Views from the Citizen Health Information Portal: Qualitative Study (E43) Tracie Risling, Juan Martinez, Jeremy Young, Nancy Thorp-Froslie
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(Gastropoda: Cocculiniformia) from Off the Caribbean Coast of Colombia
ó^S PROCEEDINGS OF THE BIOLOGICAL SOCIETY OF WASHINGTON ll8(2):344-366. 2005. Cocculinid and pseudococculinid limpets (Gastropoda: Cocculiniformia) from off the Caribbean coast of Colombia Néstor E. Ardila and M. G. Harasewych (NEA) Museo de Historia Natural Marina de Colombia, Instituto de Investigaciones Marinas, INVEMAR, Santa Marta, A.A. 1016, Colombia, e-mail: [email protected]; (MGH) Department of Invertebrate Zoology, MRC-I63, National Museum of Natural History, Smithsonian Institution, Washington, D.C. 20013-7012 U.S.A., e-mail: [email protected] Abstract.•The present paper reports on the occurrence of six species of Cocculinidae and three species of Pseudococculinidae off the Caribbean coast of Colombia. Cocculina messingi McLean & Harasewych, 1995, Cocculina emsoni McLean & Harasewych, 1995 Notocrater houbricki McLean & Hara- sewych, 1995 and Notocrater youngi McLean & Harasewych, 1995 were not previously known to occur within the of the Caribbean Sea, while Fedikovella beanii (Dall, 1882) had been reported only from the western margins of the Atlantic Ocean, including the lesser Antilles. New data are presented on the external anatomy and radular morphology of Coccocrater portoricensis (Dall & Simpson, 1901) that supports its placement in the genus Coccocrater. Coc- culina fenestrata n. sp. (Cocculinidae) and Copulabyssia Colombia n. sp. (Pseu- dococculinidae) are described from the upper continental slope of Caribbean Colombia. Cocculiniform limpets comprise two paraphyletic, with the Cocculinoidea related groups of bathyal to hadal gastropods with to Neomphalina and the Lepetelloidea in- global distribution that live primarily on cluded within Vetigastropoda (Ponder & biogenic substrates (e.g., wood, algal hold- Lindberg 1996, 1997; McArthur & Hara- fasts, whale bone, cephalopod beaks, crab sewych 2003). -

Contributions in Science
NUMBER 453 9 JUNE 1995 CONTRIBUTIONS IN SCIENCE REVIEW OF WESTERN ATLANTIC SPECIES OF COCCULINID AND PSEUDOCOCCULINID LIMPETS, WITH DESCRIPTIONS OF NEW SPECIES (GASTROPODA: COCCULINIFORMIA) JAMES H. MCLEAN AND M. G. HARASEWYCH NATURAL HISTORY MUSEUM OF LOS ANGELES GOUNTY Thf: scientific publications of the Natural History Mu- SERIAL seum of Los Angeles County have been issued at irregular intervals in three major series; the issues in each series are PUBLICATIONS numbered individually, and numbers run consecutively, OF THE regardless of the subject matter. • Contributions in Science, a miscellaneous series of tech- NATURAL HISTORY nical papers describing original research in the life and earth sciences. MUSEUM OF • Science Bulletin, a miscellaneous series of monographs describing original research in the hfe and earth sci- LOS ANGELES ences. This series was discontinued in 1978 with the issue of Numbers 29 and 30; monographs are now COUNTY published by the Museum in Contributions in Science. • Science Series, long anieles and collections of papers on natural history topics. Copies of the publications in these series are sold through the Museum Book Shop. A catalog is available on request. The Museum also publishes Technical Reports, a mis- cellaneous series containing information relative to schol- arly inquiry and collections but not reporting the results of original research. Issue is authorized by the Museum's Scientific Publications Committee; however, manuscripts do not receive anonymous peer review. Individual Tech- nical Reports may be obtained from the relevant Section of the Museum. SCIENTIFIC PUBLICATIONS COMMITTEE «ÎWA James L. Powell, Museum President NATURAL HISTORY MUSEUM Daniel M. Cohen, Committee OF Los ANGELES COUNTY Chairman 900 EXPOSITION BOULEVARD Brian V. -

Shell Microstructures in Early Cambrian Molluscs
Shell microstructures in Early Cambrian molluscs ARTEM KOUCHINSKY Kouchinsky, A. 2000. Shell microstructures in Early Cambrian molluscs. - Acta Palaeontologica Polonica 45,2, 119-150. The affinities of a considerable part of the earliest skeletal fossils are problematical, but investigation of their microstructures may be useful for understanding biomineralization mechanisms in early metazoans and helpful for their taxonomy. The skeletons of Early Cambrian mollusc-like organisms increased by marginal secretion of new growth lamel- lae or sclerites, the recognized basal elements of which were fibers of apparently aragon- ite. The juvenile part of some composite shells consisted of needle-like sclerites; the adult part was built of hollow leaf-like sclerites. A layer of mineralized prism-like units (low aragonitic prisms or flattened spherulites) surrounded by an organic matrix possibly existed in most of the shells with continuous walls. The distribution of initial points of the prism-like units on a periostracurn-like sheet and their growth rate were mostly regular. The units may be replicated on the surface of internal molds as shallow concave poly- gons, which may contain a more or less well-expressed tubercle in their center. Tubercles are often not enclosed in concave polygons and may co-occur with other types of tex- tures. Convex polygons seem to have resulted from decalcification of prism-like units. They do not co-occur with tubercles. The latter are interpreted as casts of pore channels in the wall possibly playing a role in biomineralization or pits serving as attachment sites of groups of mantle cells. Casts of fibers and/or lamellar units may overlap a polygonal tex- ture or occur without it. -

Mollusca, Archaeogastropoda) from the Northeastern Pacific
Zoologica Scripta, Vol. 25, No. 1, pp. 35-49, 1996 Pergamon Elsevier Science Ltd © 1996 The Norwegian Academy of Science and Letters Printed in Great Britain. All rights reserved 0300-3256(95)00015-1 0300-3256/96 $ 15.00 + 0.00 Anatomy and systematics of bathyphytophilid limpets (Mollusca, Archaeogastropoda) from the northeastern Pacific GERHARD HASZPRUNAR and JAMES H. McLEAN Accepted 28 September 1995 Haszprunar, G. & McLean, J. H. 1995. Anatomy and systematics of bathyphytophilid limpets (Mollusca, Archaeogastropoda) from the northeastern Pacific.—Zool. Scr. 25: 35^9. Bathyphytophilus diegensis sp. n. is described on basis of shell and radula characters. The radula of another species of Bathyphytophilus is illustrated, but the species is not described since the shell is unknown. Both species feed on detached blades of the surfgrass Phyllospadix carried by turbidity currents into continental slope depths in the San Diego Trough. The anatomy of B. diegensis was investigated by means of semithin serial sectioning and graphic reconstruction. The shell is limpet like; the protoconch resembles that of pseudococculinids and other lepetelloids. The radula is a distinctive, highly modified rhipidoglossate type with close similarities to the lepetellid radula. The anatomy falls well into the lepetelloid bauplan and is in general similar to that of Pseudococculini- dae and Pyropeltidae. Apomorphic features are the presence of gill-leaflets at both sides of the pallial roof (shared with certain pseudococculinids), the lack of jaws, and in particular many enigmatic pouches (bacterial chambers?) which open into the posterior oesophagus. Autapomor- phic characters of shell, radula and anatomy confirm the placement of Bathyphytophilus (with Aenigmabonus) in a distinct family, Bathyphytophilidae Moskalev, 1978. -

Keeping a Lid on It: Muscle Scars and the Mystery of the Mobergellidae
1 Keeping a lid on it: muscle scars and the mystery of the 2 Mobergellidae 3 4 TIMOTHY P. TOPPER1,2* and CHRISTIAN B. SKOVSTED1 5 6 1Department of Palaeobiology, Swedish Museum of Natural History, P.O. Box 50007, 7 SE-104 05, Stockholm, Sweden. 8 2Palaeoecosystems Group, Department of Earth Sciences, Durham University, Durham 9 DH1 3LE, UK. 10 11 Mobergellans were one of the first Cambrian skeletal groups to be recognized yet have 12 long remained one of the most problematic in terms of biological function and affinity. 13 Typified by a disc-shaped, phosphatic sclerite the most distinctive character of the 14 group is a prominent set of internal scars, interpreted as representing sites of former 15 muscle attachment. Predominantly based on muscle scar distribution, mobergellans 16 have been compared to brachiopods, bivalves and monoplacophorans, however a 17 recurring theory that the sclerites acted as operculum remains untested. Rather than 18 correlate the number of muscle scars between taxa, here we focus on the percentage of 19 the inner surface shell area that the scars constitute. We investigate two mobergellan 20 species, Mobergella holsti and Discinella micans comparing the Cambrian taxa with the 21 muscle scars of a variety of extant and fossil marine invertebrate taxa to test if the 22 mobergellan muscle attachment area is compatible with an interpretation as operculum. 23 The only skeletal elements in our study with a comparable muscle attachment 24 percentage are gastropod opercula. Complemented with additional morphological 25 information, our analysis supports the theory that mobergellan sclerites acted as an 26 operculum presumably from a tube-living organism. -
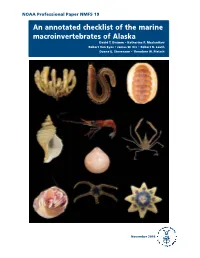
An Annotated Checklist of the Marine Macroinvertebrates of Alaska David T
NOAA Professional Paper NMFS 19 An annotated checklist of the marine macroinvertebrates of Alaska David T. Drumm • Katherine P. Maslenikov Robert Van Syoc • James W. Orr • Robert R. Lauth Duane E. Stevenson • Theodore W. Pietsch November 2016 U.S. Department of Commerce NOAA Professional Penny Pritzker Secretary of Commerce National Oceanic Papers NMFS and Atmospheric Administration Kathryn D. Sullivan Scientific Editor* Administrator Richard Langton National Marine National Marine Fisheries Service Fisheries Service Northeast Fisheries Science Center Maine Field Station Eileen Sobeck 17 Godfrey Drive, Suite 1 Assistant Administrator Orono, Maine 04473 for Fisheries Associate Editor Kathryn Dennis National Marine Fisheries Service Office of Science and Technology Economics and Social Analysis Division 1845 Wasp Blvd., Bldg. 178 Honolulu, Hawaii 96818 Managing Editor Shelley Arenas National Marine Fisheries Service Scientific Publications Office 7600 Sand Point Way NE Seattle, Washington 98115 Editorial Committee Ann C. Matarese National Marine Fisheries Service James W. Orr National Marine Fisheries Service The NOAA Professional Paper NMFS (ISSN 1931-4590) series is pub- lished by the Scientific Publications Of- *Bruce Mundy (PIFSC) was Scientific Editor during the fice, National Marine Fisheries Service, scientific editing and preparation of this report. NOAA, 7600 Sand Point Way NE, Seattle, WA 98115. The Secretary of Commerce has The NOAA Professional Paper NMFS series carries peer-reviewed, lengthy original determined that the publication of research reports, taxonomic keys, species synopses, flora and fauna studies, and data- this series is necessary in the transac- intensive reports on investigations in fishery science, engineering, and economics. tion of the public business required by law of this Department. -

Deep-Sea Video Technology Tracks a Monoplacophoran to the End of Its Trail (Mollusca, Tryblidia)
Deep-sea video technology tracks a monoplacophoran to the end of its trail (Mollusca, Tryblidia) Sigwart, J. D., Wicksten, M. K., Jackson, M. G., & Herrera, S. (2018). Deep-sea video technology tracks a monoplacophoran to the end of its trail (Mollusca, Tryblidia). Marine Biodiversity, 1-8. https://doi.org/10.1007/s12526-018-0860-2 Published in: Marine Biodiversity Document Version: Publisher's PDF, also known as Version of record Queen's University Belfast - Research Portal: Link to publication record in Queen's University Belfast Research Portal Publisher rights Copyright 2018 the authors. This is an open access article published under a Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution and reproduction in any medium, provided the author and source are cited. General rights Copyright for the publications made accessible via the Queen's University Belfast Research Portal is retained by the author(s) and / or other copyright owners and it is a condition of accessing these publications that users recognise and abide by the legal requirements associated with these rights. Take down policy The Research Portal is Queen's institutional repository that provides access to Queen's research output. Every effort has been made to ensure that content in the Research Portal does not infringe any person's rights, or applicable UK laws. If you discover content in the Research Portal that you believe breaches copyright or violates any law, please contact [email protected]. Download date:06. Oct. 2021 Deep-sea video technology tracks a monoplacophoran to the end of its trail (Mollusca, Tryblidia) Sigwart, J. -

(Gastropoda) with a Rhipidoglossate Radula
Org Divers Evol (2011) 11:201–236 DOI 10.1007/s13127-011-0048-0 ORIGINAL ARTICLE Interactive 3D anatomy and affinities of the Hyalogyrinidae, basal Heterobranchia (Gastropoda) with a rhipidoglossate radula Gerhard Haszprunar & Erika Speimann & Andreas Hawe & Martin Heß Received: 25 January 2011 /Accepted: 26 May 2011 /Published online: 19 June 2011 # Gesellschaft für Biologische Systematik 2011 Abstract Whereas Hyalogyrina Marshall, 1988 was already on the rhipidoglossate, i.e. the ‘archaeogastropod’, originally considered a skeneid vetigastropod, the family level of evolution. Ectobranchia are considered the first Hyalogyrinidae Warén & Bouchet, 1993 has later been extant offshoot of the Heterobranchia; implications for the classified as basal Heterobranchia despite their rhipidoglossate stem species of the latter are outlined. radula. In order to evaluate this placement and to shed more light on the origin of all higher Gastropoda, we investigated Keywords Gastropoda . Ectobranchia . Hyalogyrinidae . five representatives of all three nominal hyalogyrinid genera Interactive 3D anatomy. Systematics . Phylogeny. by means of semithin serial sectioning and computer-aided Heterobranchia 3D reconstruction of the respective anatomy, which we present in an interactive way. In general the morphological features (shell, external morphology, anatomy) fully confirm Introduction the placement of Hyalogyrinidae in the Heterobranchia, but in particular the conditions of the genital system vary During the last 25 years major progress has been made in substantially within the family. The ectobranch gill of our understanding of the origin of the higher gastropods, Hyalogyrinidae is shared with Valvatidae, Cornirostridae, i.e. the allogastropod, opisthobranch and pulmonate taxa, the and Xylodisculidae; consequently all these families are latter two of which are commonly united as Euthyneura. -

The Continuing Debate on Deep Molluscan Phylogeny: Evidence for Serialia (Mollusca, Monoplacophora + Polyplacophora)
Hindawi Publishing Corporation BioMed Research International Volume 2013, Article ID 407072, 18 pages http://dx.doi.org/10.1155/2013/407072 Research Article The Continuing Debate on Deep Molluscan Phylogeny: Evidence for Serialia (Mollusca, Monoplacophora + Polyplacophora) I. Stöger,1,2 J. D. Sigwart,3 Y. Kano,4 T. Knebelsberger,5 B. A. Marshall,6 E. Schwabe,1,2 and M. Schrödl1,2 1 SNSB-Bavarian State Collection of Zoology, Munchhausenstraße¨ 21, 81247 Munich, Germany 2 Faculty of Biology, Department II, Ludwig-Maximilians-Universitat¨ Munchen,¨ Großhaderner Straße 2-4, 82152 Planegg-Martinsried, Germany 3 Queen’s University Belfast, School of Biological Sciences, Marine Laboratory, 12-13 The Strand, Portaferry BT22 1PF, UK 4 Department of Marine Ecosystems Dynamics, Atmosphere and Ocean Research Institute, University of Tokyo, 5-1-5 Kashiwanoha, Kashiwa, Chiba 277-8564, Japan 5 Senckenberg Research Institute, German Centre for Marine Biodiversity Research (DZMB), Sudstrand¨ 44, 26382 Wilhelmshaven, Germany 6 Museum of New Zealand Te Papa Tongarewa, P.O. Box 467, Wellington, New Zealand Correspondence should be addressed to M. Schrodl;¨ [email protected] Received 1 March 2013; Revised 8 August 2013; Accepted 23 August 2013 Academic Editor: Dietmar Quandt Copyright © 2013 I. Stoger¨ et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Molluscs are a diverse animal phylum with a formidable fossil record. Although there is little doubt about the monophyly of the eight extant classes, relationships between these groups are controversial. We analysed a comprehensive multilocus molecular data set for molluscs, the first to include multiple species from all classes, including five monoplacophorans in both extant families. -

Jahresbericht 2010 Der Generaldirektion Der Staatlichen Naturwissenschaftlichen Sammlungen Bayerns Herausgegeben Von: Prof
Jahresbericht 2010 der Generaldirektion der Staatlichen Naturwissenschaftlichen Sammlungen Bayerns Herausgegeben von: Prof. Dr. Gerhard Haszprunar, Generaldirektor Generaldirektion der Staatlichen Naturwissenschaftlichen Sammlungen Bayerns (SNSB) Menzinger Straße 71, 80638 München München November 2010 Zusammenstellung und Endredaktion: Dr. Eva Maria Natzer (Generaldirektion) Unterstützung durch: Maria-Luise Kaim (Generaldirektion) Iris Krumböck (Generaldirektion) Susanne Legat (Generaldirektion) Druck: Digitaldruckzentrum, Amalienstrasse, München Inhaltsverzeichnis Bericht des Generaldirektors ...................................................................................................5 Wissenschaftliche Publikationen ................................................................................................6 Drittmittelübersicht ...................................................................................................................37 Organigramm ............................................................................................................................49 Generaldirektion .....................................................................................................................50 Personalvertretung ....................................................................................................................52 Museen Museum Mensch und Natur (MMN) ........................................................................................53 Museum Reich der Kristalle (MRK) ........................................................................................59 -

Coccopigya Viminensis (Rocchini, 1990)
Allegato alla pubblicazione “CatalogoAnnotato Atlante e iconogr Vers.1.0 Coccopigya viminensis (Rocchini, 1990) Scheda tassonomica: Classis Gastropoda Cuvier, 1797 Ordo Archaeogastropoda Thiele, 1925 Superfamilia Cocculinoidea Dall, 1882 Familia Cocculinidae Dall, 1882 Subfamilia Genus Coccopigya Marshall B.A., 1986 Subgenus afico deiafico molluschi marini del specie viminensis (Rocchini, 1990) [Cocculina] subspecie Scheda descrittiva: Sinonimi Descrizione Conchiglia capuliforme, subovale, ben elevata e robusta, ricoperta da un periostraco lanuginoso che, sfumando verso l’apice, lo fa apparire glabro, così ri diritti i Tutti Mediterraneo” come si presentano gli esemplari giovanili. Scultura: marcate linee radiali che intersecando fitte ed irregolari linee concentriche danno forma ad una superficie simile all’intreccio dei panieri di vimini, obsoleta verso l’apice. Colore: castano ialino. Apice prominente ma piccolo, formante la spira di un solo giro, indifferentemente orientato, nei vari esemplari, a destra, a sinistra, o al centro e posizionato a circa 1/3 dal margine posteriore. I giovani hanno guscio più compresso e delicato con periostraco non lanuginoso. servati2007 © per i rispettiviproprietari. Vietatala duplicazion Dimensioni Lunghezza 4,00 /5,50 mm – larghezza 3,00/4,00 mm – altezza 1,20/2,50 mm. Area di distribuzione e habitat Mediterraneo intorno ai 450/500 metri, gli esemplari rinvenuti dal Rocchini erano presenti su trocheetti di legno e provenivano da fondali NO isola di Gorgona. Descrizione originale Riferimenti bibliografici R. Rocchini, Cocculina viminensis n.s. - Bollettino Malacologico – 26 (1990) – (1-4) – (47-52) – Milano 30/06/1990 Riferimenti on line http://www.cervia.com/conchigliedelmediterraneo/masterscheda.asp?nome=Coccopigya%20viminensis Comparazione Note Redattore Scheda di Claudio Giannobi aggiornata al 18/03/2007 e riproduzione senza espressa Riferimenti fotografici: Immagini non disponibili Foto 1 di autorizzazionescritta. -

Marine Shell-Bearing Gastropoda of Murman (Barents Sea): an Annotated Check-List
Ruthenica, 2014, vol. 24, No. 2: 75-121. © Ruthenica, 2014 Published online November 24, 2014. http: www.ruthenica.com Marine shell-bearing Gastropoda of Murman (Barents Sea): an annotated check-list Ivan O. NEKHAEV Murmansk Marine Biological Institute, Russian Academy of Sciences, Vladimirskaya str. 17, Murmansk 183010, Russia; [email protected] ABSTRACT. Annotated check-list of shell-bearing were placed close to Kola Peninsula [Derjugin, 1924]. Gastropoda of Murman Coast (Barents Sea Coast of Some samples of bottom fauna including Mollusca Kola Peninsula) is presented. Based on original materi- were collected along the Murman Coast by both al collected in 1996-2013 and literature data 148 species Helgoland expedition in 1898 and Poseidon expedi- are recorded for the region. Nine species: Skenea rugu- tion in 1913 [Thiele, 1928]. losa (G.O. Sars, 1878), Aclis sarsi Dautzenberg et Fis- Biological station in Dalnie Zelentsy village was cher, 1912, Admete clivicola Høisæter, 2010, Nassarius established after shutting of the research station in incrassatus (Strøm, 1768), Raphitoma leufroyi Ekaterinenskaya Bay in 1933. The first account of (Michaud, 1828), Taranis moerchi (Malm, 1861), Ondi- the fauna of the biological station vicinity (Yarnish- na divisa (J. Adams, 1797), Menestho albula (Fabri- naya, Dalne-Zelenetskaya and Porchnikha bays) was cius, 1780), Bogasonia volutoides Warén, 1989 were published by Ushakov [1948]. The general direction absent in previous reviews of Russian molluscan fau- na. Three species with unclear taxonomical position are of molluscan research during this period was com- listed: Skenea cf. trochoides, Omalogyra cf. atomus prehensive study of population ecology, life history, and Chrysallida sp. A majority of species found in breeding and in some cases embryonic develop- Murman waters have a boreal distribution and are typi- ment of common species [Kuznetsov, 1946; 1948a; cal for northern European fauna.