Firmagon®) SMC No
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Leuprolide Acetate)
For Pediatric Use LUPRON® INJECTION (leuprolide acetate) Rx only DESCRIPTION Leuprolide acetate is a synthetic nonapeptide analog of naturally occurring gonadotropin releasing hormone (GnRH or LH-RH). The analog possesses greater potency than the natural hormone. The chemical name is 5- oxo -L-prolyl-L-histidyl-L-tryptophyl-L-seryl-L-tyrosyl-D-leucyl-L-leucyl-L-arginyl- N-ethyl-L-prolinamide acetate (salt) with the following structural formula: LUPRON INJECTION is a sterile, aqueous solution intended for daily subcutaneous injection. It is available in a 2.8 mL multiple dose vial containing leuprolide acetate (5 mg/mL), sodium chloride, USP (6.3 mg/mL) for tonicity adjustment, benzyl alcohol, NF as a preservative (9 mg/mL), and water for injection, USP. The pH may have been adjusted with sodium hydroxide, NF and/or acetic acid, NF. CLINICAL PHARMACOLOGY Leuprolide acetate, a GnRH agonist, acts as a potent inhibitor of gonadotropin secretion when given continuously and in therapeutic doses. Animal and human studies indicate that following an initial stimulation of gonadotropins, chronic administration of leuprolide acetate results in suppression of ovarian and testicular steroidogenesis. This effect is reversible upon discontinuation of drug therapy. Leuprolide acetate is not active when given orally. Pharmacokinetics A pharmacokinetic study of leuprolide acetate in children has not been performed. Absorption Page 1 In adults, bioavailability by subcutaneous administration is comparable to that by intravenous administration. Distribution The mean steady-state volume of distribution of leuprolide following intravenous bolus administration to healthy adult male volunteers was 27 L. In vitro binding to human plasma proteins ranged from 43% to 49%. -

Hormonal Treatment Strategies Tailored to Non-Binary Transgender Individuals
Journal of Clinical Medicine Review Hormonal Treatment Strategies Tailored to Non-Binary Transgender Individuals Carlotta Cocchetti 1, Jiska Ristori 1, Alessia Romani 1, Mario Maggi 2 and Alessandra Daphne Fisher 1,* 1 Andrology, Women’s Endocrinology and Gender Incongruence Unit, Florence University Hospital, 50139 Florence, Italy; [email protected] (C.C); jiska.ristori@unifi.it (J.R.); [email protected] (A.R.) 2 Department of Experimental, Clinical and Biomedical Sciences, Careggi University Hospital, 50139 Florence, Italy; [email protected]fi.it * Correspondence: fi[email protected] Received: 16 April 2020; Accepted: 18 May 2020; Published: 26 May 2020 Abstract: Introduction: To date no standardized hormonal treatment protocols for non-binary transgender individuals have been described in the literature and there is a lack of data regarding their efficacy and safety. Objectives: To suggest possible treatment strategies for non-binary transgender individuals with non-standardized requests and to emphasize the importance of a personalized clinical approach. Methods: A narrative review of pertinent literature on gender-affirming hormonal treatment in transgender persons was performed using PubMed. Results: New hormonal treatment regimens outside those reported in current guidelines should be considered for non-binary transgender individuals, in order to improve psychological well-being and quality of life. In the present review we suggested the use of hormonal and non-hormonal compounds, which—based on their mechanism of action—could be used in these cases depending on clients’ requests. Conclusion: Requests for an individualized hormonal treatment in non-binary transgender individuals represent a future challenge for professionals managing transgender health care. For each case, clinicians should balance the benefits and risks of a personalized non-standardized treatment, actively involving the person in decisions regarding hormonal treatment. -
Personalized ADT
Personalized ADT Thomas Keane MD Conflicts • Ferring • Tolemar • Bayer • Astellas • myriad Personalized ADT for the Specific Paent • Cardiac • OBesity and testosterone • Fsh • High volume metastac disease • Docetaxol • Significant LUTS Cardiovascular risk profile and ADT Is there a difference? Degarelix Belongs to a class of synthe@c drug, GnRH antagonist (Blocker) GnRH pGlu His Trp Ser Tyr Gly Leu Arg Pro Gly NH2 Leuprolide D-Leu NEt Goserelin D-Ser NH2 LHRH agonists Triptorelin D-Trp NH2 Buserelin D-Ser NEt Degarelix D-NaI D-Cpa D-PaI Aph D-Aph D-Ala NH2 N-Me ABarelix D-NaI D-Cpa D-PaI D-Asn Lys D-Ala NH2 Tyr GnRH antagonists Cetrorelix D-NaI D-Cpa D-PaI D-Cit D-Ala NH2 Ganirelix D-NaI D-CPa D-PaI D-hArg D-hArg D-Ala NH2 Millar RP, et al. Endocr Rev 2004;25:235–75 Most acute CVD events are caused By rupture of a vulnerable atherosclero@c plaque The vulnerable plaque – thin cap with inflammaon Inflammation Plaque instability is at the heart of cardiovascular disease Stable plaque Vulnerable plaque Lumen Lumen Lipid core Lipid core FiBrous cap FiBrous cap Thick Cap Thin Rich in SMC and matrix Composion Rich in inflammatory cells: proteoly@c ac@vity Poor Lipid Rich Inflammatory Inflammatory state Highly inflammatory LiBBy P. Circulaon 1995;91:2844-2850 Incidence of Both prostate cancer and CV events is highest in older men Prostate cancer CV events 3500 3500 Prostate cancer All CV disease Major CV events 3000 3000 2827.1 2500 2500 2338.9 2000 2000 1719.7 1500 1500 1152.6 1008.7 1038.7 1000 1000 641.2 545.2 571.1 Age-specific incidence per 100,000 person-years 500 500 246.9 133.7 4.3 0 0 40-49 50-59 60-69 70-79 80-89 90-99 40-49 50-59 60-69 70-79 80-89 90-99 CV, cardiovascular Major CV events = myocardial infarc@on, stroke, or death due to CV disease All CV disease = major CV events + self-reported angina or revascularisaon procedures Driver, et al. -

Hertfordshire Medicines Management Committee (Hmmc) Nafarelin for Endometriosis Amber Initiation – Recommended for Restricted Use
HERTFORDSHIRE MEDICINES MANAGEMENT COMMITTEE (HMMC) NAFARELIN FOR ENDOMETRIOSIS AMBER INITIATION – RECOMMENDED FOR RESTRICTED USE Name: What it is Indication Date Decision NICE / SMC generic decision status Guidance (trade) last revised Nafarelin A potent agonistic The hormonal December Final NICE NG73 2mg/ml analogue of management of 2020 Nasal Spray gonadotrophin endometriosis, (Synarel®) releasing hormone including pain relief and (GnRH) reduction of endometriotic lesions HMMC recommendation: Amber initiation across Hertfordshire (i.e. suitable for primary care prescribing after specialist initiation) as an option in endometriosis Background Information: Gonadorelin analogues (or gonadotrophin-releasing hormone agonists [GnRHas]) include buserelin, goserelin, leuprorelin, nafarelin and triptorelin. The current HMMC decision recommends triptorelin as Decapeptyl SR® injection as the gonadorelin analogue of choice within licensed indications (which include endometriosis) link to decision. A request was made by ENHT to use nafarelin nasal spray as an alternative to triptorelin intramuscular injection during the COVID-19 pandemic. The hospital would provide initial 1 month supply, then GPs would continue for further 5 months as an alternative to the patient attending for further clinic appointments for administration of triptorelin. Previously at ENHT, triptorelin was the only gonadorelin analogue on formulary for gynaecological indications. At WHHT buserelin nasal spray 150mcg/dose is RED (hospital only) for infertility & endometriosis indications. Nafarelin nasal spray 2mg/ml is licensed for: . The hormonal management of endometriosis, including pain relief and reduction of endometriotic lesions. Use in controlled ovarian stimulation programmes prior to in-vitro fertilisation, under the supervision of an infertility specialist. Use of nafarelin in endometriosis aims to induce chronic pituitary desensitisation, which gives a menopause-like state maintained over many months. -

Statistical Analysis Plan
Title: An Open label, Multicenter Study to Assess the Safety and Efficacy of Leuprorelin in the Treatment of Central Precocious Puberty NCT Number: NCT02427958 SAP Approve Date: 01 June 2017 Certain information within this Statistical Analysis Plan has been redacted (ie, specific content is masked irreversibly from view with a black/blue bar) to protect either personally identifiable (PPD) information or company confidential information (CCI). This may include, but is not limited to, redaction of the following: Named persons or organizations associated with the study. Proprietary information, such as scales or coding systems, which are considered confidential information under prior agreements with license holder. • Other information as needed to protect confidentiality of Takeda or partners, personal information, or to otherwise protect the integrity of the clinical study. Takeda Statistical Analysis Plan Leuprorelin-4001 Version: 1.0 An Open label, Multicenter Study to Assess the Safety and Efficacy of Leuprorelin in the Treatment of Central Precocious Puberty Leuprorelin-4001, Leuprorelin in the Treatment of Central Precocious Puberty Statistical Analysis Plan Version: 1.0 Date: 01 June 2017 1 PPD PPD Takeda Statistical Analysis Plan Leuprorelin-4001 Version: 1.0 TABLE OF CONTENTS ABBREVIATIONS ........................................................................................................................ 6 1. INTRODUCTION ............................................................................................................... -

Degarelix for Treating Advanced Hormone- Dependent Prostate Cancer
CONFIDENTIAL UNTIL PUBLISHED NATIONAL INSTITUTE FOR HEALTH AND CARE EXCELLENCE Final appraisal determination Degarelix for treating advanced hormone- dependent prostate cancer This guidance was developed using the single technology appraisal (STA) process 1 Guidance 1.1 Degarelix is recommended as an option for treating advanced hormone-dependent prostate cancer, only in adults with spinal metastases who present with signs or symptoms of spinal cord compression. 1.2 People currently receiving treatment initiated within the NHS with degarelix that is not recommended for them by NICE in this guidance should be able to continue treatment until they and their NHS clinician consider it appropriate to stop. 2 The technology 2.1 Degarelix (Firmagon, Ferring Pharmaceuticals) is a selective gonadotrophin-releasing hormone antagonist that reduces the release of gonadotrophins by the pituitary, which in turn reduces the secretion of testosterone by the testes. Gonadotrophin- releasing hormone is also known as luteinising hormone-releasing hormone (LHRH). Because gonadotrophin-releasing hormone antagonists do not produce a rise in hormone levels at the start of treatment, there is no initial testosterone surge or tumour stimulation, and therefore no potential for symptomatic flares. National Institute for Health and Care Excellence Page 1 of 71 Final appraisal determination – Degarelix for treating advanced hormone-dependent prostate cancer Issue date: April 2014 CONFIDENTIAL UNTIL PUBLISHED Degarelix has a UK marketing authorisation for the ‘treatment of adult male patients with advanced hormone-dependent prostate cancer’. It is administered as a subcutaneous injection. 2.2 The most common adverse reactions with degarelix are related to the effects of testosterone suppression, including hot flushes and weight increase, or injection site reactions (such as pain and erythema). -

Altered Cognitive Function in Men Treated for Prostate
Altered Cognitive Function in Men Treated for Prostate Cancer with LHRH Analogues and Cyproterone Acetate: A Randomised Controlled Trial H. J. Green PhD1,2, K. I. Pakenham PhD1, B. C. Headley PhD3, J. Yaxley FRACS3, D. L. Nicol FRACS2,4, P. N. Mactaggart FRACS2,5, C. Swanson PhD2, R. B. W atson FRACS6, & R. A. Gardiner MD2,3 1School of Psychology and 2Department of Surgery, The University of Queensland, 3Royal Brisbane, 4Princess Alexandra, 5Queen Elizabeth II & 6Mater Hospitals, Brisbane, Queensland, Australia In conjunction with the Northern Section of the Urological Society of Australasia Correspondence should be addressed to: Dr R. A. Gardiner, Department of Surgery, The University of Queensland, Brisbane, Qld 4072, Australia Fax: +61 7 3365 5559; Phone: +61 7 3365 5233; Email: f.gardiner@ mailbox.uq.edu.au This work was wholly funded by Queensland Cancer Fund. **PREPRINT. Final version published in British Journal of Urology (BJU: International) (2002), 90, 427-432 ** Short Title: COGNITIVE CHANGES W ITH HORMONAL MEDICATION 2 Objective. Luteinising hormone releasing hormone (LHRH) analogues have been associated with memory impairments in women using these drugs for gynaecological conditions. This is the first systematic investigation of the cognitive effects of LHRH analogues in male patients. Methods. 82 men with non-localised prostate cancer were randomly assigned to receive continuous leuprorelin (LHRH analogue), goserelin (LHRH analogue), cyproterone acetate (steroidal antiandrogen) or close clinical monitoring. These patients underwent cognitive assessments at baseline and before commencement of treatment (77) then 6 months later (65). Results. Compared with baseline assessments, men administered androgen suppression monotherapy performed worse in 2/12 tests of attention and memory. -

Degarelix Acetate (Firmagon) Reference Number: PA.CP.PHAR.170 Effective Date: 01/18 Last Review Date: 10/18 Revision Log
Clinical Policy: Degarelix Acetate (Firmagon) Reference Number: PA.CP.PHAR.170 Effective Date: 01/18 Last Review Date: 10/18 Revision Log Description The intent of the criteria is to ensure that patients follow selection elements established by Pennsylvania Health and Wellness® clinical policy for the use of Degarelix Acetate (Firmagon®). FDA Approved Indication(s) Firmagon is indicated for treatment of advanced prostate cancer. Policy/Criteria It is the policy of Pennsylvania Health and Wellness that Firmagon is medically necessary when the following criteria are met: I. Initial Approval Criteria A. Prostate Cancer (must meet all): 1. Diagnosis of prostate cancer; 2. Prescribed by or in consultation with an oncologist; 3. Request meets one of the following (a, b or c): a. Starting dose does not exceed 240 mg given as two injections of 120 mg each; b. Maintenance dose does not exceed 80 mg as a single injection per 28 days; c. Dose is supported by practice guidelines or peer-reviewed literature for the relevant off- label use (prescriber must submit supporting evidence). Approval duration: 12 months B. Other diagnoses/indications: Refer to PA.CP.PMN.53 1. The following NCCN recommended uses for Firmagon, meeting NCCN categories 1, 2a, or 2b, are approved per the PA.CP.PMN.53: II. Continued Approval A. Prostate Cancer (must meet all): 1. Currently receiving medication via Pennsylvania Health and Wellness benefit or member has previously met approval criteria or the Continuity of Care policy (PA.LTSS.PHAR.01) applies; 2. Member is responding positively to therapy; 3. If request is for a dose increase, request meets one of the following: a. -
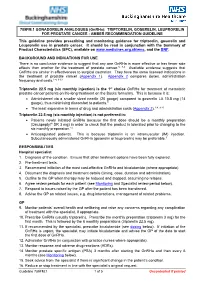
Triptorelin, Goserelin and Leuprorelin for Prostate
789FM.1 GONADORELIN ANALOGUES (GnRHa): TRIPTORELIN, GOSERELIN, LEUPRORELIN FOR PROSTATE CANCER - AMBER RECOMMENDATION GUIDELINE This guideline provides prescribing and monitoring guidance for triptorelin, goserelin and Leuprorelin use in prostate cancer. It should be read in conjunction with the Summary of Product Characteristics (SPC), available on www.medicines.org.uk/emc, and the BNF. BACKGROUND AND INDICATIONS FOR USE There is no conclusive evidence to suggest that any one GnRHa is more effective or has fewer side effects than another for the treatment of prostate cancer.5, 7-9 Available evidence suggests that GnRHa are similar in effectiveness to surgical castration. They have the same licensed indications in the treatment of prostate cancer (Appendix 1). Appendix 2 compares doses, administration frequency and costs.1-4, 9-13 Triptorelin 22.5 mg (six monthly injection) is the 1st choice GnRHa for treatment of metastatic prostate cancer patients on life-long treatment on the Bucks formulary. This is because it is: • Administered via a smaller sized needle (20 gauge) compared to goserelin LA 10.8 mg (14 gauge), thus minimising discomfort to patients.9 • The least expensive in terms of drug and administration costs (Appendix 2).1-4, 9-13 Triptorelin 22.5 mg (six monthly injection) is not preferred in: • Patients newly initiated GnRHa because the first dose should be a monthly preparation (Decapeptyl® SR 3 mg) in order to check that the product is tolerated prior to changing to the six monthly preparation.14 • Anticoagulated patients. This is because triptorelin is an intramuscular (IM) injection. Subcutaneously administered GnRHa (goserelin or leuprorelin) may be preferable.9 RESPONSIBILITIES Hospital specialist 1. -

Follicular and Endocrine Profiles Associated with Different Gnrh
Reproductive BioMedicine Online (2012) 24, 153– 162 www.sciencedirect.com www.rbmonline.com ARTICLE Follicular and endocrine profiles associated with different GnRH-antagonist regimens: a randomized controlled trial Juan Antonio Garcı´a-Velasco a, Sanja Kupesic b, Antonio Pellicer c, Claire Bourgain d, Carlos Simo´n e, Milan Mrazek f, Paul Devroey g, Joan-Carles Arce h,* a IVI Foundation, Reproductive Endocrinology, Madrid, Spain; b Texas Tech University Health Sciences Center, Department of Obstetrics and Gynecology, El Paso, TX, USA; c IVI Foundation, Reproductive Endocrinology, Valencia, Spain; d UZ Brussel, Department of Pathology, Brussels, Belgium; e IVI Foundation, Research Department, Valencia, Spain; f ISCARE IVF a.s., Lighthouse, Prague, Czech Republic; g UZ Brussel, Centre for Reproductive Medicine, Brussels, Belgium; h Reproductive Health, Global Clinical and Non-Clinical R & D, Ferring Pharmaceuticals, Copenhagen, Denmark * Corresponding author. E-mail address: [email protected] (J.-C. Arce). Dr Juan Garcı´a-Velasco did his training in obstetrics and gynaecology at Madrid Autonoma University, and then his reproductive endocrinology and infertility fellowship at Yale University, USA (1997–1998). He is now Director of IVI-Madrid and Associate Professor at Rey Juan Carlos University. He has published over 100 peer- reviewed articles. He is an ad-hoc reviewer for the main journals in the field and serves on the editorial board of Reproductive BioMedicine Online. His main research interests are endometriosis, ovarian hyperstimulation syndrome, low responders and human implantation. Abstract This trial assessed the impact of early initiation of gonadotrophin-releasing hormone (GnRH) antagonist on follicular and endocrine profiles compared with the fixed GnRH-antagonist protocol. -

Gnrh Antagonists Have Direct Inhibitory Effects on Castration-Resistant Prostate
Author Manuscript Published OnlineFirst on July 24, 2019; DOI: 10.1158/1535-7163.MCT-18-1337 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. GnRH antagonists have direct inhibitory effects on castration-resistant prostate cancer via intracrine androgen and AR-V7 expression. Vito Cucchiara1*, Joy C. Yang1*, Chengfei Liu1, Hans H. Adomat2, Emma S. Tomlinson Guns2, Martin E. Gleave2, Allen C. Gao1,3, Christopher P. Evans1,3 1Department of Urologic Surgery, University of California at Davis, Sacramento, California. 2Vancouver Prostate Centre, University of British Columbia, Vancouver, BC, Canada 3UC Davis Comprehensive Cancer Center, University of California Davis, California. Running title: GnRH antagonist inhibits intracrine androgen and AR-V7 Keywords: Prostate Cancer, ADT, GnRH antagonist, intracrine androgen Financial Support: This work is supported in part by grants DOD PC150040P1 and Ferring Pharmaceuticals to CP Evans. Conflicts of Interest: Research support from Ferring to CPE and JCY. All other authors have no conflicts of interest. Corresponding Author: Christopher P. Evans, MD, FACS Professor and Chairman, Department of Urology Urologic Surgical Oncology University of California, Davis, School of Medicine 4860 Y St., Suite 3500 Sacramento, CA 95817 academic office tel # (916)734-7520 academic office fax # (916)734-8094 email: [email protected] *These authors contributed equally to this work Downloaded from mct.aacrjournals.org on October 6, 2021. © 2019 American Association for Cancer Research. Author Manuscript Published OnlineFirst on July 24, 2019; DOI: 10.1158/1535-7163.MCT-18-1337 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. -

Systematic Review of Luteinising Hormone-Releasing Hormone Agonists in Adjuvant Therapy of Early Breast Cancer
Systematic review of luteinising hormone-releasing hormone agonists in adjuvant therapy of early breast cancer Search conducted May–June 2003 Review written June–November 2003 Prepared by Sharma R, Hamilton A, Beith J On behalf of the National Breast Cancer Centre This Systematic review of luteinising hormone-releasing hormone agonists in adjuvant therapy of early breast cancer was prepared by Sharma R, Hamilton A and Beith J on behalf of the National Breast Cancer Centre: 92 Parramatta Road Camperdown, Sydney, Australia Locked Bag 16 Camperdown NSW 1450 Telephone +61 2 9036 3030 Facsimile +61 2 9036 3077 Website www.nbcc.org.au © National Breast Cancer Centre 2004 ISBN Print: 1 74127 019 7 Online: 1 74127 025 1 This work is copyright. Apart from any use as permitted under the Copyright Act 1968, no part may be reproduced by any process without prior written permission from the National Breast Cancer Centre. Requests and enquiries concerning reproduction and rights should be addressed to the Copyright Office, National Breast Cancer Centre, Locked Bag 16 Camperdown NSW 1450 Australia. Website: www.nbcc.org.au Email: [email protected] The conclusions of this systematic review are based on evidence available to November 2003. New data are constantly emerging. The conclusions of this systematic review are likely to change with longer follow-up periods and in light of evidence from other trials. The National Breast Cancer Centre is funded by the Australian Government Department of Health & Ageing 2 Systematic review of luteinising hormone-releasing