical follow-up, illustrating the difficulty in recognizing drug-induced effects in a polymorbid patient. Case presentation: Digoxin 0.25 mg qd for atrial fibrillation was prescribed to a 91-year-old woman with an esti‑ mated creatinine clearance of 18 ml/min. Over the following 2–3 weeks she developed nausea, vomiting and dyspha‑ gia, snowy and blurry vision, photopsia, dyschromatopsia, aggravated pre-existing formed visual hallucinations and proprioceptive illusions. She saw her family doctor twice and visited the eye clinic once until, 1 month after starting digoxin, she was admitted to the emergency room. Intoxication was confirmed by a serum digoxin level of 5.7 ng/ml (reference range 0.8–2 ng/ml). After stopping digoxin, general symptoms resolved in a few days, but visual complaints persisted. Examination by the ophthalmologist revealed decreased visual acuity in both eyes, 4/10 in the right eye (OD) and 5/10 in the left eye (OS), decreased color vision as demonstrated by a score of 1/13 in both eyes (OU) on Ishihara pseudoisochromatic plates, OS cataract, and dry age-related macular degeneration (ARMD). -
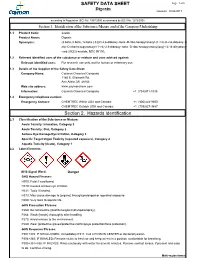
Digoxin SAFETY DATA SHEET Section 2. Hazards Identification
SAFETY DATA SHEET Page: 1 of 6 Digoxin Revision: 08/24/2017 according to Regulation (EC) No. 1907/2006 as amended by (EC) No. 1272/2008 Section 1. Identification of the Substance/Mixture and of the Company/Undertaking 1.1 Product Code: 22266 Product Name: Digoxin Synonyms: (3.beta.,5.beta.,12.beta.)-3-[(O-2,6-dideoxy-.beta.-D-ribo-hexopyranosyl-(1->4)-O-2,6-dideoxy-.b eta.-D-ribo-hexopyranosyl-(1->4)-2,6-dideoxy-.beta.-D-ribo-hexopyranosyl)oxy]-12,14-dihydroxy- card-20(22)-enolide; NSC 95100; 1.2 Relevant identified uses of the substance or mixture and uses advised against: Relevant identified uses: For research use only, not for human or veterinary use. 1.3 Details of the Supplier of the Safety Data Sheet: Company Name: Cayman Chemical Company 1180 E. Ellsworth Rd. Ann Arbor, MI 48108 Web site address: www.caymanchem.com Information: Cayman Chemical Company +1 (734)971-3335 1.4 Emergency telephone number: Emergency Contact: CHEMTREC Within USA and Canada: +1 (800)424-9300 CHEMTREC Outside USA and Canada: +1 (703)527-3887 Section 2. Hazards Identification 2.1 Classification of the Substance or Mixture: Acute Toxicity: Inhalation, Category 3 Acute Toxicity: Oral, Category 2 Serious Eye Damage/Eye Irritation, Category 2 Specific Target Organ Toxicity (repeated exposure), Category 2 Aquatic Toxicity (Acute), Category 1 2.2 Label Elements: GHS Signal Word: Danger GHS Hazard Phrases: H300: Fatal if swallowed. H319: Causes serious eye irritation. H331: Toxic if inhaled. H373: May cause damage to {organs} through prolonged or repeated exposure. H400: Very toxic to aquatic life. -

Digoxin Toxicity 1
Chronic Digoxin Toxicity Reviewers: Shawn M. Varney, Authors: Matthew Riddle, MD, Mel Otten, MD MD Target Audience: Emergency Medicine Residents (junior and senior level postgraduate learners), Medical Students Primary Learning Objectives: 1. Recognize signs and symptoms of digoxin toxicity 2. Order appropriate diagnostic studies for evaluation of digoxin toxicity 3. Appropriately interpret ECG 4. Administer digoxin-specific antibody fragments (DSFab) 5. Recognize acute kidney injury as a precipitating factor of toxicity, and treat acute kidney injury appropriately 6. Select an appropriate disposition for patient with digoxin toxicity Secondary Learning Objectives: detailed technical/behavioral goals, didactic points 1. Develop independent differential diagnosis in setting of leading information from the nurse 2. Describe the mechanism of digoxin toxicity and treatment, DSFab 3. Use appropriate dosing strategy for DSFab administration Critical actions checklist: 1. Order a basic metabolic panel 2. Order a digoxin level 3. Obtain ECG 4. Provide volume resuscitation for acute kidney injury 5. Administer digoxin antibody fragments 6. Consult Poison Center/Toxicologist 7. Admit to the MICU Environment: Emergency Department treatment area 1. Room Set Up – ED critical care area a. Manikin Set Up – Mid or high fidelity simulator b. Props – Standard ED equipment 2. Distractors – ED noise, alarming monitor For Examiner Only CASE SUMMARY SYNOPSIS OF HISTORY/ Scenario Background The setting is an urban emergency department. The patient is a 63-year-old male with a history of atrial fibrillation, HTN, and CHF brought to the emergency department by EMS for nausea and vomiting for the past four days and confusion that began shortly before arrival. PMHx: atrial fibrillation, HTN, and CHF PSHx: None Medications: ASA 81 mg once daily, Digoxin 250 mcg once daily, Amlodipine 10 mg once daily, Lasix 20 mg twice daily, warfarin 5 mg once daily Allergies: NKDA SocHx: smokes ½ ppd for 40 years. -

Guideline for Preoperative Medication Management
Guideline: Preoperative Medication Management Guideline for Preoperative Medication Management Purpose of Guideline: To provide guidance to physicians, advanced practice providers (APPs), pharmacists, and nurses regarding medication management in the preoperative setting. Background: Appropriate perioperative medication management is essential to ensure positive surgical outcomes and prevent medication misadventures.1 Results from a prospective analysis of 1,025 patients admitted to a general surgical unit concluded that patients on at least one medication for a chronic disease are 2.7 times more likely to experience surgical complications compared with those not taking any medications. As the aging population requires more medication use and the availability of various nonprescription medications continues to increase, so does the risk of polypharmacy and the need for perioperative medication guidance.2 There are no well-designed trials to support evidence-based recommendations for perioperative medication management; however, general principles and best practice approaches are available. General considerations for perioperative medication management include a thorough medication history, understanding of the medication pharmacokinetics and potential for withdrawal symptoms, understanding the risks associated with the surgical procedure and the risks of medication discontinuation based on the intended indication. Clinical judgement must be exercised, especially if medication pharmacokinetics are not predictable or there are significant risks associated with inappropriate medication withdrawal (eg, tolerance) or continuation (eg, postsurgical infection).2 Clinical Assessment: Prior to instructing the patient on preoperative medication management, completion of a thorough medication history is recommended – including all information on prescription medications, over-the-counter medications, “as needed” medications, vitamins, supplements, and herbal medications. Allergies should also be verified and documented. -
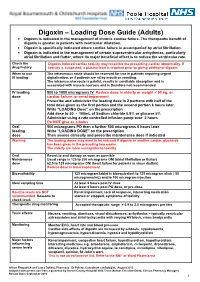
Digoxin – Loading Dose Guide (Adults) Digoxin Is Indicated in the Management of Chronic Cardiac Failure
Digoxin – Loading Dose Guide (Adults) Digoxin is indicated in the management of chronic cardiac failure. The therapeutic benefit of digoxin is greater in patients with ventricular dilatation. Digoxin is specifically indicated where cardiac failure is accompanied by atrial fibrillation. Digoxin is indicated in the management of certain supraventricular arrhythmias, particularly atrial fibrillation and flutter, where its major beneficial effect is to reduce the ventricular rate. Check the Digoxin-induced cardiac toxicity may resemble the presenting cardiac abnormality. If drug history toxicity is suspected, a plasma level is required prior to giving additional digoxin. When to use The intravenous route should be reserved for use in patients requiring urgent IV loading digitalisation, or if patients are nil by mouth or vomiting. The intramuscular route is painful, results in unreliable absorption and is associated with muscle necrosis and is therefore not recommended. IV loading 500 to 1000 micrograms IV Reduce dose in elderly or weight < 50 kg, or dose cardiac failure, or renal impairment Prescribe and administer the loading dose in 2 portions with half of the total dose given as the first portion and the second portion 6 hours later. Write “LOADING Dose” on the prescription Add dose to 50 - 100mL of Sodium chloride 0.9% or glucose 5% Administer using a rate controlled infusion pump over 2 hours Do NOT give as a bolus Oral 500 micrograms PO then a further 500 micrograms 6 hours later loading Write “LOADING DOSE” on the prescription dose Then assess clinically and prescribe maintenance dose if indicated Warning The loading doses may need to be reduced if digoxin or another cardiac glycoside has been given in the preceding two weeks. -

Quinidine, Beta-Blockers, Diphenylhydantoin, Bretylium *
Pharmacology of Antiarrhythmics: Quinidine, Beta-Blockers, Diphenylhydantoin, Bretylium * ALBERT J. WASSERMAN, M.D. Professor of Medicine, Chairman, Division of Clinical Pharmacology, Medical College of Virginia, Health Sciences Division of Virginia Commonwealth University, Richmond, Virginia JACK D. PROCTOR, M.D. Assistant Professor of Medicine, Medical College of Virginia, Health Sciences Division of Virginia Commonwealth University, Richmond, Virginia The electrophysiologic effects of the antiar adequate, controlled clinical comparisons are virtu rhythmic drugs, presented elsewhere in this sym ally nonexistent. posium, form only one of the bases for the selec A complete presentation of the non-electro tion of a therapeutic agent in any given clinical physiologic pharmacology would include the follow situation. The final choice depends at least on the ing considerations: following factors: 1. Absorption and peak effect times 1. The specific arrhythmia 2. Biotransformation 2. Underlying heart disease, if any 3. Rate of elimination or half-life (t1d 3. The degree of compromise of the circula 4. Drug interactions tion, if any 5. Toxicity 4. The etiology of the arrhythmia 6. Clinical usefulness 5. The efficacy of the drug for that arrhythmia 7. Therapeutic drug levels due to that etiology 8. Dosage schedules 6. The toxicity of the drug, especially in the As all of the above data cannot be presented in given patient with possible alterations in the limited space available, only selected items will volume of distribution, biotransformation, be discussed. Much of the preceding information and excretion is available, however, in standard texts ( 1 7, 10). 7. The electrophysiologic effects of the drug (See Addendum 1) 8. The routes and frequency of administration Quinidine.