Inflammatory Skin Disease Every Pathologist Should Know
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Paraneoplastic Syndrome Presenting As Giant Porokeratosis in a Patient with Nasopharyngeal Cancer
Paraneoplastic Syndrome Presenting As Giant Porokeratosis in A Patient with Nasopharyngeal Cancer Fitri Azizah, Sonia Hanifati, Sri Adi Sularsito, Lili Legiawati, Shannaz Nadia Yusharyahya, Rahadi Rihatmadja Department of Dermatology and Venereology, Faculty of Medicine Universitas Indonesia / Dr. Cipto Mangunkusumo National General Hospital Keywords: porokeratosis, giant porokeratosis, paraneoplastic syndrome, nasopharyngeal Abstract: Giant porokeratosis is a rare condition in which the hyperkeratotic plaques of porokeratosis reach up to 20 cm in diameter. Porokeratosis is characterized clinically by hyperkeratotic papules or plaques with a thread-like elevated border. Although rare, porokeratosis has been reported in conjunction with malignancies suggesting a paraneoplastic nature. Associated malignancies reported were hematopoietic, hepatocellular, and cholangiocarcinoma. We report a case of giant porokeratosis in a patient with nasopharyngeal cancer responding to removal of the primary cancer by chemoradiotherapy. 1 INTRODUCTION regress completely after the treatment of malignancy, suggestive of paraneoplastic syndrome. Porokeratosis is a chronic progressive disorder of keratinization, characterized by hyperkeratotic papules or plaques surrounded by a thread-like 2 CASE elevated border corresponds to a typical histologic hallmark, the cornoid lamella . O regan, 2012) There Mr. SS, 68-year-old, was referred for evaluation of are at least six clinical variants of porokeratosis pruritic, slightly erythematous plaques with raised, recognized with known genetic disorder.1 Some hyperpigmented border of one and a half year clinical variant of porokeratosis has been reported in duration on the extensor surface of both legs. The the setting of immunosuppressive conditions, organ lesions shown minimal response to potent topical transplantation, use of systemic corticosteroids, and corticosteroids and phototherapy given during the infections, suggesting that impaired immunity may last 8 months in another hospital. -

ECZEMA) Shankar Pratap K
Research Article International Ayurvedi c Medical Journal ISSN:2320 5091 A HISTOPATHOLOGICAL STUDY ON LEECH APPLICATION IN THE MANAGEMENT OF VICARCIKA (ECZEMA) Shankar Pratap K. M.1 Rao Dattatreya 2 Sai Prasad 3 1Dept. of Shalya Tantra , Santhigiri Ayurvedic College , Palakkad, Kerala, India 2Dept. of Shalya Tantra, S.V. Ayurvedic College, Tirupati , Andhra Pradesh , India 3Dept. of Pathology, S. V. Medical College, Tirupati, Andhra Pradesh, India ABSTRACT To assess the efficacy of Leech application in the management of Vicarcik a (Eczema) with Histopathological study, the present study with 10 patients having the classical symptoms of Vicarcika, were randomly selected as per the inclusion and exclusion criteria from O.P.D. & I.P.D. sections of Shalya department, S.V. Ayurvedic Hospital, Tirupati. Minimum 4 sittings of Leech application was carried out with seven days interval. Total duration of treatment was 6 weeks. Biopsy samples were collected from the lesion site before and after treatment. Histopathological examination was done by the pathologist. In eczema (dermatitis) the leech application therapy gives excellent response by reducing the inflammatory component, hyperkeratosis, spongiosis, irregular acanthosis and by evoking a granulation tissue response in the dermis and in most of the cases with complete recovery from the lesion. Most of the cases in the study were chronic dermatitis and sebhoric keratosis, almost all local/focal pigmented lesion is totally relieved by leech therapy especially in cases of sebhoric keratos is. In the present study it was found that, leech application evokes significant changes at histological level specifically in reduction of inflammatory component, hyperkeratosis, spongiosis and irregular acanthosis. -
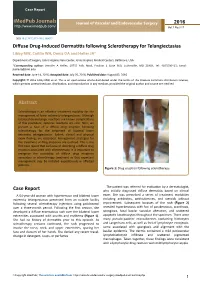
Diffuse Drug-Induced Dermatitis Following Sclerotherapy for Telangiectasias Libby MW, Caitlin WH, Deniz OA and Heller JA*
Case Report iMedPub Journals Journal of Vascular and Endovascular Surgery 2016 http://www.imedpub.com/ Vol.1 No.3:17 DOI: 10.21767/2573-4482.100017 Diffuse Drug-Induced Dermatitis following Sclerotherapy for Telangiectasias Libby MW, Caitlin WH, Deniz OA and Heller JA* Department of Surgery, Johns Hopkins Vein Center, Johns Hopkins Medical Centers, Baltimore, USA *Corresponding author: Jennifer A Heller, 10755 Falls Road, Pavilion 1 Suite 360, Lutherville, MD 21903, Tel: 4105500415; Email: [email protected] Received date: June 14, 2016; Accepted date: July 26, 2016; Published date: August 02, 2016 Copyright: © 2016 Libby MW, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Sclerotherapy is an effective treatment modality for the management of lower extremity telangiectasias. Although localized dermatologic reactions are known complications of this procedure, systemic reactions are rare. Here, we present a case of a diffuse drug eruption following sclerotherapy for the treatment of bilateral lower extremity telangiectasias. Salient clinical and physical exam findings are described. Management strategies for the treatment of drug eruptions are outlined. This is the first case report that we know of describing a diffuse drug eruption associated with sclerotherapy. It is important to recognize the possibility of diffuse drug eruptions secondary to sclerotherapy treatment so that expectant management may be initiated expeditiously in affected patients. Figure 1: Drug eruption following sclerotherapy. The patient was referred for evaluation by a dermatologist, Case Report who initially diagnosed diffuse dermatitis based on clinical A 64-year-old woman with hypertension and bilateral lower exam. -

JMSCR Vol||07||Issue||03||Page 281-286||March 2019
JMSCR Vol||07||Issue||03||Page 281-286||March 2019 www.jmscr.igmpublication.org Index Copernicus Value: 79.54 ISSN (e)-2347-176x ISSN (p) 2455-0450 DOI: https://dx.doi.org/10.18535/jmscr/v7i3.51 Histopathological Evaluation of Collagen Profiles in Spongiotic Dermatitis Authors Anjali Patankar, Ramya Gandhi*, Erli Amel Ivan Department of Pathology, Sri Manakula Vinayagar Medical College and Hospital, Kalitheerthalkuppam, Puducherry, 605 107 India *Corresponding Author Dr Ramya Gandhi Associate Professor, Department of Pathology, Sri Manakula Vinayagar Medical College and Hospital, Kalitheerthalkuppam, Puducherry, 605 107, India Email: [email protected], Mobile no- 9787740891 Abstract Context: Spongiotic Dermatitis is a common clinical condition also known as eczema, characterized by rashes and itching further may progress to scarring. The terms eczema and dermatitis are often used interchangeably to denote a polymorphic inflammatory reaction pattern involving the epidermis and dermis. Spongiosis refers to intraepidermal edema. Aim: To assess the orientation of collagen in eczematous spongiotic dermatitis. Material and Methods: The present study was done in the Department of Pathology, Sri Manakula Vinayagar Medical College, Pondicherry. Sixty diagnosed cases of spongiotic dermatitis diagnosed over a period of five years were taken in the study. Orientation of collagen was evaluated using Masson’s trichrome stain. Results: Spongiotic dermatitis occurred in all age groups but commonly seen in middle age to elderly. Male to female ratio was 1:1.2 The most common symptom was itching (85%) followed by scaling (63.3%). Most common site was upper extremities (80%). subacute cases were predominantly seen (38.3%) followed by chronic cases (33.3%). -

Pemphigus and Other Bullous Dermatoses: Correlation of Clinical and Pathologic Findings
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector PEMPHIG[JS AND OTHER BULLOUS DERMATOSES: CORRELATION OF CLINICAL AND PATHOLOGIC FINDINGS" JOSEPH G. BRENNAN, M.D.t AND HAMILTON MONTGOMERY, M.D4 A detailed clinical and histopathologic study has been made of patients who had pemphigus of various types and of patients who had other bullous derma- toses; this study includes follow-up information covering a period of years. The lesions in some of these patients have had to he reclassified on the basis of newer histologic concepts of pemphigus, namely the phenomenon of acantholysis, which is seen in pemphigus and not in other bullous dermatoses, except for those caused by viral diseases. By acantholysis is meant loss of prickles of the prickle cells in the epidermis, with lysis of the individual cell. This phenomenon, occurring as a primary change in pemphigus in distinction from pressure or tension phenomena, which are the primary changes in other bullous dermatoses (except for pemphi- gus and viral diseases), is considered in another article by one of us (Brennan, 1). Differentiation of bullous dermatoses was accepted clinically prior to 1848, when Simon (2) considered that the bulla of pemphigus could be differentiated histologically because it was subepidermal and because the hair follicle was torn off. Haight (3), in 1868, thought the bulla of pemphigus was under the stratum corneum and was characterized by fissures formed by long, drawn-out prickle cells. Auspitz (4), in 1881, classified bullous dermatoses accord- ing to their histology and was the first to describe acantholysis. -

2. Studies of Cancer in Humans
P_179_278.qxp 30/11/2007 09:40 Page 179 HUMAN PAPILLOMAVIRUSES 179 2. Studies of Cancer in Humans 2.1 Methodological concerns (a) Choice of disease end-point To obtain epidemiological evidence of the risk for cervical cancer due to a specific type of human papillomavirus (HPV), the choice of disease end-point must be appro- priate. The risk for invasive cancer is examined optimally by a case–control design or among historical cohorts in which archived specimens are tested. Prospective studies that follow women forward in time must ethically rely on surro- gate end-points, the choice of which is critical. For studies of HPV infection, invasive cancer and grade 3 cervical intraepithelial neoplasia (CIN3; which subsumes diagnoses of severe dysplasia and carcinoma in situ) are considered to be the primary disease end- points. The inclusion of CIN3 as a surrogate for invasive cancer permits prospective studies that would otherwise be unethical, because it is a condition that often requires medical treatment, whith thus interrupts the natural history of the disease. CIN3 is the immediate precursor of invasive cervical cancer, and the two diseases share a similar P_179_278.qxp 30/11/2007 09:40 Page 180 180 IARC MONOGRAPHS VOLUME 90 cross-sectional virological and epidemiological profile (except for an earlier average age at diagnosis of CIN3) and demonstrate good histopathological reproducibility (Shah et al., 1980; Walker et al., 1983; Muñoz et al., 1992, 1993). Therefore, CIN3 is a practical surro- gate end-point for cervical cancer, although a proportion of cases of CIN3 regress rather than invade. However, in cohort studies, new diagnoses of small CIN3 lesions may repre- sent diseases that were missed at the time of enrolment when HPV was assayed. -

Review of the Literature
Review Clinical and Histopathological Features and Potential Pathological Mechanisms of Skin Lesions in COVID-19: Review of the Literature Gürkan Kaya 1,*, Aysin Kaya 2 and Jean-Hilaire Saurat 2 1 Departments of Dermatology and Clinical Pathology, University Hospital of Geneva, 1205 Geneva, Switzerland 2 Department of Clinical Pharmacology and Toxicology, University of Geneva, 1205 Geneva, Switzerland; [email protected] (A.K.); [email protected] (J.-H.S.) * Correspondence: [email protected] Received: 24 June 2020; Accepted: 29 June 2020; Published: 30 June 2020 Abstract: In recent weeks, several reports have emerged of skin lesions with different clinical presentations in COVID-19 cases. All dermatologists should be aware of these cutaneous lesions, which may be early clinical symptoms of infection. We reviewed the literature on cutaneous manifestations in the PubMed database from December 2019 and June 2020. From the cases described as case reports or series in 57 recent articles, it appears that skin lesions (i) are highly varied, (ii) may not be related to the severity of the condition and (iii) resolve spontaneously in a few days. The frequency of these lesions in COVID-19 patients varies between 1.8% and 20.4%. The major clinical forms described were maculopapular eruptions, acral areas of erythema with vesicles or pustules (pseudochilblain), urticarial lesions, other vesicular eruptions and livedo or necrosis. The lesions were mainly localized in the trunk and extremities. The majority of patients were male, aged between 4.5 and 89 years. A minority of the patients were children presenting with acral, chilblain-like lesions, papulo-vesicular eruptions or Kawasaki disease-like pediatric inflammatory multisystem syndrome. -

Fig. 1. Lentigo Simplex. Elongated Rete Ridges, Hyperpigmentation of The
97 Fig. 1. Lentigo simplex. Elongated rete ridges, hyperpigmentation of the basal layer and increase in number of enlarged melanocytes arranged singly along the basal layer Fig. 2. Junctional melanocytic naevus. Nests of melanocytes are present at the dermo-epidermal junction, predominantly at the bases of elongated rete ridges 98 a b Fig.3a,b. Compound melanocytic naevus. a Nests of melanocytes in the dermis as well as the derma-epidermal junction, smaller and more diffusely arranged in the deeper dermis. b The nests of melanocytes include multinucleated giant cells 99 Fig. 4. Dermal melanocytic naevus. Entirely intradermal tumour in a nested pattern in the superficial layers, composed of small naevoid melanocytes in the deep dermis Fig. 5. Dermal melanocytic naevus. The deeper layers of this dermal melanocytic naevus include neuroid structures similar to Wagner-Meissner corpuscles (neuroid dermal melanocytic naevus) 100 Fig. 6. Balloon cell naevus. The tumour is composed mainly of melanocytes with abundant clear cytoplasm and central nuclei Fig. 7. Halo naevus. Compound naevus with a dense lymphocytic infiltrate between the naevoid melanocytes of the dermal component Fig. 8. Combined intradermal naevus and blue naevus. Nests of epithelioid naevus cells in the dermis (right) and heavily pigmented spindle and dendritic cells arranged between collagen bundles in the adjacent stroma (left) Fig. 9a. Deep penetrating naevus. A wedge-shaped lesion composed of irregu lar collections of variably pigmented cells extending into the deep dermis. 102 Fig. 9b. Deep penetrating naevus. In the deep dermis the lesion includes large cells with nuclear pseudo-inclusions, smaller naevoid melanocytes and groups of melanophages in the intervening stroma Fig. -

Pigmented Actinic Keratosis: Case Report and Review of an Uncommon Actinic Keratosis Variant That Can Mimic Melanoma
Open Access Case Report DOI: 10.7759/cureus.4721 Pigmented Actinic Keratosis: Case Report and Review of an Uncommon Actinic Keratosis Variant that can Mimic Melanoma Boya Abudu 1 , Antoanella Calame 2 , Philip R. Cohen 3 1. Internal Medicine, Kaiser Permanente Oakland Medical Center, Oakland, USA 2. Dermatology, Compass Dermatopathology, Inc., San Diego, USA 3. Dermatology, San Diego Family Dermatology, National City, USA Corresponding author: Boya Abudu, [email protected] Abstract Pigmented actinic keratosis is an uncommon variant of actinic keratosis that can mimic melanocytic lesions. A 54-year-old man who presented with a dark lesion on his nasal tip is described; biopsy of the lesion revealed a pigmented actinic keratosis that was treated with cryotherapy using liquid nitrogen. Pigmented actinic keratoses typically appear on sun-exposed areas of the skin as flat hyperpigmented lesions that grow in a centrifugal pattern. Dermoscopy reveals one or more pseudonetworks with hyperpigmented dots or globules. Histopathology shows atypical keratinocytes in the epidermal basal layer and increased melanin content in the epidermis and dermis. Treatment options include liquid nitrogen cryotherapy for solitary lesions and curettage, 5-fluorouracil, imiquimod, ingenol mebutate, photodynamic therapy, or superficial peels for extensive lesions. Categories: Dermatology, Pathology Keywords: actinic, immunoperoxidase, keratosis, lentigo, maligna, malignant, melanoma, pigmented, solar, spreading Introduction Pigmented actinic keratosis is an uncommon clinical variant of actinic keratosis [1-18]. This precancerous lesion can mimic not only melanocytic lesions but also other epithelial tumors [7-8,16-18]. The clinical and pathologic features of an actinic keratosis on the nasal tip of a man are described and the characteristics of this unique lesion are reviewed. -

The Best Diagnosis Is: A
DERMATOPATHOLOGY DIAGNOSIS H&E, original magnification ×40. The best diagnosis is: a. lichen striatus copy b. linear epidermolytic hyperkeratosis c. linear lichen planus d. linear porokeratosisnot e. linear psoriasis Do A H&E, original magnification ×CUTIS40. B H&E, original magnification ×200 for both. PLEASE TURN TO PAGE 120 FOR DERMATOPATHOLOGY DIAGNOSIS DISCUSSION Jacqueline N. Graham, BS; Eric W. Hossler, MD Ms. Graham is from Northeast Ohio Medical University, Rootstown. Dr. Hossler is from the Departments of Dermatology and Pathology, Geisinger Medical Center, Danville, Pennsylvania. The authors report no conflict of interest. Correspondence: Jacqueline N. Graham, BS, 4249 Pine Dr, Rootstown, OH 44272 ([email protected]). 86 CUTIS® WWW.CUTIS.COM Copyright Cutis 2015. No part of this publication may be reproduced, stored, or transmitted without the prior written permission of the Publisher. Dermatopathology Diagnosis Discussion Lichen Striatus ichen striatus (LS) is a benign, uncommon, self-limited, linear inflammatory skin disorder Lthat primarily affects children up to 15 years of age, most commonly around 2 to 3 years of age, and is seen more frequently in girls.1 It presents with a sudden eruption of asymptomatic small, flat- topped, lichenoid, scaly papules in a linear array on a single extremity. The lesions may be erythematous, flesh colored, or hypopigmented.1,2 Multiple lesions appear over days to weeks and coalesce into linear plaques in a continuous or interrupted pattern along the lines of Blaschko, indicating possible -

WSC 14-15 Conf 7 Layout
Joint Pathology Center Veterinary Pathology Services WEDNESDAY SLIDE CONFERENCE 2014-2015 Conference 7 22 October 2014 CASE I: B13-962 (JPC 4049563). performed at that time. The dog presented again in July 2013 with continued hematuria. On Signalment: 10-year-old spayed female Welsh ultrasound, the left renal cortex had a 2.2 cm, corgi dog, Canis familiaris. round, heterogeneous mass with multiple, internal, anechoic regions. History: The dog presented in 2011 for a 6-week history of hematuria. Urine culture was negative Gross Pathology: The renal cortex was and no signs of uroliths were seen on radiographs. extensively disrupted by coalescing, dark red, Ultrasound revealed two, 1.7 mm, mineralized blood-filled nodules ranging from 0.7 x 0.5 x 0.2 foci in the left renal pelvis, but the kidneys were cm to 2.5 x 2 x 2 cm. normal in shape and size. No further workup was Histopathologic Description: Kidney: The renal interstitium is markedly expanded by many, severely dilated, blood-filled vascular spaces lined by mature endothelial cells surrounded by abundant fibrous tissue. Some vascular spaces contain thrombi with fibrin arranged as lines of Zahn separated by red and white blood cells that are occasionally attached to the vascular wall by fibrous tissue. The intervening and adjacent renal parenchyma is markedly atrophic with replacement of many nephrons by fibrosis, many lymphocytes and plasma cells, and variable 1-1. Kidney, Welsh corgi: The cortex is expanded by large, ectatic, thin-walled vessels which efface renal parenchyma. (HE 6.3X) hemorrhage. Remaining tubules 1 WSC 2014-2015 1-2. -

Plasma Cell Gingivitis
Plasma Cell Gingivitis C. Román Curto, MD; M. Yuste Chaves, MD; A. González Morán, MD; P. González Asensio, MD; G. López, MD Plasma cell gingivitis (PCG), an infrequent benign inflammatory condition of unknown etiology, is a type of plasma cell orificial mucositis, which includes a wide spectrum of conditions. We pre- sent the case of a 13-year-old girl who had PCG with an erythematous congestive plaque on the anterior maxillary gingiva for 4 years. Occasion- ally, the lesion became increasingly swollen and painful and bled. Results of a histopathologic examination showed dense plasmacytic infiltrate in the dermis, affecting the dermoepidermal bor- der, with immunohistochemical positivity in the and light chains and vascular proliferation. “Lozenge” keratinocytes, “watery” spongiosis, and exocytosis were seen in the epidermis. Figure 1. A bright red, slightly elevated plaque on the Laboratory analysis showed notably low levels of upper gum with a fine, whitish, superficial network. both serum IgA and secretory IgA. We consider whether secretory IgA at low levels has an impor- tant etiopathogenic role favoring the develop- Case Report ment of localized subclinical repetitive infections A 13-year-old girl without significant pathologic or that could lead to chronic PCG. dental history (other than the habit of chewing gum 2 or 3 times a week) had a bright red, congestive, lasma cell gingivitis (PCG) is a benign inflam- asymptomatic plaque on her upper gum for 4 years. matory condition that is uncommon (at least Occasionally and without any clear association with P in the dermatologic literature) and of unclear the girl’s menstrual cycle, the lesion became increas- etiology.