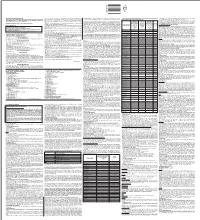
Treatment for Calcium Channel Blocker Poisoning: a Systematic Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mapping the Dissociated Body
Lesley University DigitalCommons@Lesley Graduate School of Arts and Social Sciences Expressive Therapies Capstone Theses (GSASS) Spring 5-16-2020 Mapping the Dissociated Body Elizabeth Hough [email protected] Follow this and additional works at: https://digitalcommons.lesley.edu/expressive_theses Part of the Social and Behavioral Sciences Commons Recommended Citation Hough, Elizabeth, "Mapping the Dissociated Body" (2020). Expressive Therapies Capstone Theses. 239. https://digitalcommons.lesley.edu/expressive_theses/239 This Thesis is brought to you for free and open access by the Graduate School of Arts and Social Sciences (GSASS) at DigitalCommons@Lesley. It has been accepted for inclusion in Expressive Therapies Capstone Theses by an authorized administrator of DigitalCommons@Lesley. For more information, please contact [email protected], [email protected]. Running Head: MAPPING THE DISSOCIATED BODY 1 Mapping the Dissociated Body Elizabeth Hough Lesley University Running Head: MAPPING THE DISSOCIATED BODY 2 Abstract This capstone thesis explored the use of body mapping and body scans as a tool for assessing and tracking somatic dissociation and embodiment. The researcher utilized a client- centered approach and mindfulness-based interventions and theory to ground the work with the clients. While there were a variety of questionnaire-based tools for assessing dissociation with clients, many of them were lacking in the somatic component of dissociation. The available assessments were also exclusively self-reported and written or verbal, which had the potential to result in biased reporting. Clients may have also struggled to identify their level of somatic dissociation due to an inherent disconnection or dismissal of their somatic experience. This research described two case studies in which body scans and body mapping were utilized as a method to assess and track the client’s level of body dissociation and embodiment. -

The Pharmacology of Amiodarone and Digoxin As Antiarrhythmic Agents
Part I Anaesthesia Refresher Course – 2017 University of Cape Town The Pharmacology of Amiodarone and Digoxin as Antiarrhythmic Agents Dr Adri Vorster UCT Department of Anaesthesia & Perioperative Medicine The heart contains pacemaker, conduction and contractile tissue. Cardiac arrhythmias are caused by either enhancement or depression of cardiac action potential generation by pacemaker cells, or by abnormal conduction of the action potential. The pharmacological treatment of arrhythmias aims to achieve restoration of a normal rhythm and rate. The resting membrane potential of myocytes is around -90 mV, with the inside of the membrane more negative than the outside. The main extracellular ions are Na+ and Cl−, with K+ the main intracellular ion. The cardiac action potential involves a change in voltage across the cell membrane of myocytes, caused by movement of charged ions across the membrane. This voltage change is triggered by pacemaker cells. The action potential is divided into 5 phases (figure 1). Phase 0: Rapid depolarisation Duration < 2ms Threshold potential must be reached (-70 mV) for propagation to occur Rapid positive charge achieved as a result of increased Na+ conductance through voltage-gated Na+ channels in the cell membrane Phase 1: Partial repolarisation Closure of Na+ channels K+ channels open and close, resulting in brief outflow of K+ and a more negative membrane potential Phase 2: Plateau Duration up to 150 ms Absolute refractory period – prevents further depolarisation and myocardial tetany Result of Ca++ influx -

Dabigatran Amoxicillin Clavulanate IV Treatment in the Community
BEST PRACTICE 38 SEPTEMBER 2011 Dabigatran Amoxicillin clavulanate bpac nz IV treatment in the community better medicin e Editor-in-chief We would like to acknowledge the following people for Professor Murray Tilyard their guidance and expertise in developing this edition: Professor Carl Burgess, Wellington Editor Dr Gerry Devlin, Hamilton Rebecca Harris Dr John Fink, Christchurch Dr Lisa Houghton, Dunedin Programme Development Dr Rosemary Ikram, Christchurch Mark Caswell Dr Sisira Jayathissa, Wellington Rachael Clarke Kate Laidlow, Rotorua Peter Ellison Dr Hywel Lloyd, GP Reviewer, Dunedin Julie Knight Associate Professor Stewart Mann, Wellington Noni Richards Dr Richard Medlicott, Wellington Dr AnneMarie Tangney Dr Alan Panting, Nelson Dr Sharyn Willis Dr Helen Patterson, Dunedin Dave Woods David Rankin, Wellington Report Development Dr Ralph Stewart, Auckland Justine Broadley Dr Neil Whittaker, GP Reviewer, Nelson Tim Powell Dr Howard Wilson, Akaroa Design Michael Crawford Best Practice Journal (BPJ) ISSN 1177-5645 Web BPJ, Issue 38, September 2011 Gordon Smith BPJ is published and owned by bpacnz Ltd Management and Administration Level 8, 10 George Street, Dunedin, New Zealand. Jaala Baldwin Bpacnz Ltd is an independent organisation that promotes health Kaye Baldwin care interventions which meet patients’ needs and are evidence Tony Fraser based, cost effective and suitable for the New Zealand context. Kyla Letman We develop and distribute evidence based resources which describe, facilitate and help overcome the barriers to best Clinical Advisory Group practice. Clive Cannons nz Michele Cray Bpac Ltd is currently funded through contracts with PHARMAC and DHBNZ. Margaret Gibbs nz Dr Rosemary Ikram Bpac Ltd has five shareholders: Procare Health, South Link Health, General Practice NZ, the University of Otago and Pegasus Dr Cam Kyle Health. -

204508S000lbl.Pdf
HIGHLIGHTS OF PRESCRIBING INFORMATION These highlights do not include all the information needed to use ____________________CONTRAINDICATIONS____________________ CLINOLIPID injection safely and effectively. See full prescribing • Known hypersensitivity to egg and soybean proteins, the lipid emulsion information for CLINOLIPID injection. and/or excipients. (4) • Severe hyperlipidemia or severe disorders of lipid metabolism. (4) CLINOLIPID (Lipid Injectable Emulsion) for intravenous use Initial U.S. Approval: 1975 ________________WARNINGS AND PRECAUTIONS_______________ • Preterm infants have poor clearance of intravenous lipid emulsion. (5.1) WARNING: DEATH IN PRETERM INFANTS • Monitor for signs or symptoms of hypersensitivity reactions. (5.2) See full prescribing information for complete boxed warning • Monitor for signs and symptoms of infection, fat overload, and refeeding • Deaths in preterm infants have been reported in literature. (5.1, complications. (5.3, 5.4, 5.5) 8.4) • Frequent clinical and laboratory determinations are necessary. (5.6) • Autopsy findings included intravascular fat accumulation in the lungs. (5.1, 8.4) __________________ADVERSE REACTIONS__________________ • Preterm and low birth weight infants have poor clearance of The most common (5%) adverse drug reactions from clinical trials were intravenous lipid emulsion and increased free fatty acid plasma nausea and vomiting, hyperlipidemia, hyperglycemia, hypoproteinemia and levels following lipid emulsion infusion. (5.1, 8.4) abnormal liver function tests. (6.1) __________________INDICATIONS AND USAGE___________________ To report SUSPECTED ADVERSE REACTIONS, contact Baxter CLINOLIPID injection is a lipid emulsion indicated in adults for parenteral Healthcare at 1-866-888-2472 or FDA at 1-800-FDA-1088 or nutrition providing a source of calories and essential fatty acids when oral or www.fda.gov/medwatch enteral nutrition is not possible, insufficient, or contraindicated. -
Full Prescribing Information Warning: Suicidal Thoughts
tablets (SR) BUPROPION hydrochloride extended-release HIGHLIGHTS OF PRESCRIBING INFORMATION anxiety, and panic, as well as suicidal ideation, suicide attempt, and completed suicide. Observe hydrochloride extended-release tablets (SR) was reported. However, the symptoms persisted in some Table 3. Adverse Reactions Reported by at Least 1% of Subjects on Active Treatment and at a tablets (SR) may be necessary when coadministered with ritonavir, lopinavir, or efavirenz [see Clinical These highlights do not include all the information needed to use bupropion hydrochloride patients attempting to quit smoking with Bupropion hydrochloride extended-release tablets, USP cases; therefore, ongoing monitoring and supportive care should be provided until symptoms resolve. Greater Frequency than Placebo in the Comparator Trial Pharmacology (12.3)] but should not exceed the maximum recommended dose. extended-release tablets (SR) safely and effectively. See full prescribing information for (SR) for the occurrence of such symptoms and instruct them to discontinue Bupropion hydrochloride Carbamazepine, Phenobarbital, Phenytoin: While not systematically studied, these drugs extended-release tablets, USP (SR) and contact a healthcare provider if they experience such adverse The neuropsychiatric safety of Bupropion hydrochloride extended-release tablets (SR) was evaluated in Bupropion Bupropion may induce the metabolism of bupropion and may decrease bupropion exposure [see Clinical bupropion hydrochloride extended-release tablets (SR). Nicotine events. (5.2) a randomized, double-blind, active-and placebo-controlled study that included patients without a history Hydrochloride Hydrochloride Pharmacology (12.3)]. If bupropion is used concomitantly with a CYP inducer, it may be necessary Transdermal BUPROPION hydrochloride extended-release tablets (SR), for oral use • Seizure risk: The risk is dose-related. -

Spectrum of Digoxin-Induced Ocular Toxicity: a Case Report and Literature Review Delphine Renard1*, Eve Rubli2, Nathalie Voide3, François‑Xavier Borruat3 and Laura E
Renard et al. BMC Res Notes (2015) 8:368 DOI 10.1186/s13104-015-1367-6 CASE REPORT Open Access Spectrum of digoxin-induced ocular toxicity: a case report and literature review Delphine Renard1*, Eve Rubli2, Nathalie Voide3, François‑Xavier Borruat3 and Laura E. Rothuizen1 Abstract Background: Digoxin intoxication results in predominantly digestive, cardiac and neurological symptoms. This case is outstanding in that the intoxication occurred in a nonagenarian and induced severe, extensively documented visual symptoms as well as dysphagia and proprioceptive illusions. Moreover, it went undiagnosed for a whole month despite close medical follow-up, illustrating the difficulty in recognizing drug-induced effects in a polymorbid patient. Case presentation: Digoxin 0.25 mg qd for atrial fibrillation was prescribed to a 91-year-old woman with an esti‑ mated creatinine clearance of 18 ml/min. Over the following 2–3 weeks she developed nausea, vomiting and dyspha‑ gia, snowy and blurry vision, photopsia, dyschromatopsia, aggravated pre-existing formed visual hallucinations and proprioceptive illusions. She saw her family doctor twice and visited the eye clinic once until, 1 month after starting digoxin, she was admitted to the emergency room. Intoxication was confirmed by a serum digoxin level of 5.7 ng/ml (reference range 0.8–2 ng/ml). After stopping digoxin, general symptoms resolved in a few days, but visual complaints persisted. Examination by the ophthalmologist revealed decreased visual acuity in both eyes, 4/10 in the right eye (OD) and 5/10 in the left eye (OS), decreased color vision as demonstrated by a score of 1/13 in both eyes (OU) on Ishihara pseudoisochromatic plates, OS cataract, and dry age-related macular degeneration (ARMD). -

Liposomes to Augment Dialysis in Preclinical Models: a Structured Review
pharmaceutics Review Liposomes to Augment Dialysis in Preclinical Models: A Structured Review Kevin Hart 1,*, Martyn Harvey 2, Mingtan Tang 3 , Zimei Wu 3 and Grant Cave 1 1 Intensive Care Unit, Hawkes Bay District Health Board, Hastings 9014, New Zealand; [email protected] 2 Waikato Hospital Emergency Department, Waikato District Health Board, Hamilton 3240, New Zealand; [email protected] 3 Faculty of Medicine and Health Sciences, School of Pharmacy, University of Auckland, Auckland 1023, New Zealand; [email protected] (M.T.); [email protected] (Z.W.) * Correspondence: [email protected] Abstract: In recent years, a number of groups have been investigating the use of “empty” liposomes with no drug loaded as scavengers both for exogenous intoxicants and endogenous toxic molecules. Preclinical trials have demonstrated that repurposing liposomes to sequester such compounds may prove clinically useful. The use of such “empty” liposomes in the dialysate during dialysis avoids recognition by complement surveillance, allowing high doses of liposomes to be used. The “reach” of dialysis may also be increased to molecules that are not traditionally dialysable. We aim to review the current literature in this area with the aims of increasing awareness and informing further research. A structured literature search identified thirteen papers which met the inclusion criteria. Augmenting the extraction of ammonia in hepatic failure with pH-gradient liposomes with acidic centres in peritoneal dialysis is the most studied area, with work progressing toward phase one trials. Liposomes used to augment the removal of exogenous intoxicants and protein- Citation: Hart, K.; Harvey, M.; Tang, bound uraemic and hepatic toxins that accumulate in these organ failures and liposome-supported M.; Wu, Z.; Cave, G. -

XELJANZ (Tofacitinib)
HIGHLIGHTS OF PRESCRIBING INFORMATION Psoriatic Arthritis (in combination with nonbiologic DMARDs) These highlights do not include all the information needed to use XELJANZ 5 mg twice daily or XELJANZ XR 11 mg once daily. (2.2) XELJANZ/XELJANZ XR safely and effectively. See full prescribing Recommended dosage in patients with moderate and severe renal information for XELJANZ. impairment or moderate hepatic impairment is XELJANZ 5 mg once daily. (2, 8.7, 8.8) ® XELJANZ (tofacitinib) tablets, for oral use Ulcerative Colitis ® XELJANZ XR (tofacitinib) extended-release tablets, for oral use XELJANZ 10 mg twice daily for at least 8 weeks; then 5 or 10 mg Initial U.S. Approval: 2012 twice daily. Discontinue after 16 weeks of 10 mg twice daily, if adequate therapeutic benefit is not achieved. Use the lowest effective dose to WARNING: SERIOUS INFECTIONS AND MALIGNANCY maintain response. (2.3) See full prescribing information for complete boxed warning. Recommended dosage in patients with moderate and severe renal impairment or moderate hepatic impairment: half the total daily dosage Serious infections leading to hospitalization or death, including recommended for patients with normal renal and hepatic function. (2, 8.7, tuberculosis and bacterial, invasive fungal, viral, and other 8.8) opportunistic infections, have occurred in patients receiving Dosage Adjustment XELJANZ. (5.1) See the full prescribing information for dosage adjustments by indication If a serious infection develops, interrupt XELJANZ/XELJANZ XR for patients receiving CYP2C19 and/or CYP3A4 inhibitors; in patients until the infection is controlled. (5.1) with moderate or severe renal impairment or moderate hepatic Prior to starting XELJANZ/XELJANZ XR, perform a test for latent impairment; and patients with lymphopenia, neutropenia, or anemia. -

1: Gastro-Intestinal System
1 1: GASTRO-INTESTINAL SYSTEM Antacids .......................................................... 1 Stimulant laxatives ...................................46 Compound alginate products .................. 3 Docuate sodium .......................................49 Simeticone ................................................... 4 Lactulose ....................................................50 Antimuscarinics .......................................... 5 Macrogols (polyethylene glycols) ..........51 Glycopyrronium .......................................13 Magnesium salts ........................................53 Hyoscine butylbromide ...........................16 Rectal products for constipation ..........55 Hyoscine hydrobromide .........................19 Products for haemorrhoids .................56 Propantheline ............................................21 Pancreatin ...................................................58 Orphenadrine ...........................................23 Prokinetics ..................................................24 Quick Clinical Guides: H2-receptor antagonists .......................27 Death rattle (noisy rattling breathing) 12 Proton pump inhibitors ........................30 Opioid-induced constipation .................42 Loperamide ................................................35 Bowel management in paraplegia Laxatives ......................................................38 and tetraplegia .....................................44 Ispaghula (Psyllium husk) ........................45 ANTACIDS Indications: -

Transdermal Drug Delivery Device Including An
(19) TZZ_ZZ¥¥_T (11) EP 1 807 033 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.: of the grant of the patent: A61F 13/02 (2006.01) A61L 15/16 (2006.01) 20.07.2016 Bulletin 2016/29 (86) International application number: (21) Application number: 05815555.7 PCT/US2005/035806 (22) Date of filing: 07.10.2005 (87) International publication number: WO 2006/044206 (27.04.2006 Gazette 2006/17) (54) TRANSDERMAL DRUG DELIVERY DEVICE INCLUDING AN OCCLUSIVE BACKING VORRICHTUNG ZUR TRANSDERMALEN VERABREICHUNG VON ARZNEIMITTELN EINSCHLIESSLICH EINER VERSTOPFUNGSSICHERUNG DISPOSITIF D’ADMINISTRATION TRANSDERMIQUE DE MEDICAMENTS AVEC COUCHE SUPPORT OCCLUSIVE (84) Designated Contracting States: • MANTELLE, Juan AT BE BG CH CY CZ DE DK EE ES FI FR GB GR Miami, FL 33186 (US) HU IE IS IT LI LT LU LV MC NL PL PT RO SE SI • NGUYEN, Viet SK TR Miami, FL 33176 (US) (30) Priority: 08.10.2004 US 616861 P (74) Representative: Awapatent AB P.O. Box 5117 (43) Date of publication of application: 200 71 Malmö (SE) 18.07.2007 Bulletin 2007/29 (56) References cited: (73) Proprietor: NOVEN PHARMACEUTICALS, INC. WO-A-02/36103 WO-A-97/23205 Miami, FL 33186 (US) WO-A-2005/046600 WO-A-2006/028863 US-A- 4 994 278 US-A- 4 994 278 (72) Inventors: US-A- 5 246 705 US-A- 5 474 783 • KANIOS, David US-A- 5 474 783 US-A1- 2001 051 180 Miami, FL 33196 (US) US-A1- 2002 128 345 US-A1- 2006 034 905 Note: Within nine months of the publication of the mention of the grant of the European patent in the European Patent Bulletin, any person may give notice to the European Patent Office of opposition to that patent, in accordance with the Implementing Regulations. -

Neurochemical Mechanisms Underlying Alcohol Withdrawal
Neurochemical Mechanisms Underlying Alcohol Withdrawal John Littleton, MD, Ph.D. More than 50 years ago, C.K. Himmelsbach first suggested that physiological mechanisms responsible for maintaining a stable state of equilibrium (i.e., homeostasis) in the patient’s body and brain are responsible for drug tolerance and the drug withdrawal syndrome. In the latter case, he suggested that the absence of the drug leaves these same homeostatic mechanisms exposed, leading to the withdrawal syndrome. This theory provides the framework for a majority of neurochemical investigations of the adaptations that occur in alcohol dependence and how these adaptations may precipitate withdrawal. This article examines the Himmelsbach theory and its application to alcohol withdrawal; reviews the animal models being used to study withdrawal; and looks at the postulated neuroadaptations in three systems—the gamma-aminobutyric acid (GABA) neurotransmitter system, the glutamate neurotransmitter system, and the calcium channel system that regulates various processes inside neurons. The role of these neuroadaptations in withdrawal and the clinical implications of this research also are considered. KEY WORDS: AOD withdrawal syndrome; neurochemistry; biochemical mechanism; AOD tolerance; brain; homeostasis; biological AOD dependence; biological AOD use; disorder theory; biological adaptation; animal model; GABA receptors; glutamate receptors; calcium channel; proteins; detoxification; brain damage; disease severity; AODD (alcohol and other drug dependence) relapse; literature review uring the past 25 years research- science models used to study with- of the reasons why advances in basic ers have made rapid progress drawal neurochemistry as well as a research have not yet been translated Din understanding the chemi- reluctance on the part of clinicians to into therapeutic gains and suggests cal activities that occur in the nervous consider new treatments. -

Calcium Current Block by (-)-Pentobarbital, Phenobarbital
The Journal of Neuroscience, August 1993, 13(E): 321 l-3221 Calcium Current Block by (-)-Pentobarbital, Phenobarbital, and CHEB but not (+)-Pentobarbital in Acutely Isolated Hippocampal CA1 Neurons: Comparison with Effects on GABA-activated Cl- Current Jarlath M. H. ffrench-Mullen,’ Jeffery L. Barker,* and Michael A. Rogawski3 ‘Department of Pharmacology, Zeneca Pharmaceuticals Group, Zeneca Inc., Wilmington, Delaware 19897 and *Laboratory of Neurophysiology, and 3Neuronal Excitability Section, Epilepsy Research Branch, National Institute of Neurological Disorders and Stroke, National Institutes of Health, Bethesda, Maryland 20892 Block of a voltage-activated Ca*+ channel current by pheno- Ca*+ current, whereas the sedative effects that occur at high- barbital (PHB), 5-(2-cyclohexylideneethyl)-5-ethyl barbituric er concentrations could reflect stronger Ca2+ current block- acid (CHEB), and the optical R(-)- and S(+)-enantiomers of ade. The powerful sedative-hypnotic action of (-)-PB may pentobarbital (PB) was examined in freshly dissociated adult reflect greater maximal enhancement of GABA responses guinea pig hippocampal CA1 neurons; the effects of the in conjunction with strong inhibition of Ca2+ current. The barbiturates on GABA-activated Cl- current were also char- convulsant action of CHEB is unlikely to be related to its acterized in the same preparation. (-)-PB, PHB, and CHEB effects on the Ca*+ current. produced a reversible, concentration-dependent block of the [Key words: calcium channel, GABA receptor, (-)-pen- peak Ca*+ channel current (3 mM Ba2+ as the charge carrier) tobarbital, (+)-pentobarbital, phenobarbital, CHEB [S-(2-cy- evoked by depolarization from -80 to - 10 mV (I&,, values, clohexylideneethyl)-S-ethyl barbituric acid], CA 1 hippocam- 3.5, 72, and 118 PM, respectively).