Elagolix for Treating Endometriosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Study Protocol and Documented in the Subject Dispensing Log
Protocol Title of trial: A Multicenter, Double-Blind, Randomized, Placebo-Controlled Study Evaluating Three Doses of Subcutaneous Pulsatile GnRH Administered via OmniPod Pump for Ovulation Induction in Female Subjects with Primary Amenorrhea with Hypogonadotropic Hypogonadism NCT number: NCT01976728 Sponsor trial code: 000070 Date: 06 Dec 2017 Gonadorelin Acetate, FE Trial Code: 000070 Date: 06 Dec 2017 999037, FE 999903 E-Protocol Amendment-21975;1.0 No Specified Dosage Form and Strength Supersedes: None Clinical Trial Protocol - Amendment 7 Page 1 of 82 CLINICAL TRIAL PROTOCOL A Multicenter, Double-Blind, Randomized, Placebo-Controlled Study Evaluating Three Doses of Subcutaneous Pulsatile GnRH Administered via OmniPod Pump for Ovulation Induction in Female Subjects with Primary Amenorrhea with Hypogonadotropic Hypogonadism Trial Code 000070 Consolidated Protocol Incorporating Amendments 1-7 IND Number: 22,278 Investigational Medicinal Product: LutrePulse OmniPod Indication: Primary Hypothalamic Amenorrhea Phase: III Name and Address of Sponsor: Ferring International Pharmascience Center U.S., Inc. 100 Interpace Parkway Parsippany, NJ 07054 P: 973-796-1600 F: 973-796-1660 GCP Statement: This trial will be performed in compliance with GCP. The information in this document is confidential and is proprietary to Ferring International Pharmascience Center U.S. or another company within the Ferring Group. It is understood that information in this document shall not be disclosed to any third party, in any form, without prior written consent -

Progestin-Only Systemic Hormone Therapy for Menopausal Hot Flashes
EDITORIAL Progestin-only systemic hormone therapy for menopausal hot flashes Clinicians treating postmenopausal hot flashes often recommend “systemic estrogen treatment.” However, progestin-only therapy also can effectively treat hot flashes and is an option for women with a contraindication to estrogen therapy. Robert L. Barbieri, MD Editor in Chief, OBG MANAGEMENT Chair, Obstetrics and Gynecology Brigham and Women’s Hospital Boston, Massachusetts Kate Macy Ladd Professor of Obstetrics, Gynecology and Reproductive Biology Harvard Medical School he field of menopause medi- women. In one study, 133 postmeno- in postmenopausal women with cine is dominated by studies pausal women with an average age an American Heart Association risk T documenting the effective- of 55 years and approximately 3 years score greater than 10% over 10 years.3 ness of systemic estrogen or estro- from their last menstrual period were Additional contraindications to sys- gen-progestin hormone therapy for randomly assigned to 12 weeks of temic estrogen include women with the treatment of hot flashes caused treatment with placebo or micronized cardiac disease who have a throm- by hypoestrogenism. The effective- progesterone 300 mg daily taken at bophilia, such as the Factor V Leiden ness of progestin-only systemic bedtime.1 Mean serum progesterone mutation.4 hormone therapy for the treatment levels were 0.28 ng/mL (0.89 nM) and For women who are at high risk of hot flashes is much less studied 27 ng/mL (86 nM) in the women taking for estrogen-induced cardiovascu- and seldom is utilized in clinical placebo and micronized progesterone, lar events, micronized progesterone practice. -
Personalized ADT
Personalized ADT Thomas Keane MD Conflicts • Ferring • Tolemar • Bayer • Astellas • myriad Personalized ADT for the Specific Paent • Cardiac • OBesity and testosterone • Fsh • High volume metastac disease • Docetaxol • Significant LUTS Cardiovascular risk profile and ADT Is there a difference? Degarelix Belongs to a class of synthe@c drug, GnRH antagonist (Blocker) GnRH pGlu His Trp Ser Tyr Gly Leu Arg Pro Gly NH2 Leuprolide D-Leu NEt Goserelin D-Ser NH2 LHRH agonists Triptorelin D-Trp NH2 Buserelin D-Ser NEt Degarelix D-NaI D-Cpa D-PaI Aph D-Aph D-Ala NH2 N-Me ABarelix D-NaI D-Cpa D-PaI D-Asn Lys D-Ala NH2 Tyr GnRH antagonists Cetrorelix D-NaI D-Cpa D-PaI D-Cit D-Ala NH2 Ganirelix D-NaI D-CPa D-PaI D-hArg D-hArg D-Ala NH2 Millar RP, et al. Endocr Rev 2004;25:235–75 Most acute CVD events are caused By rupture of a vulnerable atherosclero@c plaque The vulnerable plaque – thin cap with inflammaon Inflammation Plaque instability is at the heart of cardiovascular disease Stable plaque Vulnerable plaque Lumen Lumen Lipid core Lipid core FiBrous cap FiBrous cap Thick Cap Thin Rich in SMC and matrix Composion Rich in inflammatory cells: proteoly@c ac@vity Poor Lipid Rich Inflammatory Inflammatory state Highly inflammatory LiBBy P. Circulaon 1995;91:2844-2850 Incidence of Both prostate cancer and CV events is highest in older men Prostate cancer CV events 3500 3500 Prostate cancer All CV disease Major CV events 3000 3000 2827.1 2500 2500 2338.9 2000 2000 1719.7 1500 1500 1152.6 1008.7 1038.7 1000 1000 641.2 545.2 571.1 Age-specific incidence per 100,000 person-years 500 500 246.9 133.7 4.3 0 0 40-49 50-59 60-69 70-79 80-89 90-99 40-49 50-59 60-69 70-79 80-89 90-99 CV, cardiovascular Major CV events = myocardial infarc@on, stroke, or death due to CV disease All CV disease = major CV events + self-reported angina or revascularisaon procedures Driver, et al. -

6 Ways Your Brain Transforms During Menopause
6 Ways Your Brain Transforms During Menopause By Aviva Patz Movies and TV shows have gotten a lot of laughs out of menopause, with its dramatic hot flashes and night sweats. But the midlife transition out of our reproductive years—marked by yo-yoing of hormones, mostly estrogen—is a serious quality-of-life issue for many women, and as we're now learning, may leave permanent marks on our health. "There is a critical window hypothesis in that what is done to treat the symptoms and risk factors during perimenopause predicts future health and symptoms," explains Diana Bitner, MD, assistant professor at Michigan State University College of Human Medicine and author of I Want to Age Like That: Healthy Aging Through Midlife and Menopause. "If women act on the mood changes in perimenopause and get healthy and take estrogen, the symptoms are much better immediately and also lifelong." (Going through menopause and your hormones are out of whack? Then check out The Hormone Reset Diet to balance your hormones and lose weight.) For many decades, the mantra has been that the only true menopausal symptoms are hot flashes and vaginal dryness. Certainly they're the easiest signs to spot! But we have estrogen receptors throughout the brain and body, so when estrogen levels change, we experience the repercussions all over—especially when it comes to how we think and feel. Two large studies, including one of the nation's longest longitudinal investigations, have revealed that there's a lot going on in the brain during this transition. "Before it was hard to tease out: How much of this is due to the ovaries aging and how much is due to the whole body aging?" says Pauline Maki, PhD, professor of psychiatry and psychology at the University of Illinois at Chicago and Immediate Past President of the North American Menopause Society (NAMS). -
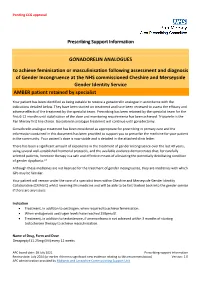
Prescribing Support Information GONADORELIN ANALOGUES To
Pending CCG approval Prescribing Support Information GONADORELIN ANALOGUES to achieve feminisation or masculinisation following assessment and diagnosis of Gender Incongruence at the NHS commissioned Cheshire and Merseyside Gender Identity Service AMBER patient retained by specialist Your patient has been identified as being suitable to receive a gonadorelin analogue in accordance with the indications detailed below. They have been started on treatment and have been reviewed to assess the efficacy and adverse effects of the treatment by the specialist team. Prescribing has been retained by the specialist team for the first 6-12 months until stabilisation of the dose and monitoring requirements has been achieved. Triptorelin is the Pan Mersey first line choice. Gonadorelin analogue treatment will continue until gonadectomy. Gonadorelin analogue treatment has been considered as appropriate for prescribing in primary care and the information contained in this document has been provided to support you to prescribe the medicine for your patient in the community. Your patient’s dose is now stable and is detailed in the attached clinic letter. There has been a significant amount of experience in the treatment of gender incongruence over the last 40 years, using several well-established hormonal protocols, and the available evidence demonstrates that, for carefully selected patients, hormone therapy is a safe and effective means of alleviating the potentially debilitating condition of gender dysphoria.1.2 Although these medicines are not licensed for the treatment of gender incongruence, they are medicines with which GPs may be familiar. Your patient will remain under the care of a specialist team within Cheshire and Merseyside Gender Identity Collaborative (CMAGIC) whilst receiving this medicine and will be able to be fast tracked back into the gender service if there are any issues. -

Hertfordshire Medicines Management Committee (Hmmc) Nafarelin for Endometriosis Amber Initiation – Recommended for Restricted Use
HERTFORDSHIRE MEDICINES MANAGEMENT COMMITTEE (HMMC) NAFARELIN FOR ENDOMETRIOSIS AMBER INITIATION – RECOMMENDED FOR RESTRICTED USE Name: What it is Indication Date Decision NICE / SMC generic decision status Guidance (trade) last revised Nafarelin A potent agonistic The hormonal December Final NICE NG73 2mg/ml analogue of management of 2020 Nasal Spray gonadotrophin endometriosis, (Synarel®) releasing hormone including pain relief and (GnRH) reduction of endometriotic lesions HMMC recommendation: Amber initiation across Hertfordshire (i.e. suitable for primary care prescribing after specialist initiation) as an option in endometriosis Background Information: Gonadorelin analogues (or gonadotrophin-releasing hormone agonists [GnRHas]) include buserelin, goserelin, leuprorelin, nafarelin and triptorelin. The current HMMC decision recommends triptorelin as Decapeptyl SR® injection as the gonadorelin analogue of choice within licensed indications (which include endometriosis) link to decision. A request was made by ENHT to use nafarelin nasal spray as an alternative to triptorelin intramuscular injection during the COVID-19 pandemic. The hospital would provide initial 1 month supply, then GPs would continue for further 5 months as an alternative to the patient attending for further clinic appointments for administration of triptorelin. Previously at ENHT, triptorelin was the only gonadorelin analogue on formulary for gynaecological indications. At WHHT buserelin nasal spray 150mcg/dose is RED (hospital only) for infertility & endometriosis indications. Nafarelin nasal spray 2mg/ml is licensed for: . The hormonal management of endometriosis, including pain relief and reduction of endometriotic lesions. Use in controlled ovarian stimulation programmes prior to in-vitro fertilisation, under the supervision of an infertility specialist. Use of nafarelin in endometriosis aims to induce chronic pituitary desensitisation, which gives a menopause-like state maintained over many months. -

CRPT-113Hrpt565-Pt2.Pdf
113TH CONGRESS REPT. 113–565 " ! 2d Session HOUSE OF REPRESENTATIVES Part 2 IMPROVING REGULATORY TRANSPARENCY FOR NEW MEDICAL THERAPIES ACT SEPTEMBER 19, 2014.—Committed to the Committee of the Whole House on the State of the Union and ordered to be printed Mr. GOODLATTE, from the Committee on the Judiciary, submitted the following R E P O R T [To accompany H.R. 4299] [Including cost estimate of the Congressional Budget Office] The Committee on the Judiciary, to whom was referred the bill (H.R. 4299) to amend the Controlled Substances Act with respect to drug scheduling recommendations by the Secretary of Health and Human Services, and with respect to registration of manufac- turers and distributors seeking to conduct clinical testing, having considered the same, report favorably thereon with an amendment and recommend that the bill as amended do pass. CONTENTS Page The Amendment ...................................................................................................... 1 Purpose and Summary ............................................................................................ 2 Background and Need for the Legislation ............................................................. 2 Hearings ................................................................................................................... 3 Committee Consideration ........................................................................................ 3 Committee Votes ..................................................................................................... -

Degarelix for Treating Advanced Hormone- Dependent Prostate Cancer
CONFIDENTIAL UNTIL PUBLISHED NATIONAL INSTITUTE FOR HEALTH AND CARE EXCELLENCE Final appraisal determination Degarelix for treating advanced hormone- dependent prostate cancer This guidance was developed using the single technology appraisal (STA) process 1 Guidance 1.1 Degarelix is recommended as an option for treating advanced hormone-dependent prostate cancer, only in adults with spinal metastases who present with signs or symptoms of spinal cord compression. 1.2 People currently receiving treatment initiated within the NHS with degarelix that is not recommended for them by NICE in this guidance should be able to continue treatment until they and their NHS clinician consider it appropriate to stop. 2 The technology 2.1 Degarelix (Firmagon, Ferring Pharmaceuticals) is a selective gonadotrophin-releasing hormone antagonist that reduces the release of gonadotrophins by the pituitary, which in turn reduces the secretion of testosterone by the testes. Gonadotrophin- releasing hormone is also known as luteinising hormone-releasing hormone (LHRH). Because gonadotrophin-releasing hormone antagonists do not produce a rise in hormone levels at the start of treatment, there is no initial testosterone surge or tumour stimulation, and therefore no potential for symptomatic flares. National Institute for Health and Care Excellence Page 1 of 71 Final appraisal determination – Degarelix for treating advanced hormone-dependent prostate cancer Issue date: April 2014 CONFIDENTIAL UNTIL PUBLISHED Degarelix has a UK marketing authorisation for the ‘treatment of adult male patients with advanced hormone-dependent prostate cancer’. It is administered as a subcutaneous injection. 2.2 The most common adverse reactions with degarelix are related to the effects of testosterone suppression, including hot flushes and weight increase, or injection site reactions (such as pain and erythema). -

Tanibirumab (CUI C3490677) Add to Cart
5/17/2018 NCI Metathesaurus Contains Exact Match Begins With Name Code Property Relationship Source ALL Advanced Search NCIm Version: 201706 Version 2.8 (using LexEVS 6.5) Home | NCIt Hierarchy | Sources | Help Suggest changes to this concept Tanibirumab (CUI C3490677) Add to Cart Table of Contents Terms & Properties Synonym Details Relationships By Source Terms & Properties Concept Unique Identifier (CUI): C3490677 NCI Thesaurus Code: C102877 (see NCI Thesaurus info) Semantic Type: Immunologic Factor Semantic Type: Amino Acid, Peptide, or Protein Semantic Type: Pharmacologic Substance NCIt Definition: A fully human monoclonal antibody targeting the vascular endothelial growth factor receptor 2 (VEGFR2), with potential antiangiogenic activity. Upon administration, tanibirumab specifically binds to VEGFR2, thereby preventing the binding of its ligand VEGF. This may result in the inhibition of tumor angiogenesis and a decrease in tumor nutrient supply. VEGFR2 is a pro-angiogenic growth factor receptor tyrosine kinase expressed by endothelial cells, while VEGF is overexpressed in many tumors and is correlated to tumor progression. PDQ Definition: A fully human monoclonal antibody targeting the vascular endothelial growth factor receptor 2 (VEGFR2), with potential antiangiogenic activity. Upon administration, tanibirumab specifically binds to VEGFR2, thereby preventing the binding of its ligand VEGF. This may result in the inhibition of tumor angiogenesis and a decrease in tumor nutrient supply. VEGFR2 is a pro-angiogenic growth factor receptor -

Guidance for Industry Postmarketing Safety Reporting for Human Drug and Biological Products Including Vaccines
Guidance for Industry Postmarketing Safety Reporting for Human Drug and Biological Products Including Vaccines DRAFT GUIDANCE This guidance document is being distributed for comment purposes only. Comments and suggestions regarding this draft document should be submitted within 60 days of publication in the Federal Register of the notice announcing the availability of the draft guidance. Submit comments to Dockets Management Branch (HFA-305), Food and Drug Administration, 5630 Fishers Lane, rm. 1061, Rockville, MD 20857. All comments should be identified with the docket number listed in the notice of availability that publishes in the Federal Register. For questions on the content of the draft document contact (CDER) Min Chen, 301-827- 3169 (phone); 301-827-5190 (fax), or (CBER) Miles Braun, 301-827-3974 (phone); 301- 827-3529 (fax). U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER) Center for Biologics Evaluation and Research (CBER) March 2001 G:\4177dft.doc Guidance for Industry Postmarketing Safety Reporting for Human Drug and Biological Products Including Vaccines Additional copies are available from: Drug Information Branch (HFD-210) Center for Drug Evaluation and Research (CDER) 5600 Fishers Lane, Rockville, MD 20857 (Tel) 301-827-4570 Internet at http://www.fda.gov/cder/guidance/index.htm or Office of Communication, Training and Manufacturers Assistance (HFM-40) Center for Biologics Evaluation and Research (CBER) 1401 Rockville Pike, Rockville, MD 20852-1448 (Fax) 1-888-CBERFAX or 301-827-3844 (Voice Information) 1-800-835-4709 or 301-827-1800 Internet at http://www.fda.gov/cber/guidelines.htm U.S. -

Degarelix Acetate (Firmagon) Reference Number: PA.CP.PHAR.170 Effective Date: 01/18 Last Review Date: 10/18 Revision Log
Clinical Policy: Degarelix Acetate (Firmagon) Reference Number: PA.CP.PHAR.170 Effective Date: 01/18 Last Review Date: 10/18 Revision Log Description The intent of the criteria is to ensure that patients follow selection elements established by Pennsylvania Health and Wellness® clinical policy for the use of Degarelix Acetate (Firmagon®). FDA Approved Indication(s) Firmagon is indicated for treatment of advanced prostate cancer. Policy/Criteria It is the policy of Pennsylvania Health and Wellness that Firmagon is medically necessary when the following criteria are met: I. Initial Approval Criteria A. Prostate Cancer (must meet all): 1. Diagnosis of prostate cancer; 2. Prescribed by or in consultation with an oncologist; 3. Request meets one of the following (a, b or c): a. Starting dose does not exceed 240 mg given as two injections of 120 mg each; b. Maintenance dose does not exceed 80 mg as a single injection per 28 days; c. Dose is supported by practice guidelines or peer-reviewed literature for the relevant off- label use (prescriber must submit supporting evidence). Approval duration: 12 months B. Other diagnoses/indications: Refer to PA.CP.PMN.53 1. The following NCCN recommended uses for Firmagon, meeting NCCN categories 1, 2a, or 2b, are approved per the PA.CP.PMN.53: II. Continued Approval A. Prostate Cancer (must meet all): 1. Currently receiving medication via Pennsylvania Health and Wellness benefit or member has previously met approval criteria or the Continuity of Care policy (PA.LTSS.PHAR.01) applies; 2. Member is responding positively to therapy; 3. If request is for a dose increase, request meets one of the following: a. -

Duloxetine and Escitalopram for Hot Flushes: Efficacy and Compliance in Breast Cancer Survivors
Original Article Duloxetine and escitalopram for hot flushes: efficacy and compliance in breast cancer survivors N. BIGLIA, MD, PHD, Gynaecology and Obstetrics Unit, Umberto I Hospital, Department of Surgical Sciences, University of Turin, Turin, V.E. BOUNOUS, MD, Gynaecology and Obstetrics Unit, Umberto I Hospital, Department of Surgical Sciences, University of Turin, Turin, T. SUSINI, MD, PHD, Breast Unit Department of Health Science, OB & GYN Section, AOU Careggi, School of Medicine, University of Florence, Florence, S. PECCHIO, MD, Gynaecology and Obstetrics Unit, Umberto I Hospital, Department of Surgical Sciences, University of Turin, Turin, L.G. SGRO, MD, PHD, Gynaecology and Obstetrics Unit, Umberto I Hospital, Department of Surgical Sciences, University of Turin, Turin, V. TUNINETTI, Gynaecology and Obstetrics Unit, Umberto I Hospital, Department of Surgical Sciences, University of Turin, Turin, & R. TORTA, MD, PHD, Psycho-Oncology Unit, Department of Neurosciences, University of Turin, Turin, Italy BIGLIA N., BOUNOUS V.E., SUSINI T., PECCHIO S., SGRO L.G., TUNINETTI V. & TORTA R. (2016) Euro- pean Journal of Cancer Care Duloxetine and escitalopram for hot flushes: efficacy and compliance in breast cancer survivors Selective serotonin reuptake inhibitors (SSRI) and serotonin–norepinephrine reuptake inhibitors (SNRI) might be an effective treatment for hot flushes (HFs) in breast cancer survivors (BCSs). This study aims to compare the efficacy and tolerability of duloxetine (SNRI) versus escitalopram (SSRI) in reducing frequency and severity of HFs in BCSs and to assess the effect on depression. Thirty-four symptomatic BCSs with emotional impairment received randomly duloxetine 60 mg daily or escitalopram 20 mg daily for 12 weeks. Patients were asked to record in a diary HF frequency and severity at baseline and after 4 and 12 weeks of treatment.