Attempted Suicide Patients Risk Factors and Suicide
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Prison Suicide: an Overview and Guide to Prevention National Institute of Corrections
U.S. Department of Justice National Institute of Corrections Prison Suicide: An Overview and Guide to Prevention National Institute of Corrections Morris L. Thigpen, Director Susan M. Hunter, Chief Prisons Division John E. Moore, Project Manager Prison Suicide: An Overview and Guide to Prevention By Lindsay M. Hayes Project Director National Center on Institutions and Alternatives Mansfield, Massachusetts June 1995 This document was prepared under grant number 93P01GHU1 from the National Institute of Corrections, U.S. Department of Justice. Points of view or opinions stated in this document are those of the author(s) and do not necessarily represent the official position or policies of the U.S. Department of Justice. Copyright © 1995 by the National Center on Institutions and Alternatives The National Institute of Corrections reserves the right to reproduce, publish, translate, or otherwise use, and to authorize others to publish and use all or any part of the copyrighted material contained in this publication. ii TABLE OF CONTENTS FOREWORD .......................................................................................................................................v PREFACE AND ACKNOWLEDGMENTS ..................................................................................vi 1. INTRODUCTION AND LITERATURE REVIEW ..............................................................1 2. NATIONAL AND STATE STANDARDS FOR PRISON SUICIDE PREVENTION ...........................................................................................................8 -

Fresno County Community-Based Suicide Prevention Strategic Plan
Fresno County Community-Based Suicide Prevention Strategic Plan Written by DeQuincy A. Lezine, PhD and Noah J. Whitaker, MBA For those who struggle, those who have been lost, those left behind, may you find hope… Fresno Cares 2018 Introduction 4 Background and Rationale 5 How Suicide Impacts Fresno County 5 The Fresno County Suicide Prevention Collaborative 7 History 8 Capacity-Building 9 Suicide Prevention in Schools (AB 2246) 10 Workgroups 10 Data 11 Communication 11 Learning & Education 12 Health Care 13 Schools 14 Justice & First Responders 15 Understanding Suicide 16 Overview: the Suicidal crisis within life context 17 The Suicidal Crisis: Timeline of suicidal crisis and prevention 22 Levels of Influence: The Social-Ecological Model 23 Identifying and Characterizing Risk 24 Understanding How Risk Escalates Into Suicidal Thinking 26 Warning Signs: Recognizing when someone may be suicidal 27 Understanding How Suicidal Thinking Turns into Behavior 28 Understanding How a Suicide Attempt Becomes a Suicide 28 Understanding How Suicide Affects Personal Connections 29 Stopping the Crisis Path 30 Comprehensive Suicide Prevention in Fresno County 31 Health and Wellness Promotion 34 Prevention (Universal strategies) 34 Early Intervention (Selective strategies) 35 Clinical Intervention (Selective strategies) 35 Crisis Intervention and Postvention (Indicated strategies) 36 Where We are Now: Needs and Assets in Fresno County 37 Suicidal Thoughts and Feelings 37 Suicide Attempts 40 1 Suicide 41 Understanding -

Community Conversations to Inform Youth Suicide Prevention
2018 Community Conversations to Inform Youth Suicide Prevention A STUDY OF YOUTH SUICIDE IN FOUR COLORADO COUNTIES Presented to Attorney General Cynthia H. Coffman Colorado Office of the Attorney General By Health Management Associates 2 TABLE OF CONTENTS Acknowledgements............................................................................................................................................................. 3 Executive Summary..............................................................................................................................................................4 Introduction..........................................................................................................................................................................11 Scope of the Problem........................................................................................................................................................11 Key Stakeholder Interviews...........................................................................................................................................13 Community Focus Groups.............................................................................................................................................. 17 School Policies & Procedures........................................................................................................................................27 Traditional Media & Suicide.......................................................................................................................................... -

Answer Key: Suicide Prevention
Personal Health Series Suicide Quiz Answer Key 1. List four factors that can increase a teen’s risk of suicide: Any four of the following: a psychological disorder, especially depression, bipolar disorder, and alcohol and/or drug use; feelings of hopelessness and worthlessness; previous suicide attempt; family history of depression or suicide; emotional, physical, or sexual abuse; lack of a support network, poor relationships with parents or peers, and feelings of social isolation; dealing with bisexuality or homosexuality in an unsupportive family or community or hostile school environment; perfectionism. 2. True or false: If a person talks about suicide, it means he or she is just looking for attention and won’t go through with it. 3. True or false: The danger of suicide has passed when a person begins to cheer up. 4. List four warning signs that someone is thinking about suicide: Any four of the following: talking about suicide or death in general; hinting he/she might not be around anymore; talking about feeling hopeless or feeling guilty; pulling away from friends or family; writing songs, poems, or letters about death, separation, or loss; giving away treasured possessions; losing the desire to do favorite things or activities; having trouble concentrating or thinking clearly; changing eating or sleeping habits; engaging in risky or self-destructive behaviors; losing interest in school and/or extra-curricular activities. 5. True or false: Once a person is suicidal, he or she is suicidal forever. 6. True or false: Most teens who attempt suicide really intend to die. 7. True or false: If a friend tells you she’s considering suicide and swears you to secrecy, you have to keep your promise. -

The Most Common Method of Suicide in Tehran 2000–2004
See discussions, stats, and author profiles for this publication at: https://www.researchgate.net/publication/23182135 The Most Common Method of Suicide in Tehran 2000–2004 Article in Crisis The Journal of Crisis Intervention and Suicide Prevention · February 2008 DOI: 10.1027/0227-5910.29.3.164 · Source: PubMed CITATIONS READS 7 69 4 authors, including: Mohsen Rezaeian Rafsanjan University of Medical Sciences 240 PUBLICATIONS 1,176 CITATIONS SEE PROFILE Some of the authors of this publication are also working on these related projects: Suicide Mortality in Kermanshah Province View project nasal carriage of s. aureus among health workers in Iran View project All content following this page was uploaded by Mohsen Rezaeian on 11 December 2015. The user has requested enhancement of the downloaded file. M. Razaeian et al.: Method© 2008 ofCrisis Suicide Hogrefe2008; in Tehran Vol.& Huber 29(3):164–166 2000–2004 Publishers Short Report The Most Common Method of Suicide in Tehran 2000–2004 Implications for Prevention Mohsen Razaeian1,2, Maryam Mohammadi2, Malihe Akbari2, and Maryam Maleki2 1Social Medicine Department, School of Medicine, Rafsanjan University of Medical Sciences 2Public Health Department, School of Health, Shaheed Beheshti University of Medical Sciences, both Tehran, Iran Abstract. The likelihood of completing suicide depends to some extent on knowledge of effective means and also on the availability and/or acceptability of such methods. Since studying suicide methods may have an implication for prevention, the focus of this study was on the most favored method of suicide in Tehran, Iran. The study uses confirmed suicide data provided by the Beheshet Zahra Organization (BZO), which gathers all mortality data within Tehran and enters them into a computerized database, from which the relevant information for all the recorded suicide cases during the year 2000 to 2004 were obtained and analyzed. -
National Guidelines: Responding to Grief, Trauma, and Distress After a Suicide
Responding to Grief, Trauma, and Distress After a Suicide: U.S. National Guidelines Survivors of Suicide Loss Task Force April 2015 Blank page Responding to Grief, Trauma, and Distress After a Suicide: U.S. National Guidelines Table of Contents Front Matter Acknowledgements ...................................................................................................................................... i Task Force Co-Leads, Members .................................................................................................................. ii Reviewers .................................................................................................................................................... ii Preface ....................................................................................................................................................... iii National Guidelines Executive Summary ..................................................................................................................................... 1 Introduction ................................................................................................................................................ 4 Terminology: “Postvention” and “Loss Survivor” ....................................................................................... 4 Development and Purpose of the Guidelines ............................................................................................. 6 Audience of the Guidelines ........................................................................................................................ -

National Study of Jail Suicide: 20 Years Later Foreword
U.S. Department of Justice National Institute of Corrections U.S. Department of Justice National Institute of Corrections 320 First Street, NW Washington, DC 20534 Morris L. Thigpen Director Thomas J. Beauclair Deputy Director Virginia A. Hutchinson Chief, Jails Division Fran Zandi Program Manager National Institute of Corrections www.nicic.gov Lindsay M. Hayes, Project Director National Center on Institutions and Alternatives April 2010 NIC Accession Number 024308 This document was prepared under cooperative agreement number 06J47GJM0 from the National Institute of Corrections, U.S. Department of Justice. Points of view or opinions stated in this document are those of the author and do not necessarily represent the official position or policies of the U.S. Department of Justice. Contents Foreword .......................................................................................................... vii Acknowledgments ..............................................................................................ix Executive Summary ............................................................................................xi Chapter 1. Introduction ...................................................................................... 1 Prior Jail Suicide Research .................................................................................... 2 A Word About Suicide Victim Profiles .................................................................... 3 Death in Custody Reporting Act of 2000............................................................... -

Trend of Suicide in Kermanshah During 11 Years (2004 to 2014), Iran A.H
Journal of Medical and Biomedical Sciences (2017) 6(2): 17- 24 © UDS Publishers Limited All Right Reserved 2026-6294 doi: http://dx.doi.org/10.4314/jmbs.v6i2.3 ORIGINAL ARTICLE Trend of Suicide in Kermanshah during 11 years (2004 to 2014), Iran A.H. Hashemian 1,2, F. Najafi1, T.A. Jouybary3, and Z. Moradi Nazar 4 1Research Center for Environmental Determinants of Health (RCEDH), 2Department of Biostatistics, 4Department of Biostatistics and Epidemiology, School of Public Health, 3Clinical Research Development Center. Imam Khomeini Hospital, Kermanshah University of Medical Sciences, Kermanshah, Iran Suicide is one of the most important health problems which has dedicated a significant part of the energy and health care costs to itself. The present study carried out to investigate trend of suicide in Kermanshah province during 2004-2014. This is an analytical (cross sectional) study in which all cases died by suicide and documented in forensics of Kermanshah during 2004 – 2014 were investigated. For evaluating the trend for suicide, Poisson regression model was used and to calculate suicide rate, census data from 2006 and 2011 as well as Organization for Civil Registration were obtained. During the 11 years of study, 2799 people died in Kermanshah province by suicide; among which 1681 (60.1%) were men and 1118 (39.9%) were women. The average annual mortality rate was 15.77 per 100,000; that is, 12.81 women and 18.62 men per every 100,000 populations. The highest number of deaths caused by suicide was witnessed among the age group 20-24 by 24.91 per 100,000. -
Suicides and Self-Inflicted Injuries in Massachusetts: Data Update
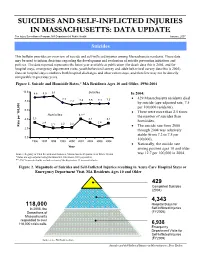
SSUUIICCIIDDEESS AANNDD SSEELLFF--IINNFFLLIICCTTEEDD IINNJJUURRIIEESS IINN MMAASSSSAACCHHUUSSEETTTTSS:: DDAATTAA UUPPDDAATTEE The Injury Surveillance Program, MA Department of Public Health January, 2007 Suicides This bulletin provides an overview of suicide and self-inflicted injuries among Massachusetts residents. These data may be used to inform decisions regarding the development and evaluation of suicide prevention initiatives and policies. The data reported represents the latest year available at publication (for death data this is 2004, and for hospital stays, emergency department visits, youth behavioral survey and adult behavioral survey data this is 2005). Data on hospital stays combines both hospital discharges and observation stays, and therefore may not be directly comparable to previous years. Figure 1. Suicide and Homicide Rates,* MA Residents Ages 10 and Older, 1996-2004 10.0 8.8 8.9 9.1 Suicides In 2004: 7.7 • 429 Massachusetts residents died 8.0 7.2 7.4 7.5 7.4 7.5 by suicide (age-adjusted rate, 7.5 per 100,000 residents). 6.0 • There were more than 2.5 times Homicides 4.1** the number of suicides than 4.0 3.3 3.2 3.1 2.4 2.4 homicides. 2.1 2.2 2.2 100,000 per Rate • The suicide rate from 2000 2.0 through 2004 was relatively stable (from 7.2 to 7.5 per 0.0 100,000). 1996 1997 1998 1999 2000 2001 2002 2003 2004 • Nationally, the suicide rate Year among persons ages 10 and older Source: Registry of Vital Records and Statistics, Massachusetts Department of Public Health was 12.7 per 100,000 in 2004. -

Age Differences in Suicide Methods
Forensic Research & Criminology International Journal Research Article Open Access Age differences in suicide methods Abstract Volume 6 Issue 6 - 2018 Objective: There is not adequate research on suicide methods by age in Turkey. The purpose of the present study is to investigate whether there is any change in suicide methods Mustafa Demir by age over time and whether suicide methods significantly differ by age. State University of New York at Plattsburgh, USA Method: Secondary data about suicide from 2007 to 2015 were obtained from the Turkish Correspondence: Mustafa Demir, State University of New Statistical Institute. The number of suicide cases was 25,696. Direct standardization method York at Plattsburgh, USA, Tel +15185643305, was used to calculate suicide rates. Line charts were plotted to reveal the trends in suicide Email methods by age. Then, one-way anova (ANOVA) test was conducted to test whether suicide methods significantly differed by age. Received: June 05, 2017 | Published: December 11, 2018 Results: Among all ages, hanging was the most common suicide method, followed by firearm, jumping, intoxication, and cutting/burning among all age groups. Moreover, all of the other suicide methods increased except for cutting/burning among those aged 15- 24 years, except for firearm among those aged 25-44 years, except for hanging among those aged 45-64 years. Among those aged 65 and older, suicide by hanging decreased, however, suicide by other methods overall remained stable. The results also showed that with increasing age, suicide by hanging, jumping, and cutting increased, while suicide by firearm and intoxication decreased. In addition, the results of ANOVA test indicated that except for intoxication, all other suicide methods differed significantly by age groups. -

Oregon Youth Suicide Prevention Guidelines
Photograph by Jason Dessel (1998) OORREEGGOONN YYOOUUTTHH SSUUIICCIIDDEE PPRREEVVEENNTTIIOONN YOUTH SUICIDE PREVENTION INTERVENTION & POSTVENTION GUIDELINES A Resource for School Personnel Developed by The Maine Youth Suicide Prevention Program A Program of Governor Angus S. King, Jr. And the Maine Children’s Cabinet May 2002 Modified for Oregon by Jill Hollingsworth, MA Looking Glass Youth and Family Services November 2007 (2nd revision) YOUTH SUICIDE PREVENTION, INTERVENTION & POSTVENTION GUIDELINES TABLE OF CONTENTS Page I. INTRODUCTION 1 II. RATIONALE FOR DEVELOPING AND IMPLEMENTING SUICIDE PREVENTION 4 AND INTERVENTION PROTOCOLS III. COMPONENTS OF SCHOOL-BASED SUICIDE PREVENTION 6 A. READINESS SURVEY FOR ADMINISTRATORS 9 IV. COMPONENTS OF SCHOOL- BASED SUICIDE INTERVENTION 13 A. ESTABLISHING SUICIDE PROTOCOLS WITHIN THE SCHOOL CRISIS 14 RESPONSE PLAN B. GUIDELINES FOR WHEN THE RISK OF SUICIDE HAS BEEN RAISED 14 C. GUIDELINES FOR MEDIUM TO HIGH RISK SITUATIONS 16 D. GUIDELINES FOR WHEN A SUICIDE INVOLVES A PACT 17 E. RESPONDING TO A STUDENT SUICIDE ATTEMPT ON SCHOOL PREMISES 18 F. GUIDELINES FOR A STUDENT SUICIDE ATTEMPT OFF SCHOOL PREMISES 19 G. GUIDELINES FOR WHEN A STUDENT RETURNS TO SCHOOL FOLLOWING 20 H. ABSENCE FOR SUICIDAL BEHAVIOR V. COMPONENTS OF SUICIDE POSTVENTION PLANNING 22 A. KEY CONSIDERATIONS 23 B. RESPONDING TO A SUICIDE 25 Appendix A – RESPONSE, a Comprehensive Suicide Awareness Program 32 Appendix B – Basic Suicide Prevention and Intervention Information 36 Appendix C – Short Version of Suicide Intervention and -

Homicide-Followed-By-Suicide Incidents Involving Child Victims
Homicide-Followed-by-Suicide Incidents Involving Child Victims Joseph E. Logan, PhD, MHS; Sabrina Walsh, DrPH; Nimeshkumar Patel, MA; Jeffrey E. Hall, PhD, MSPH Objectives: To describe homicide-fol- were parents/caregivers. Eighty-one per- lowed-by-suicide incidents involving cent of incidents with paternal perpetra- child victims Methods: Using 2003-2009 tors and 59% with maternal perpetrators National Violent Death Reporting Sys- were preceded by parental discord. Fifty- tem data, we characterized 129 incidents two percent of incidents with maternal based on victim and perpetrator demo- perpetrators were associated with mater- graphic information, their relationships, nal psychiatric problems. Conclusions: the weapons/mechanisms involved, and Strategies that resolve parental conflicts the perpetrators’ health and stress-re- rationally and facilitate detection and lated circumstances. Results: These in- treatment of parental mental conditions cidents accounted for 188 child deaths; might help prevention efforts. 69% were under 11 years old, and 58% Key words: homicide-suicide, children were killed with a firearm. Approximately Am J Health Behav. 2013;37(4):531-542 76% of perpetrators were males, and 75% DOI: http://dx.doi.org/10.5993/AJHB.37.4.11 omicide-followed-by-suicide (hereafter re- of homicide-suicide victims are children, stepchil- ferred to as “homicide-suicide”) incidents dren, or foster children of the perpetrator.1 This Hare defined as violent acts during which finding indicates that research is needed to iden- a person kills one or more individuals and then tify factors that might prevent this form of violence commits suicide.1-3 These incidents account for against children from occurring.