Comparison of Oocyte Maturity Rates in Recombinant Human Chorionic Go
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hertfordshire Medicines Management Committee (Hmmc) Nafarelin for Endometriosis Amber Initiation – Recommended for Restricted Use
HERTFORDSHIRE MEDICINES MANAGEMENT COMMITTEE (HMMC) NAFARELIN FOR ENDOMETRIOSIS AMBER INITIATION – RECOMMENDED FOR RESTRICTED USE Name: What it is Indication Date Decision NICE / SMC generic decision status Guidance (trade) last revised Nafarelin A potent agonistic The hormonal December Final NICE NG73 2mg/ml analogue of management of 2020 Nasal Spray gonadotrophin endometriosis, (Synarel®) releasing hormone including pain relief and (GnRH) reduction of endometriotic lesions HMMC recommendation: Amber initiation across Hertfordshire (i.e. suitable for primary care prescribing after specialist initiation) as an option in endometriosis Background Information: Gonadorelin analogues (or gonadotrophin-releasing hormone agonists [GnRHas]) include buserelin, goserelin, leuprorelin, nafarelin and triptorelin. The current HMMC decision recommends triptorelin as Decapeptyl SR® injection as the gonadorelin analogue of choice within licensed indications (which include endometriosis) link to decision. A request was made by ENHT to use nafarelin nasal spray as an alternative to triptorelin intramuscular injection during the COVID-19 pandemic. The hospital would provide initial 1 month supply, then GPs would continue for further 5 months as an alternative to the patient attending for further clinic appointments for administration of triptorelin. Previously at ENHT, triptorelin was the only gonadorelin analogue on formulary for gynaecological indications. At WHHT buserelin nasal spray 150mcg/dose is RED (hospital only) for infertility & endometriosis indications. Nafarelin nasal spray 2mg/ml is licensed for: . The hormonal management of endometriosis, including pain relief and reduction of endometriotic lesions. Use in controlled ovarian stimulation programmes prior to in-vitro fertilisation, under the supervision of an infertility specialist. Use of nafarelin in endometriosis aims to induce chronic pituitary desensitisation, which gives a menopause-like state maintained over many months. -

Degarelix for Treating Advanced Hormone- Dependent Prostate Cancer
CONFIDENTIAL UNTIL PUBLISHED NATIONAL INSTITUTE FOR HEALTH AND CARE EXCELLENCE Final appraisal determination Degarelix for treating advanced hormone- dependent prostate cancer This guidance was developed using the single technology appraisal (STA) process 1 Guidance 1.1 Degarelix is recommended as an option for treating advanced hormone-dependent prostate cancer, only in adults with spinal metastases who present with signs or symptoms of spinal cord compression. 1.2 People currently receiving treatment initiated within the NHS with degarelix that is not recommended for them by NICE in this guidance should be able to continue treatment until they and their NHS clinician consider it appropriate to stop. 2 The technology 2.1 Degarelix (Firmagon, Ferring Pharmaceuticals) is a selective gonadotrophin-releasing hormone antagonist that reduces the release of gonadotrophins by the pituitary, which in turn reduces the secretion of testosterone by the testes. Gonadotrophin- releasing hormone is also known as luteinising hormone-releasing hormone (LHRH). Because gonadotrophin-releasing hormone antagonists do not produce a rise in hormone levels at the start of treatment, there is no initial testosterone surge or tumour stimulation, and therefore no potential for symptomatic flares. National Institute for Health and Care Excellence Page 1 of 71 Final appraisal determination – Degarelix for treating advanced hormone-dependent prostate cancer Issue date: April 2014 CONFIDENTIAL UNTIL PUBLISHED Degarelix has a UK marketing authorisation for the ‘treatment of adult male patients with advanced hormone-dependent prostate cancer’. It is administered as a subcutaneous injection. 2.2 The most common adverse reactions with degarelix are related to the effects of testosterone suppression, including hot flushes and weight increase, or injection site reactions (such as pain and erythema). -

The Use of an Intravaginal Triptorelin Gel to Induce Ovulation in the Mare
THE USE OF AN INTRAVAGINAL TRIPTORELIN GEL TO INDUCE OVULATION IN THE MARE by CHELSEA D. SINCLAIR B.S., Clemson University, 2013 A THESIS submitted in partial fulfillment of the requirements for the degree MASTER OF SCIENCE Department of Animal Sciences and Industry College of Agriculture KANSAS STATE UNIVERSITY Manhattan, Kansas 2016 Approved by: Major Professor Dr. Joann M. Kouba Copyright CHELSEA D. SINCLAIR 2016 Abstract The objective of these studies was to investigate the efficacy of an intravaginal triptorelin acetate (TA) gel as an ovulation-inducing agent in mares. In Exp 1, 24 mares were stratified by parity and age and randomly assigned to 3 treatment groups receiving either: 5 mL TA gel (500 μg TA; TA5), 10 mL TA gel (1,000 μg TA; TA10), or 5 mL vehicle gel only (CON). Following the appearance of a follicle ≥ 25 mm, blood samples were obtained every 24 h until treatment administration for measurement of luteinizing hormone (LH) concentrations. Once a follicle ≥ 35 mm in diameter was detected, treatment was administered intravaginally. Following treatment, blood samples were collected and ovaries were scanned via transrectal ultrasonography every 12 h until 48 h post-ovulation. Both TA5 and TA10 tended (P = 0.08) to experience a brief surge in LH by 12 h post-treatment. Regarding LH concentrations, there was a significant (P < 0.005) treatment by time interaction. The interval from treatment to ovulation was not different (P > 0.05) between groups, nor was there a difference (P > 0.05) in the percentage of mares ovulating within 48 h of treatment administration. -
Triptorelin, Goserelin and Leuprorelin for Prostate
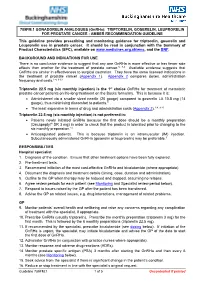
789FM.1 GONADORELIN ANALOGUES (GnRHa): TRIPTORELIN, GOSERELIN, LEUPRORELIN FOR PROSTATE CANCER - AMBER RECOMMENDATION GUIDELINE This guideline provides prescribing and monitoring guidance for triptorelin, goserelin and Leuprorelin use in prostate cancer. It should be read in conjunction with the Summary of Product Characteristics (SPC), available on www.medicines.org.uk/emc, and the BNF. BACKGROUND AND INDICATIONS FOR USE There is no conclusive evidence to suggest that any one GnRHa is more effective or has fewer side effects than another for the treatment of prostate cancer.5, 7-9 Available evidence suggests that GnRHa are similar in effectiveness to surgical castration. They have the same licensed indications in the treatment of prostate cancer (Appendix 1). Appendix 2 compares doses, administration frequency and costs.1-4, 9-13 Triptorelin 22.5 mg (six monthly injection) is the 1st choice GnRHa for treatment of metastatic prostate cancer patients on life-long treatment on the Bucks formulary. This is because it is: • Administered via a smaller sized needle (20 gauge) compared to goserelin LA 10.8 mg (14 gauge), thus minimising discomfort to patients.9 • The least expensive in terms of drug and administration costs (Appendix 2).1-4, 9-13 Triptorelin 22.5 mg (six monthly injection) is not preferred in: • Patients newly initiated GnRHa because the first dose should be a monthly preparation (Decapeptyl® SR 3 mg) in order to check that the product is tolerated prior to changing to the six monthly preparation.14 • Anticoagulated patients. This is because triptorelin is an intramuscular (IM) injection. Subcutaneously administered GnRHa (goserelin or leuprorelin) may be preferable.9 RESPONSIBILITIES Hospital specialist 1. -

Triptodur (Triptorelin)
Triptodur (triptorelin) (Intramuscular) Document Number: IC-0308 Last Review Date: 08/04/2020 Date of Origin: 08/01/2017 Dates Reviewed: 08/2017, 08/2018, 08/2019, 08/2020 I. Length of Authorization Coverage will be provided for 12 months and may be renewed. II. Dosing Limits A. Quantity Limit (max daily dose) [NDC Units]: • Triptodur 22.5 mg single-use kit: 1 kit per 168 days B. Max Units (per dose and over time) [HCPCS Units]: • 6 billable units per 168 days III. Initial Approval Criteria Coverage is provided in the following conditions: Central Precocious Puberty (CPP) † Ф 1,2-4,5 • Patient is between the ages of 2 and 13 years; AND • Onset of secondary sexual characteristics earlier than age 8 for girls and 9 for boys associated with pubertal pituitary gonadotropin activation; AND • Diagnosis is confirmed by pubertal gonadal sex steroid levels and a pubertal LH response to stimulation by native GnRH; AND • Bone age advanced greater than 2 standard deviations (SD) beyond chronological age; AND • Tumor has been ruled out by lab tests such as diagnostic imaging of the brain (to rule out intracranial tumor), pelvic/testicular/adrenal ultrasound (to rule out steroid secreting tumors), and human chorionic gonadotropin levels (to rule out a chorionic gonadotropin secreting tumor). † FDA Approved Indication(s); ‡ Compendia Recommended Indication(s); Ф Orphan Drug Proprietary & Confidential © 2020 Magellan Health, Inc. 1 IV. Renewal Criteria Authorizations can be renewed based on the following criteria: • Patient continues to meet indication-specific relevant criteria identified in section III; ; AND • Absence of unacceptable toxicity from the drug. -

Neoadjuvant Degarelix Versus Triptorelin in Premenopausal
original report Neoadjuvant Degarelix Versus Triptorelin in Premenopausal Patients Who Receive Letrozole for Locally Advanced Endocrine-Responsive Breast Cancer: A Randomized Phase II Trial Silvia Dellapasqua, MD1; Kathryn P. Gray, PhD2; Elisabetta Munzone, MD1; Daniela Rubino, MD3; Lorenzo Gianni, MD4; Harriet Johansson, PhD, MSc1; Giuseppe Viale, MD1;KarinRibi,PhD,MPH5;Jurg¨ Bernhard, PhD5; Roswitha Kammler5; Rudolf Maibach, PhD5; Manuela Rabaglio-Poretti, MD5; Barbara Ruepp, PharmD5; Angelo Di Leo, MD, PhD6;AlanS.Coates,MD7; Richard D. Gelber, PhD8,9; Meredith M. Regan, ScD9; Aron Goldhirsch, MD1; and Marco Colleoni, MD1, for the International Breast Cancer Study Group abstract PURPOSE To evaluate endocrine activity in terms of ovarian function suppression (OFS) of degarelix (a gonadotropin-releasing hormone [GnRH] antagonist) versus triptorelin (a GnRH agonist) in premenopausal patients receiving letrozole as neoadjuvant endocrine therapy for breast cancer. PATIENTS AND METHODS Premenopausal women with stage cT2 to 4b, any N, M0; estrogen receptor and progesterone receptor greater than 50%; human epidermal growth factor receptor 2–negative breast cancer were randomly assigned to triptorelin 3.75 mg administered intramuscularly on day 1 of every cycle or degarelix 240 mg administered subcutaneously (SC) on day 1 of cycle 1 then 80 mg SC on day 1 of cycles 2 through 6, both with letrozole 2.5 mg/day for six 28-day cycles. Surgery was performed 2 to 3 weeks after the last injection. ASSOCIATED Serum was collected at baseline, after 24 and 72 hours, at 7 and 14 days, and then before injections on cycles 2 CONTENT through 6. The primary end point was time to optimal OFS (time from the first injection to first assessment of Appendix centrally assessed estradiol level # 2.72 pg/mL [# 10 pmol/L] during neoadjuvant therapy). -

Recent Development of Non-Peptide Gnrh Antagonists
Review Recent Development of Non-Peptide GnRH Antagonists Feng-Ling Tukun 1, Dag Erlend Olberg 1,2, Patrick J. Riss 2,3,4, Ira Haraldsen 4, Anita Kaass 5 and Jo Klaveness 1,* 1 School of Pharmacy, University of Oslo, 0316 Oslo, Norway; [email protected] (F.-L.T.); [email protected] (D.E.O.) 2 Norsk Medisinsk Syklotronsenter AS, Postboks 4950 Nydalen, 0424 Oslo, Norway; [email protected] 3 Realomics SFI, Department of Chemistry, University of Oslo, 0316 Oslo, Norway 4 Department of neuropsychiatry and psychosomatic medicine, Oslo University Hospital, 4950 Oslo, Norway; [email protected] 5 Betanien Hospital, 3722 Skien, Norway; [email protected] * Correspondence: [email protected]; Tel.: +47-9177-6204 Received: 16 November 2017; Accepted: 4 December 2017; Published: 9 December 2017 Abstract: The decapeptide gonadotropin-releasing hormone, also referred to as luteinizing hormone-releasing hormone with the sequence (pGlu-His-Trp-Ser-Tyr-Gly-Leu-Arg-Pro-Gly-NH2) plays an important role in regulating the reproductive system. It stimulates differential release of the gonadotropins FSH and LH from pituitary tissue. To date, treatment of hormone-dependent diseases targeting the GnRH receptor, including peptide GnRH agonist and antagonists are now available on the market. The inherited issues associate with peptide agonists and antagonists have however, led to significant interest in developing orally active, small molecule, non-peptide antagonists. In this review, we will summarize all developed small molecule GnRH antagonists along with the most recent clinical data and therapeutic applications. Keywords: GnRH receptor; non-peptide GnRH antagonist 1. -

A Randomised Controlled Trial to Determine the Effect of Triptorelin on Reduction of Prostate Volume Pre- Radiotherapy Compared with Standard Therapy (Goserelin)
Research Article Clinics in Oncology Published: 22 Mar, 2019 A Randomised Controlled Trial to Determine the Effect of Triptorelin on Reduction of Prostate Volume Pre- Radiotherapy Compared with Standard Therapy (Goserelin) Amit Bahl1*, Amarnath Challapalli1, Rosemary Greenwood2, Hannah Kirk1, Krishna Garadi1, Karen Bobruk3, Rebecca Houlihan3, Katy Tucker3, Katrina Hurley3, Salah Al Buheissi4, Emma Gray5 and Raj Persad4 1Department of Clinical Oncology, University Hospitals Bristol NHS Foundation Trust, UK 2Department of Research Design Service, University Hospitals Bristol NHS Foundation Trust, UK 3Department of Research Unit, University Hospitals Bristol NHS Foundation Trust, UK 4Department of Urology, Bristol Urological Institute, UK 5Musgrove Park Hospital, Taunton, UK Abstract Objectives: To evaluate the non-inferiority of cytoreductive efficacy and effect on QoL of neoadjuvant Triptorelin as compared with Goserelin. Materials and Methods: Seventy-one patients with localised CaP were randomised to receive either neoadjuvant Triptorelin (n=37) or Goserelin (n=34). Prostate volume was measured (Transrectal Ultrasound (TRUS)), at baseline and 14 weeks after start of therapy. PSA, testosterone and QoL questionnaires were completed at baseline, 6, 10 and 14 weeks after start of therapy. Changes in TRUS volume, QoL scores; analysed as mean scores over the 4 treatment time points, were evaluated OPEN ACCESS using analysis of covariance, with baseline as covariate. *Correspondence: Results: The mean (S.D.) reduction in prostate volume after 12 weeks of Goserelin and Triptorelin Amit Bahl, Department of Clinical was 36.8% (18.3) and 30.7% (17.7), respectively (mean difference of prostate volume was 3.11 Oncology, University Hospitals Bristol cc). Twenty-nine out of 34 in Goserelin group (85.0%) and 33/37 patients in Triptorelin group NHS Foundation Trust, Bristol, (89.0%) achieved castrate levels of testosterone. -
Effects of an Extended-Interval Dosing Regimen of Triptorelin Depot on the Hormonal Profile of Patients with Endometriosis: Prospective Observational Study
Tse et al Effects of an extended-interval dosing regimen of triptorelin depot on the hormonal profile of patients with endometriosis: prospective observational study CY Tse, AMK Chow, SCS Chan Objective. To evaluate the suppression of pituitary gonadotrophins and ovarian steroid hormone with the administration of triptorelin depot at 6-weekly intervals. Design. Prospective observational study. Setting. Obstetrics and gynaecology department of a public hospital, Hong Kong. Patients. Consecutive patients with endometriosis, as diagnosed by laparoscopy or laparotomy from June 1998 through February 1999. Intervention. Administration of four doses of triptorelin depot 3.75 mg either subcutaneously or intramuscularly every 6 weeks (21 patients), or conventional 4-weekly six-dose regimen (five patients). Main outcome measures. Serum levels of 17-β-oestradiol, luteinizing hormone, and follicle-stimulating hormone; and pelvic pain symptoms. Results. For the patients receiving the extended-interval dosing regimen of triptorelin, the levels of oestradiol and luteinizing hormone, and the pain score were significantly reduced throughout the treatment period and up to 10 weeks after the injection of the last dose. The level of follicle-stimulating hormone increased slowly but was still significantly lower than pretreatment levels. The hormonal profile was similar to that of patients receiving the conventional regimen. Conclusion. The use of the extended-interval dosing regimen of triptorelin depot results in a consistent hypo- oestrogenised state, which is similar to that achieved by the conventional regimen and which would be con- sidered satisfactory for the medical treatment of pelvic endometriosis. The new regimen thus reduces the cost of treatment without compromising the effect on hormonal suppression. -

Prostate Cancer: Triptorelin (Decapeptyl SR)
pat hways Prostate cancer: triptorelin (Decapeptyl SR) Evidence summary Published: 13 January 2014 nice.org.uk/guidance/esnm30 Key points from the evidence The content of this evidence summary was up-to-date in January 2014. See summaries of product characteristics (SPCs), British national formulary (BNF) or the MHRA or NICE websites for up-to-date information. Summary In 2013, the licensed indications for the luteinising hormone-releasing hormone (LHRH) agonist, triptorelin (Decapeptyl SR), were extended to include 2 new indications for prostate cancer: neoadjuvant treatment before radiotherapy in high-risk localised or locally advanced disease, and adjuvant treatment to radical prostatectomy in locally advanced disease at high risk of progression. These are based on limited clinical data on the use of triptorelin and extrapolation from evidence for other LHRH agonists. © NICE 2018. All rights reserved. Subject to Notice of rights (https://www.nice.org.uk/terms-and- Page 1 of conditions#notice-of-rights). 17 Prostate cancer: triptorelin (Decapeptyl SR) (ESNM30) Effectiveness Safety In 2 single-arm randomised controlled trials (n=28 An initial increase in testosterone and n=50), compared with baseline, neoadjuvant levels can cause transient triptorelin for 2 or 3 months before radiotherapy worsening of signs and symptoms statistically significantly reduced prostate olumev of prostate cancer in the first (p<0.001). In 1 study (n=50) it also reduced weeks. prostate-specific antigen levels (p<0.001). LHRH agonists may reduce bone There are no clinical studies of triptorelin as mineral density, increase the risk of adjuvant treatment to radical prostatectomy. depression and cause metabolic changes (glucose intolerance and increased risk of cardiovascular disease). -

The Effects of Different Gonadotropin Releasing Hormone Analogues in IVF Cycles
Vol. 10, No. 3, 2005 Middle East Fertility Society Journal © Copyright Middle East Fertility Society The effects of different gonadotropin releasing hormone analogues in IVF cycles Cem Fiçicioğlu, M.D., Ph.D., Assoc.Prof. Seval Taşdemir, M.D. Tayfun Kutlu, M.D. Leyla Altuntaş, M.D. Zeynep Kamil Women and Children's Hospital, Reproductive Medicine-Infertility & IVF unit, Istanbul. ABSTRACT Objective: To compare Triptorelin, Leuprolide acetate and Nafarelin sodium in women undergoing controlled ovarian hyperstimulation for in vitro fertilization cycles. Settings: Zeynep Kamil Women and Children's Hospital Reproductive Endocrinology - Infertility - IVF Center. Material and Methods: Sixty patients were haphazardly distributed for each GnRH-a group. GnRH-a was administrated, starting on the 21st day of menstrual cycles for the long protocol: Triptorelin (Decapeptyl, 0.1 mg) as 0.1 mg/day SC, leuprolide (Lucrine, 5 mg flacon) as 0.5 mg/day SC and nafarelin (Synarel, 2 mg/mi nasal spray) as 200 micrograms to each nostril with a daily total dosage of 800 micrograms. The responses from each group were compared on the basis of duration of stimulation, total dosage of gonadotropin, E2 values on day 5, the down regulation duration, cyst formation, E2 values on the 1st day of stimulation and HCG, progesterone values and endometrial thickness on the HCG day, the number oocytes picked up, fertilization rates, the number of transferred embryos, pregnancy and implantation ratios. Results: Evaluating Triptorelin (T), Leuprolide (LA) and Nafarelin (NA) groups respectively, E2 values on the 1st day of menstrual cycles, measured to confirm the down regulation for each GnRH-a, were 24.67 pg/ml, 21.23 pg/ml, 29.62 pg/ml (p<0.05); the total gonadotropin usage (ampoules) were 47.15 ± 12.97, 39.45 ± 13.97, 36.72 ± 13.14 (p<0.05); the number of retrieved oocytes were 9,89 ± 5,98, 10,50 ± 3,69 and 9,19 ± 5,31 (p>0,05); the fertilization rates were 89%, 100% and 100% (p>0.05). -

Triptodur™ (Triptorelin) – New Drug Approval
Triptodur™ (triptorelin) – New drug approval • On June 30, 2017, Arbor Pharmaceuticals announced the FDA approval of Triptodur (triptorelin) extended-release injectable suspension for the treatment of pediatric patients ≥ 2 years of age with central precocious puberty (CPP). • Gonadotropin-releasing hormone (GnRH)-dependent CPP is defined by pubertal development occurring before the age of 8 years in girls and 9 years in boys. CPP is a rare disease occurring in about 1 out of every 5,000 to 10,000 children and is more common in girls than boys. • Triptorelin is the first GnRH agonist to offer once-every 6 month dosing for the treatment of CPP in the U.S. • The efficacy and safety of Triptodur were based on a single-arm, open-label study of 44 children with CPP and naïve to previous GnRH treatment administered Triptodur every 24 weeks over a 12 month period. Triptodur demonstrated a return to pre-pubertal luteinizing hormone (LH) levels in 93% of patients, with pre-pubertal LH suppression maintained at 12 months by 98% of patients. • Triptodur is contraindicated during pregnancy, and in individuals with a known hypersensitivity to triptorelin, any other component of the product, or other GnRH agonists or GnRH. • Warnings and precautions of Triptodur include initial rise of gonadotropins and sex steroid levels, psychiatric events, and convulsions. • The most common adverse reactions (≥ 4.5%) with Triptodur use were injection site reactions, menstrual (vaginal) bleeding, hot flush, headache, cough, and infections (bronchitis, gastroenteritis, influenza, nasopharyngitis, otitis externa, pharyngitis, sinusitis, and upper respiratory tract infection). • The recommended dosage of Triptodur is 22.5 mg administered as a single intramuscular injection once every 24 weeks.