Triptorelin, Goserelin and Leuprorelin for Prostate
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Study Protocol and Documented in the Subject Dispensing Log
Protocol Title of trial: A Multicenter, Double-Blind, Randomized, Placebo-Controlled Study Evaluating Three Doses of Subcutaneous Pulsatile GnRH Administered via OmniPod Pump for Ovulation Induction in Female Subjects with Primary Amenorrhea with Hypogonadotropic Hypogonadism NCT number: NCT01976728 Sponsor trial code: 000070 Date: 06 Dec 2017 Gonadorelin Acetate, FE Trial Code: 000070 Date: 06 Dec 2017 999037, FE 999903 E-Protocol Amendment-21975;1.0 No Specified Dosage Form and Strength Supersedes: None Clinical Trial Protocol - Amendment 7 Page 1 of 82 CLINICAL TRIAL PROTOCOL A Multicenter, Double-Blind, Randomized, Placebo-Controlled Study Evaluating Three Doses of Subcutaneous Pulsatile GnRH Administered via OmniPod Pump for Ovulation Induction in Female Subjects with Primary Amenorrhea with Hypogonadotropic Hypogonadism Trial Code 000070 Consolidated Protocol Incorporating Amendments 1-7 IND Number: 22,278 Investigational Medicinal Product: LutrePulse OmniPod Indication: Primary Hypothalamic Amenorrhea Phase: III Name and Address of Sponsor: Ferring International Pharmascience Center U.S., Inc. 100 Interpace Parkway Parsippany, NJ 07054 P: 973-796-1600 F: 973-796-1660 GCP Statement: This trial will be performed in compliance with GCP. The information in this document is confidential and is proprietary to Ferring International Pharmascience Center U.S. or another company within the Ferring Group. It is understood that information in this document shall not be disclosed to any third party, in any form, without prior written consent -

Leuprolide Acetate)
For Pediatric Use LUPRON® INJECTION (leuprolide acetate) Rx only DESCRIPTION Leuprolide acetate is a synthetic nonapeptide analog of naturally occurring gonadotropin releasing hormone (GnRH or LH-RH). The analog possesses greater potency than the natural hormone. The chemical name is 5- oxo -L-prolyl-L-histidyl-L-tryptophyl-L-seryl-L-tyrosyl-D-leucyl-L-leucyl-L-arginyl- N-ethyl-L-prolinamide acetate (salt) with the following structural formula: LUPRON INJECTION is a sterile, aqueous solution intended for daily subcutaneous injection. It is available in a 2.8 mL multiple dose vial containing leuprolide acetate (5 mg/mL), sodium chloride, USP (6.3 mg/mL) for tonicity adjustment, benzyl alcohol, NF as a preservative (9 mg/mL), and water for injection, USP. The pH may have been adjusted with sodium hydroxide, NF and/or acetic acid, NF. CLINICAL PHARMACOLOGY Leuprolide acetate, a GnRH agonist, acts as a potent inhibitor of gonadotropin secretion when given continuously and in therapeutic doses. Animal and human studies indicate that following an initial stimulation of gonadotropins, chronic administration of leuprolide acetate results in suppression of ovarian and testicular steroidogenesis. This effect is reversible upon discontinuation of drug therapy. Leuprolide acetate is not active when given orally. Pharmacokinetics A pharmacokinetic study of leuprolide acetate in children has not been performed. Absorption Page 1 In adults, bioavailability by subcutaneous administration is comparable to that by intravenous administration. Distribution The mean steady-state volume of distribution of leuprolide following intravenous bolus administration to healthy adult male volunteers was 27 L. In vitro binding to human plasma proteins ranged from 43% to 49%. -

CASODEX (Bicalutamide)
HIGHLIGHTS OF PRESCRIBING INFORMATION • Gynecomastia and breast pain have been reported during treatment with These highlights do not include all the information needed to use CASODEX 150 mg when used as a single agent. (5.3) CASODEX® safely and effectively. See full prescribing information for • CASODEX is used in combination with an LHRH agonist. LHRH CASODEX. agonists have been shown to cause a reduction in glucose tolerance in CASODEX® (bicalutamide) tablet, for oral use males. Consideration should be given to monitoring blood glucose in Initial U.S. Approval: 1995 patients receiving CASODEX in combination with LHRH agonists. (5.4) -------------------------- RECENT MAJOR CHANGES -------------------------- • Monitoring Prostate Specific Antigen (PSA) is recommended. Evaluate Warnings and Precautions (5.2) 10/2017 for clinical progression if PSA increases. (5.5) --------------------------- INDICATIONS AND USAGE -------------------------- ------------------------------ ADVERSE REACTIONS ----------------------------- • CASODEX 50 mg is an androgen receptor inhibitor indicated for use in Adverse reactions that occurred in more than 10% of patients receiving combination therapy with a luteinizing hormone-releasing hormone CASODEX plus an LHRH-A were: hot flashes, pain (including general, back, (LHRH) analog for the treatment of Stage D2 metastatic carcinoma of pelvic and abdominal), asthenia, constipation, infection, nausea, peripheral the prostate. (1) edema, dyspnea, diarrhea, hematuria, nocturia, and anemia. (6.1) • CASODEX 150 mg daily is not approved for use alone or with other treatments. (1) To report SUSPECTED ADVERSE REACTIONS, contact AstraZeneca Pharmaceuticals LP at 1-800-236-9933 or FDA at 1-800-FDA-1088 or ---------------------- DOSAGE AND ADMINISTRATION ---------------------- www.fda.gov/medwatch The recommended dose for CASODEX therapy in combination with an LHRH analog is one 50 mg tablet once daily (morning or evening). -

Hormonal Treatment Strategies Tailored to Non-Binary Transgender Individuals
Journal of Clinical Medicine Review Hormonal Treatment Strategies Tailored to Non-Binary Transgender Individuals Carlotta Cocchetti 1, Jiska Ristori 1, Alessia Romani 1, Mario Maggi 2 and Alessandra Daphne Fisher 1,* 1 Andrology, Women’s Endocrinology and Gender Incongruence Unit, Florence University Hospital, 50139 Florence, Italy; [email protected] (C.C); jiska.ristori@unifi.it (J.R.); [email protected] (A.R.) 2 Department of Experimental, Clinical and Biomedical Sciences, Careggi University Hospital, 50139 Florence, Italy; [email protected]fi.it * Correspondence: fi[email protected] Received: 16 April 2020; Accepted: 18 May 2020; Published: 26 May 2020 Abstract: Introduction: To date no standardized hormonal treatment protocols for non-binary transgender individuals have been described in the literature and there is a lack of data regarding their efficacy and safety. Objectives: To suggest possible treatment strategies for non-binary transgender individuals with non-standardized requests and to emphasize the importance of a personalized clinical approach. Methods: A narrative review of pertinent literature on gender-affirming hormonal treatment in transgender persons was performed using PubMed. Results: New hormonal treatment regimens outside those reported in current guidelines should be considered for non-binary transgender individuals, in order to improve psychological well-being and quality of life. In the present review we suggested the use of hormonal and non-hormonal compounds, which—based on their mechanism of action—could be used in these cases depending on clients’ requests. Conclusion: Requests for an individualized hormonal treatment in non-binary transgender individuals represent a future challenge for professionals managing transgender health care. For each case, clinicians should balance the benefits and risks of a personalized non-standardized treatment, actively involving the person in decisions regarding hormonal treatment. -
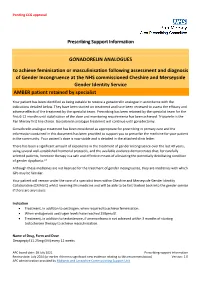
Prescribing Support Information GONADORELIN ANALOGUES To
Pending CCG approval Prescribing Support Information GONADORELIN ANALOGUES to achieve feminisation or masculinisation following assessment and diagnosis of Gender Incongruence at the NHS commissioned Cheshire and Merseyside Gender Identity Service AMBER patient retained by specialist Your patient has been identified as being suitable to receive a gonadorelin analogue in accordance with the indications detailed below. They have been started on treatment and have been reviewed to assess the efficacy and adverse effects of the treatment by the specialist team. Prescribing has been retained by the specialist team for the first 6-12 months until stabilisation of the dose and monitoring requirements has been achieved. Triptorelin is the Pan Mersey first line choice. Gonadorelin analogue treatment will continue until gonadectomy. Gonadorelin analogue treatment has been considered as appropriate for prescribing in primary care and the information contained in this document has been provided to support you to prescribe the medicine for your patient in the community. Your patient’s dose is now stable and is detailed in the attached clinic letter. There has been a significant amount of experience in the treatment of gender incongruence over the last 40 years, using several well-established hormonal protocols, and the available evidence demonstrates that, for carefully selected patients, hormone therapy is a safe and effective means of alleviating the potentially debilitating condition of gender dysphoria.1.2 Although these medicines are not licensed for the treatment of gender incongruence, they are medicines with which GPs may be familiar. Your patient will remain under the care of a specialist team within Cheshire and Merseyside Gender Identity Collaborative (CMAGIC) whilst receiving this medicine and will be able to be fast tracked back into the gender service if there are any issues. -

Hertfordshire Medicines Management Committee (Hmmc) Nafarelin for Endometriosis Amber Initiation – Recommended for Restricted Use
HERTFORDSHIRE MEDICINES MANAGEMENT COMMITTEE (HMMC) NAFARELIN FOR ENDOMETRIOSIS AMBER INITIATION – RECOMMENDED FOR RESTRICTED USE Name: What it is Indication Date Decision NICE / SMC generic decision status Guidance (trade) last revised Nafarelin A potent agonistic The hormonal December Final NICE NG73 2mg/ml analogue of management of 2020 Nasal Spray gonadotrophin endometriosis, (Synarel®) releasing hormone including pain relief and (GnRH) reduction of endometriotic lesions HMMC recommendation: Amber initiation across Hertfordshire (i.e. suitable for primary care prescribing after specialist initiation) as an option in endometriosis Background Information: Gonadorelin analogues (or gonadotrophin-releasing hormone agonists [GnRHas]) include buserelin, goserelin, leuprorelin, nafarelin and triptorelin. The current HMMC decision recommends triptorelin as Decapeptyl SR® injection as the gonadorelin analogue of choice within licensed indications (which include endometriosis) link to decision. A request was made by ENHT to use nafarelin nasal spray as an alternative to triptorelin intramuscular injection during the COVID-19 pandemic. The hospital would provide initial 1 month supply, then GPs would continue for further 5 months as an alternative to the patient attending for further clinic appointments for administration of triptorelin. Previously at ENHT, triptorelin was the only gonadorelin analogue on formulary for gynaecological indications. At WHHT buserelin nasal spray 150mcg/dose is RED (hospital only) for infertility & endometriosis indications. Nafarelin nasal spray 2mg/ml is licensed for: . The hormonal management of endometriosis, including pain relief and reduction of endometriotic lesions. Use in controlled ovarian stimulation programmes prior to in-vitro fertilisation, under the supervision of an infertility specialist. Use of nafarelin in endometriosis aims to induce chronic pituitary desensitisation, which gives a menopause-like state maintained over many months. -
Statistical Analysis Plan
Title: An Open label, Multicenter Study to Assess the Safety and Efficacy of Leuprorelin in the Treatment of Central Precocious Puberty NCT Number: NCT02427958 SAP Approve Date: 01 June 2017 Certain information within this Statistical Analysis Plan has been redacted (ie, specific content is masked irreversibly from view with a black/blue bar) to protect either personally identifiable (PPD) information or company confidential information (CCI). This may include, but is not limited to, redaction of the following: Named persons or organizations associated with the study. Proprietary information, such as scales or coding systems, which are considered confidential information under prior agreements with license holder. • Other information as needed to protect confidentiality of Takeda or partners, personal information, or to otherwise protect the integrity of the clinical study. Takeda Statistical Analysis Plan Leuprorelin-4001 Version: 1.0 An Open label, Multicenter Study to Assess the Safety and Efficacy of Leuprorelin in the Treatment of Central Precocious Puberty Leuprorelin-4001, Leuprorelin in the Treatment of Central Precocious Puberty Statistical Analysis Plan Version: 1.0 Date: 01 June 2017 1 PPD PPD Takeda Statistical Analysis Plan Leuprorelin-4001 Version: 1.0 TABLE OF CONTENTS ABBREVIATIONS ........................................................................................................................ 6 1. INTRODUCTION ............................................................................................................... -

Degarelix for Treating Advanced Hormone- Dependent Prostate Cancer
CONFIDENTIAL UNTIL PUBLISHED NATIONAL INSTITUTE FOR HEALTH AND CARE EXCELLENCE Final appraisal determination Degarelix for treating advanced hormone- dependent prostate cancer This guidance was developed using the single technology appraisal (STA) process 1 Guidance 1.1 Degarelix is recommended as an option for treating advanced hormone-dependent prostate cancer, only in adults with spinal metastases who present with signs or symptoms of spinal cord compression. 1.2 People currently receiving treatment initiated within the NHS with degarelix that is not recommended for them by NICE in this guidance should be able to continue treatment until they and their NHS clinician consider it appropriate to stop. 2 The technology 2.1 Degarelix (Firmagon, Ferring Pharmaceuticals) is a selective gonadotrophin-releasing hormone antagonist that reduces the release of gonadotrophins by the pituitary, which in turn reduces the secretion of testosterone by the testes. Gonadotrophin- releasing hormone is also known as luteinising hormone-releasing hormone (LHRH). Because gonadotrophin-releasing hormone antagonists do not produce a rise in hormone levels at the start of treatment, there is no initial testosterone surge or tumour stimulation, and therefore no potential for symptomatic flares. National Institute for Health and Care Excellence Page 1 of 71 Final appraisal determination – Degarelix for treating advanced hormone-dependent prostate cancer Issue date: April 2014 CONFIDENTIAL UNTIL PUBLISHED Degarelix has a UK marketing authorisation for the ‘treatment of adult male patients with advanced hormone-dependent prostate cancer’. It is administered as a subcutaneous injection. 2.2 The most common adverse reactions with degarelix are related to the effects of testosterone suppression, including hot flushes and weight increase, or injection site reactions (such as pain and erythema). -

Tanibirumab (CUI C3490677) Add to Cart
5/17/2018 NCI Metathesaurus Contains Exact Match Begins With Name Code Property Relationship Source ALL Advanced Search NCIm Version: 201706 Version 2.8 (using LexEVS 6.5) Home | NCIt Hierarchy | Sources | Help Suggest changes to this concept Tanibirumab (CUI C3490677) Add to Cart Table of Contents Terms & Properties Synonym Details Relationships By Source Terms & Properties Concept Unique Identifier (CUI): C3490677 NCI Thesaurus Code: C102877 (see NCI Thesaurus info) Semantic Type: Immunologic Factor Semantic Type: Amino Acid, Peptide, or Protein Semantic Type: Pharmacologic Substance NCIt Definition: A fully human monoclonal antibody targeting the vascular endothelial growth factor receptor 2 (VEGFR2), with potential antiangiogenic activity. Upon administration, tanibirumab specifically binds to VEGFR2, thereby preventing the binding of its ligand VEGF. This may result in the inhibition of tumor angiogenesis and a decrease in tumor nutrient supply. VEGFR2 is a pro-angiogenic growth factor receptor tyrosine kinase expressed by endothelial cells, while VEGF is overexpressed in many tumors and is correlated to tumor progression. PDQ Definition: A fully human monoclonal antibody targeting the vascular endothelial growth factor receptor 2 (VEGFR2), with potential antiangiogenic activity. Upon administration, tanibirumab specifically binds to VEGFR2, thereby preventing the binding of its ligand VEGF. This may result in the inhibition of tumor angiogenesis and a decrease in tumor nutrient supply. VEGFR2 is a pro-angiogenic growth factor receptor -

Sgnrha-Ovarh-Study-Protocol.Pdf
STUDY PROTOCOL FOR A COMPASSIONATE AQUACULTURE INVESTIGATIONAL NEW ANIMAL DRUG (INAD) EXEMPTION FOR SALMON GONADOTROPIN-RELEASING HORMONE ® ANALOGUE (sGnRHa - OvaRH ) (INAD 012-186) Sponsor: U.S. Fish and Wildlife Service, Division of Fish Hatcheries ______________________ ___________________ Sponsor Signature Date Approved Manufacturer: Western Chemical Inc. 1269 Lattimore Road Ferndale, WA Facility for Coordination of sGnRHa (OvaRH®) INAD: Aquatic Animal Drug Approval Partnership Program 4050 Bridger Canyon Road Bozeman, Mt 59715 Proposed Starting Date September 1, 2012 Proposed Ending Date August 31, 2017 Study Director Mr. Jim Bowker _________________________ ________________ Study Director Signature Date Clinical Field Trial Location and Trial Number: __________________________________________ _________________ Type or Print Facility Name Trial Number Investigator______________________________________________________ Type or Print Name __________________________________________ _________________ Investigator Signature Date I. STUDY ID AND TITLE .................................................................................................................................. 1 II. SPONSOR..................................................................................................................................................... 1 III. INVESTIGATORS/FACILITIES .................................................................................................................... 2 IV. PROPOSED STARTING AND COMPLETION DATES: ........................................................................ -

Altered Cognitive Function in Men Treated for Prostate
Altered Cognitive Function in Men Treated for Prostate Cancer with LHRH Analogues and Cyproterone Acetate: A Randomised Controlled Trial H. J. Green PhD1,2, K. I. Pakenham PhD1, B. C. Headley PhD3, J. Yaxley FRACS3, D. L. Nicol FRACS2,4, P. N. Mactaggart FRACS2,5, C. Swanson PhD2, R. B. W atson FRACS6, & R. A. Gardiner MD2,3 1School of Psychology and 2Department of Surgery, The University of Queensland, 3Royal Brisbane, 4Princess Alexandra, 5Queen Elizabeth II & 6Mater Hospitals, Brisbane, Queensland, Australia In conjunction with the Northern Section of the Urological Society of Australasia Correspondence should be addressed to: Dr R. A. Gardiner, Department of Surgery, The University of Queensland, Brisbane, Qld 4072, Australia Fax: +61 7 3365 5559; Phone: +61 7 3365 5233; Email: f.gardiner@ mailbox.uq.edu.au This work was wholly funded by Queensland Cancer Fund. **PREPRINT. Final version published in British Journal of Urology (BJU: International) (2002), 90, 427-432 ** Short Title: COGNITIVE CHANGES W ITH HORMONAL MEDICATION 2 Objective. Luteinising hormone releasing hormone (LHRH) analogues have been associated with memory impairments in women using these drugs for gynaecological conditions. This is the first systematic investigation of the cognitive effects of LHRH analogues in male patients. Methods. 82 men with non-localised prostate cancer were randomly assigned to receive continuous leuprorelin (LHRH analogue), goserelin (LHRH analogue), cyproterone acetate (steroidal antiandrogen) or close clinical monitoring. These patients underwent cognitive assessments at baseline and before commencement of treatment (77) then 6 months later (65). Results. Compared with baseline assessments, men administered androgen suppression monotherapy performed worse in 2/12 tests of attention and memory. -

The Use of an Intravaginal Triptorelin Gel to Induce Ovulation in the Mare
THE USE OF AN INTRAVAGINAL TRIPTORELIN GEL TO INDUCE OVULATION IN THE MARE by CHELSEA D. SINCLAIR B.S., Clemson University, 2013 A THESIS submitted in partial fulfillment of the requirements for the degree MASTER OF SCIENCE Department of Animal Sciences and Industry College of Agriculture KANSAS STATE UNIVERSITY Manhattan, Kansas 2016 Approved by: Major Professor Dr. Joann M. Kouba Copyright CHELSEA D. SINCLAIR 2016 Abstract The objective of these studies was to investigate the efficacy of an intravaginal triptorelin acetate (TA) gel as an ovulation-inducing agent in mares. In Exp 1, 24 mares were stratified by parity and age and randomly assigned to 3 treatment groups receiving either: 5 mL TA gel (500 μg TA; TA5), 10 mL TA gel (1,000 μg TA; TA10), or 5 mL vehicle gel only (CON). Following the appearance of a follicle ≥ 25 mm, blood samples were obtained every 24 h until treatment administration for measurement of luteinizing hormone (LH) concentrations. Once a follicle ≥ 35 mm in diameter was detected, treatment was administered intravaginally. Following treatment, blood samples were collected and ovaries were scanned via transrectal ultrasonography every 12 h until 48 h post-ovulation. Both TA5 and TA10 tended (P = 0.08) to experience a brief surge in LH by 12 h post-treatment. Regarding LH concentrations, there was a significant (P < 0.005) treatment by time interaction. The interval from treatment to ovulation was not different (P > 0.05) between groups, nor was there a difference (P > 0.05) in the percentage of mares ovulating within 48 h of treatment administration.